Korean J Radiol.
2012 Apr;13(2):189-194. 10.3348/kjr.2012.13.2.189.
Alternative Techniques for Cannulation of Biliary Strictures Resistant to the 0.035" System Following Living Donor Liver Transplantation
- Affiliations
-
- 1Department of Radiology and Research Institute of Radiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul 138-736, Korea. m1fenew@daum.net
- KMID: 1245383
- DOI: http://doi.org/10.3348/kjr.2012.13.2.189
Abstract
OBJECTIVE
To assess the clinical efficacy of alternative techniques for biliary stricture cannulation in patients undergoing living donor liver transplantation (LDLT), after cannulation failure with a conventional (0.035-inch guidewire) technique.
SUBJECTS AND METHODS
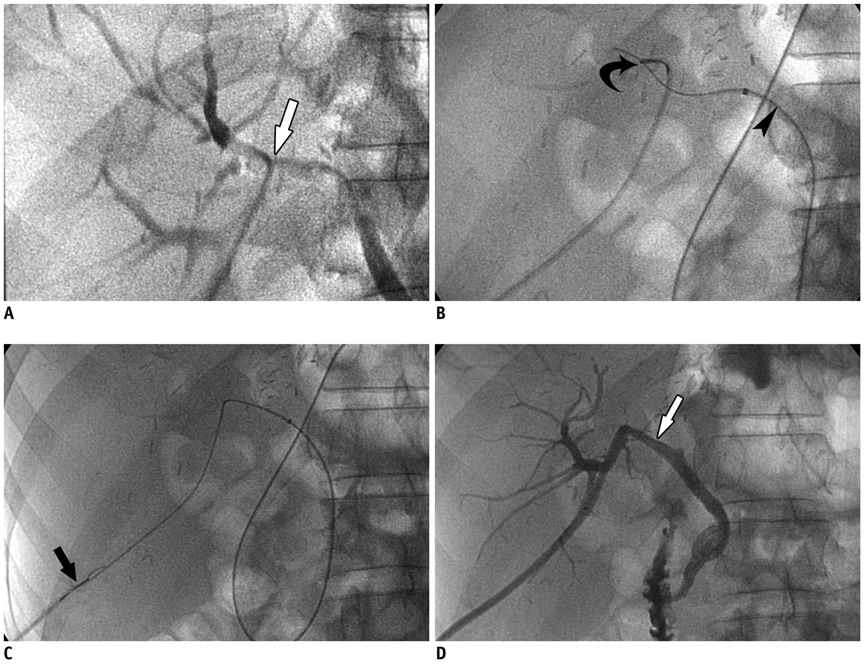
Of 293 patients with biliary strictures after LDLT, 19 (6%) patients, 11 men and 8 women of mean age 48.5 years, had the failed cannulation of the stricture by conventional techniques. Recannulation was attempted by using two alternative methods, namely a micro-catheter set via percutaneous access and a snare (rendezvous) technique using percutaneous and endoscopic approaches.
RESULTS
Strictures were successfully cannulated in 16 (84%) of the 19 patients. A microcatheter set was used in 12 and a snare technique in four patients. Stricture cannulation failed in the remaining three patients, who finally underwent surgical revision.
CONCLUSION
Most technical failures using a conventional technique for biliary stricture cannulation after LDLT can be overcome by using a microcatheter set or a snare (rendezvous) technique.
MeSH Terms
Figure
Reference
-
1. Chang JH, Lee IS, Chun HJ, Choi JY, Yoon SK, Kim DG, et al. Usefulness of the rendezvous technique for biliary stricture after adult right-lobe living-donor liver transplantation with duct-to-duct anastomosis. Gut Liver. 2010. 4:68–75.2. Kim JH, Ko GY, Sung KB, Yoon HK, Gwon DI, Kim KR, et al. Bile leak following living donor liver transplantation: clinical efficacy of percutaneous transhepatic treatment. Liver Transpl. 2008. 14:1142–1149.3. Choo SW, Shin SW, Do YS, Liu WC, Park KB, Sung YM, et al. The balloon dilatation and large profile catheter maintenance method for the management of the bile duct stricture following liver transplantation. Korean J Radiol. 2006. 7:41–49.4. Moser MA, Wall WJ. Management of biliary problems after liver transplantation. Liver Transpl. 2001. 7:S46–S52.5. Ramacciato G, Varotti G, Quintini C, Masetti M, Di Benedetto F, Grazi GL, et al. Impact of biliary complications in right lobe living donor liver transplantation. Transpl Int. 2006. 19:122–127.6. Yazumi S, Chiba T. Biliary complications after a right-lobe living donor liver transplantation. J Gastroenterol. 2005. 40:861–865.7. Kasahara M, Egawa H, Takada Y, Oike F, Sakamoto S, Kiuchi T, et al. Biliary reconstruction in right lobe living-donor liver transplantation: comparison of different techniques in 321 recipients. Ann Surg. 2006. 243:559–566.8. Hwang S, Lee SG, Sung KB, Park KM, Kim KH, Ahn CS, et al. Long-term incidence, risk factors, and management of biliary complications after adult living donor liver transplantation. Liver Transpl. 2006. 12:831–838.9. Chang JM, Lee JM, Suh KS, Yi NJ, Kim YT, Kim SH, et al. Biliary complications in living donor liver transplantation: imaging findings and the roles of interventional procedures. Cardiovasc Intervent Radiol. 2005. 28:756–767.10. Yazumi S, Yoshimoto T, Hisatsune H, Hasegawa K, Kida M, Tada S, et al. Endoscopic treatment of biliary complications after right-lobe living-donor liver transplantation with duct-to-duct biliary anastomosis. J Hepatobiliary Pancreat Surg. 2006. 13:502–510.11. Shah JN, Ahmad NA, Shetty K, Kochman ML, Long WB, Brensinger CM, et al. Endoscopic management of biliary complications after adult living donor liver transplantation. Am J Gastroenterol. 2004. 99:1291–1295.12. Verdonk RC, Buis CI, Porte RJ, van der Jagt EJ, Limburg AJ, van den Berg AP, et al. Anastomotic biliary strictures after liver transplantation: causes and consequences. Liver Transpl. 2006. 12:726–735.13. Park JS, Kim MH, Lee SK, Seo DW, Lee SS, Han J, et al. Efficacy of endoscopic and percutaneous treatments for biliary complications after cadaveric and living donor liver transplantation. Gastrointest Endosc. 2003. 57:78–85.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Unilateral Versus Bilateral Biliary Drainage for Post-Transplant Anastomotic Stricture
- Biliary Strictures after Liver Transplantation
- Anatomical limits in living donor liver transplantation
- The Application of Interventional Radiology in Living-Donor Liver Transplantation
- Endoscopic management of anastomotic stricture after living-donor liver transplantation