Ann Lab Med.
2012 May;32(3):229-233. 10.3343/alm.2012.32.3.229.
A Case of Imported Plasmodium malariae Malaria
- Affiliations
-
- 1Department of Laboratory Medicine, Seoul National University College of Medicine, Seoul, Korea. m91w95pf@snu.ac.kr
- 2Department of Laboratory Medicine, Seoul National University Bundang Hospital, Seongnam, Korea.
- 3Department of Internal Medicine, Seoul National University Bundang Hospital, Seongnam, Korea.
- KMID: 1381691
- DOI: http://doi.org/10.3343/alm.2012.32.3.229
Abstract
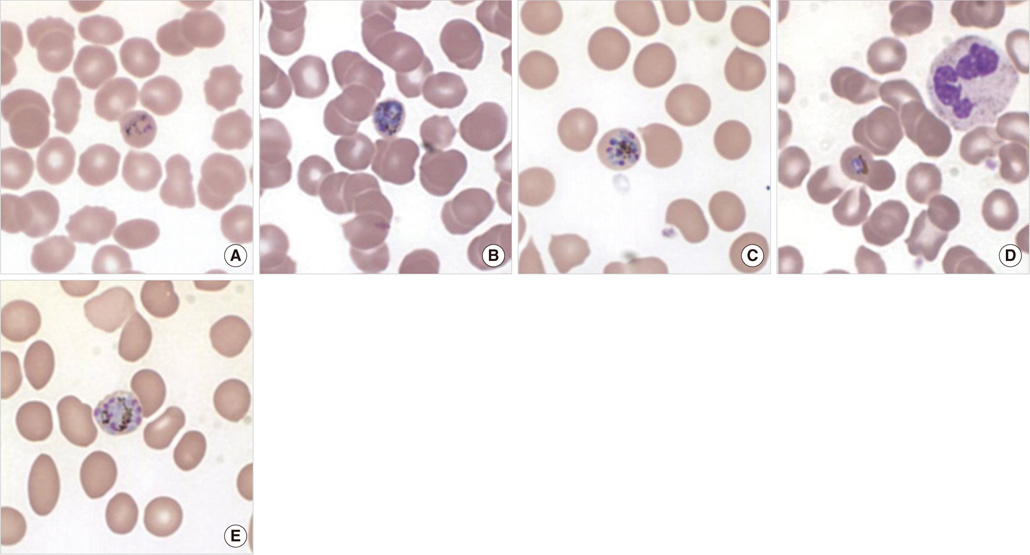
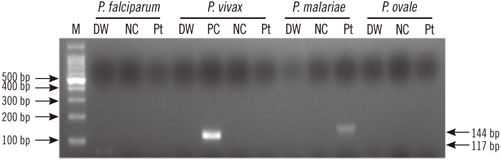
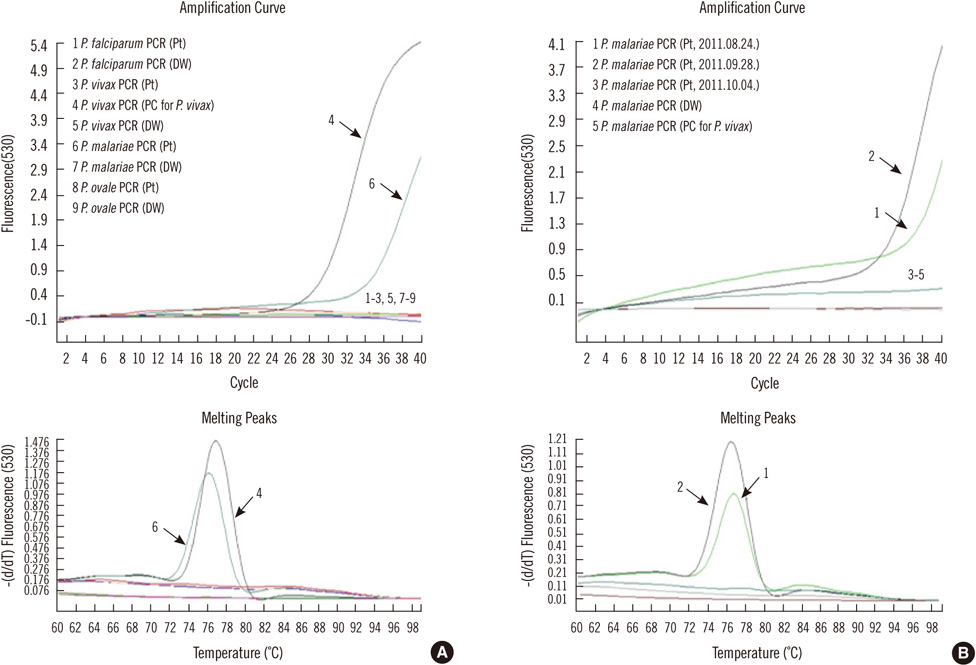
- Malaria, the most common vector-borne parasite infection worldwide, results from infection by Plasmodium species. Approximately 80% of malaria cases are caused by P. vivax, which is broadly distributed from tropical to temperate regions; P. falciparum is the second most common infectious species. P. malariae and P. ovale are responsible for a relatively small proportion of malaria cases. Here, we report the case of a 23-yr-old Korean woman who acquired a P. malariae infection while visiting the Republic of Ghana in West Africa for business. She was diagnosed with P. malariae malaria on the basis of peripheral blood smear (PBS) and species-specific conventional and real-time PCR assays for 18S rRNA. She was treated with hydroxychloroquine, and the resulting PBS examination on day 2 suggested that negative conversion occurred. At her 1-month follow-up, however, both the PBS examination and molecular test for malaria demonstrated recurrent parasitemia. We started rescue therapy with mefloquine, and the patient recovered successfully. This is an important finding suggesting possible late recrudescence of a chloroquine-resistant P. malariae strain identified not only by its morphological features, but also by molecular tests.
Keyword
MeSH Terms
Figure
Reference
-
1. Garcia LS. Malaria. Clin Lab Med. 2010. 30:93–129.
Article2. Breman JG. The ears of the hippopotamus: manifestations, determinants, and estimates of the malaria burden. Am J Trop Med Hyg. 2001. 64(1-2 Suppl):1–11.
Article3. Korea Centers for Disease Control and Prevention. last visited on Jan 2012. http://www.cdc.go.kr/kcdchome/jsp/diseasedic/dic/DISEDIC0001Detail.jsp?menuid=510264&contentid=8422&boardid=null&appid=kcdcdz01&pageNum=null&sub=null&tabinx=1&q_had01=A&q_had02=2011&idxType=0&idxNum=5.4. Whang CH. Induced malaria in Korea. Yonsei Med J. 1963. 4:51–57.
Article5. Kweon SH, Kim YS, Pai H, Park J, Park H, Choi MH, et al. A case of mixed infection with malaria and Babesia. Korean J Infect Dis. 1998. 30:198–202.6. Snounou G, Viriyakosol S, Zhu XP, Jarra W, Pinheiro L, do Rosario VE, et al. High sensitivity of detection of human malaria parasites by the use of nested polymerase chain reaction. Mol Biochem Parasitol. 1993. 61:315–320.
Article7. Ndao M, Bandyayera E, Kokoskin E, Gyorkos TW, MacLean JD, Ward BJ. Comparison of blood smear, antigen detection, and nested-PCR methods for screening refugees from regions where malaria is endemic after a malaria outbreak in Quebec, Canada. J Clin Microbiol. 2004. 42:2694–2700.
Article8. Cnops L, Jacobs J, Van Esbroeck M. Validation of a four-primer real-time PCR as a diagnostic tool for single and mixed Plasmodium infections. Clin Microbiol Infect. 2011. 17:1101–1107.9. Singh B, Kim Sung L, Matusop A, Radhakrishnan A, Shamsul SS, Cox-Singh J, et al. A large focus of naturally acquired Plasmodium knowlesi infections in human beings. Lancet. 2004. 363:1017–1024.10. Feachem RG, Phillips AA, Hwang J, Cotter C, Wielgosz B, Greenwood BM, et al. Shrinking the malaria map: progress and prospects. Lancet. 2010. 376:1566–1578.
Article11. Nzeyimana I, Henry MC, Dossou-Yovo J, Doannio JM, Diawara L, Carnevale P. The epidemiology of malaria in the southwestern forests of the Ivory Coast (Tai region). Bull Soc Pathol Exot. 2002. 95:89–94.12. World malaria report 2010. World Health Organization. Updated in 2012. Available at: http://www.who.int/malaria/world_malaria_report_2010/en/index.html.13. Warrell DA, Gilles HM, editors. Essential malariology. 2002. 4th ed. New York: Oxford University Press;192.14. WHO. Guidelines for the treatment of malaria. 2010. 2nd ed. Geneva: WHO.15. Collins WE, Jeffery GM. Plasmodium malariae: parasite and disease. Clin Microbiol Rev. 2007. 20:579–592.16. Kawamoto F, Liu Q, Ferreira MU, Tantular IS. How prevalent are Plasmodium ovale and P. malariae in East Asia? Parasitol Today. 1999. 15:422–426.17. Sulistyaningsih E, Fitri LE, Löscher T, Berens-Riha N. Diagnostic difficulties with Plasmodium knowlesi infection in humans. Emerg Infect Dis. 2010. 16:1033–1034.18. Maguire JD, Sumawinata IW, Masbar S, Laksana B, Prodjodipuro P, Susanti I, et al. Chloroquine-resistant Plasmodium malariae in south Sumatra, Indonesia. Lancet. 2002. 360:58–60.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Plasmodium malariae Infection Imported from Guinea
- Characteristics of Imported Malaria and Species of Plasmodium Involved in Shandong Province, China (2012-2014)
- Diagnosis and Molecular Analysis on Imported Plasmodium ovale curtisi and P. ovale wallikeri Malaria Cases from West and South Africa during 2013-2016
- Four Cases of The Imported Falciparum Malaria in Children
- Malaria