Korean J Ophthalmol.
2012 Feb;26(1):15-20. 10.3341/kjo.2012.26.1.15.
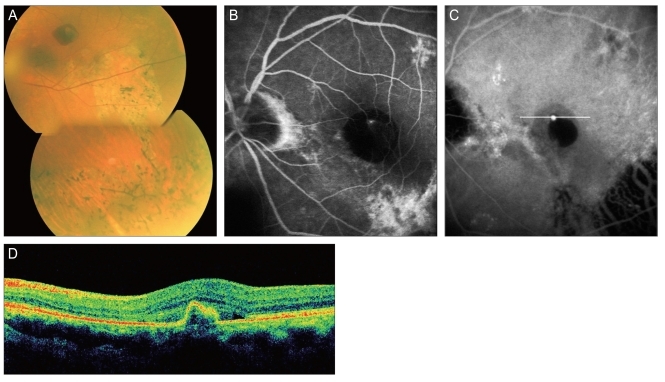
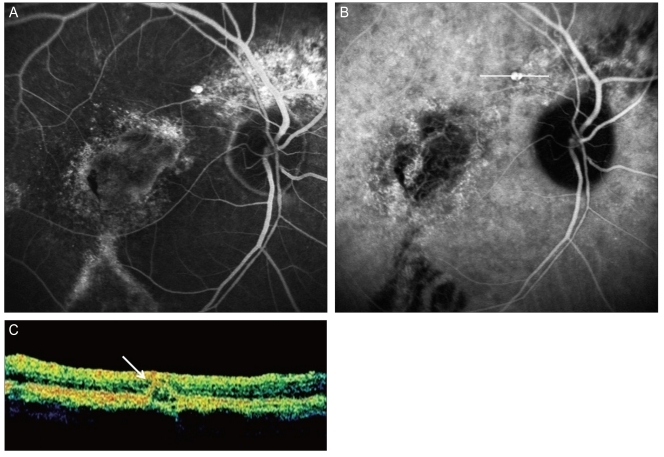
Clinical Characteristics of Polypoidal Choroidal Vasculopathy Associated with Chronic Central Serous Chorioretionopathy
- Affiliations
-
- 1Department of Ophthalmology, Kyungpook National University Hospital, Daegu, Korea. itkim@knu.ac.kr
- KMID: 1120176
- DOI: http://doi.org/10.3341/kjo.2012.26.1.15
Abstract
- PURPOSE
To investigate the clinical characteristics of polypoidal choroidal vasculopathy (PCV) associated with chronic central serous chorioretinopathy (CSC).
METHODS
We retrospectively reviewed the medical records of 246 PCV patients (283 eyes) between July 2004 and August 2009 and investigated the clinical characteristics of the PCV patients who had specific fundus findings of chronic CSC.
RESULTS
Among PCV patients, 13 eyes (4.6%) of 13 PCV patients (5.3%) had fundus findings of chronic CSC. All of the PCV lesions had a solitary polyp located outside the atrophic retina, predominantly in the macular area (84.6%), most showed an exudative pattern (69.2%) and there were a few that showed a hemorrhagic pattern (30.8%). All of the lesions were smaller than 1 disc diameter. Most of the PCV lesions (76.9%) were cured with less than two treatments in a short period of 6.4 +/- 1.9 months; however, visual acuity deteriorated (61.5%) or was not changed (30.8%) in most of the cases.
CONCLUSIONS
The PCV associated with chronic CSC had several clinical features such as a small exudative retinal lesion with a solitary polyp and frequent involvement of the macular area. Even though there was poor visual outcome due to the atrophic change, all of the PCV lesions were easily resolved in a short period with a simple treatment course and no recurrence.
Keyword
MeSH Terms
-
Aged
Choroid/*blood supply
Choroid Diseases/*complications/diagnosis/therapy
Female
Fluorescein Angiography
Humans
Indocyanine Green/diagnostic use
Male
Middle Aged
Retinal Detachment/complications/diagnosis/therapy
Retinal Diseases/*complications/diagnosis/therapy
Retrospective Studies
Risk Factors
Visual Acuity
Figure
Reference
-
1. Hayashi K, Hasegawa Y, Tokoro T. Indocyanine green angiography of central serous chorioretinopathy. Int Ophthalmol. 1986; 9:37–41. PMID: 3721709.
Article2. Scheider A, Nasemann JE, Lund OE. Fluorescein and indocyanine green angiographies of central serous choroidopathy by scanning laser ophthalmoscopy. Am J Ophthalmol. 1993; 115:50–56. PMID: 8420378.
Article3. Piccolino FC, Borgia L. Central serous chorioretinopathy and indocyanine green angiography. Retina. 1994; 14:231–242. PMID: 7973118.
Article4. Guyer DR, Yannuzzi LA, Slakter JS, et al. Digital indocyanine green videoangiography of central serous chorioretinopathy. Arch Ophthalmol. 1994; 112:1057–1062. PMID: 8053819.
Article5. Piccolino FC, Borgia L, Zinicola E, Zingirian M. Indocyanine green angiographic findings in central serous chorioretinopathy. Eye (Lond). 1995; 9(Pt 3):324–332. PMID: 7556741.
Article6. Spaide RF, Hall L, Haas A, et al. Indocyanine green videoangiography of older patients with central serous chorioretinopathy. Retina. 1996; 16:203–213. PMID: 8789858.
Article7. Prünte C, Flammer J. Choroidal capillary and venous congestion in central serous chorioretinopathy. Am J Ophthalmol. 1996; 121:26–34. PMID: 8554078.8. Menchini U, Virgili G, Lanzetta P, Ferrari E. Indocyanine green angiography in central serous chorioretinopathy. ICG angiography in CSC. Int Ophthalmol. 1997; 21:57–69. PMID: 9405986.9. Yannuzzi LA, Shakin JL, Fisher YL, Altomonte MA. Peripheral retinal detachments and retinal pigment epithelial atrophic tracts secondary to central serous pigment epitheliopathy. Ophthalmology. 1984; 91:1554–1572. PMID: 6084221.
Article10. Yannuzzi LA, Slakter JS, Kaufman SR, Gupta K. Laser treatment of diffuse retinal pigment epitheliopathy. Eur J Ophthalmol. 1992; 2:103–114. PMID: 1450655.
Article11. Castro-Correia J, Coutinho MF, Rosas V, Maia J. Long-term follow-up of central serous retinopathy in 150 patients. Doc Ophthalmol. 1992; 81:379–386. PMID: 1486812.
Article12. Spaide RF, Campeas L, Haas A, et al. Central serous chorioretinopathy in younger and older adults. Ophthalmology. 1996; 103:2070–2079. PMID: 9003341.
Article13. Spraul CW, Lang GE, Lang GK. Retinal pigment epithelial changes associated with systemic corticosteroid treatment: report of cases and review of the literature. Ophthalmologica. 1998; 212:142–148. PMID: 9486556.
Article14. Bujarborua D. Long-term follow-up of idiopathic central serous chorioretinopathy without laser. Acta Ophthalmol Scand. 2001; 79:417–421. PMID: 11453866.
Article15. Otsuka S, Ohba N, Nakao K. A long-term follow-up study of severe variant of central serous chorioretinopathy. Retina. 2002; 22:25–32. PMID: 11884874.
Article16. Maruko I, Iida T, Saito M, et al. Clinical characteristics of exudative age-related macular degeneration in Japanese patients. Am J Ophthalmol. 2007; 144:15–22. PMID: 17509509.
Article17. Byeon SH, Lee SC, Oh HS, et al. Incidence and clinical patterns of polypoidal choroidal vasculopathy in Korean patients. Jpn J Ophthalmol. 2008; 52:57–62. PMID: 18369702.
Article18. Wen F, Chen C, Wu D, Li H. Polypoidal choroidal vasculopathy in elderly Chinese patients. Graefes Arch Clin Exp Ophthalmol. 2004; 242:625–629. PMID: 15257461.
Article19. Yuzawa M, Mori R, Kawamura A. The origins of polypoidal choroidal vasculopathy. Br J Ophthalmol. 2005; 89:602–607. PMID: 15834093.
Article20. Sasahara M, Tsujikawa A, Musashi K, et al. Polypoidal choroidal vasculopathy with choroidal vascular hyperpermeability. Am J Ophthalmol. 2006; 142:601–607. PMID: 17011852.
Article21. Ueta T, Obata R, Inoue Y, et al. Background comparison of typical age-related macular degeneration and polypoidal choroidal vasculopathy in Japanese patients. Ophthalmology. 2009; 116:2400–2406. PMID: 19815291.
Article22. Uyama M, Wada M, Nagai Y, et al. Polypoidal choroidal vasculopathy: natural history. Am J Ophthalmol. 2002; 133:639–648. PMID: 11992861.23. Nakashizuka H, Mitsumata M, Okisaka S, et al. Clinicopathologic findings in polypoidal choroidal vasculopathy. Invest Ophthalmol Vis Sci. 2008; 49:4729–4737. PMID: 18586873.
Article24. Ahuja RM, Downes SM, Stanga PE, et al. Polypoidal choroidal vasculopathy and central serous chorioretinopathy. Ophthalmology. 2001; 108:1009–1010. PMID: 11382610.
Article25. Lee JW, Kim IT. Epidemiologic and clinical characteristics of polypoidal choroidal vasculopathy in Korean patients. J Korean Ophthalmol Soc. 2007; 48:63–74.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Epidemiologic and Clinical Characteristics of Polypoidal Choroidal Vasculopathy in Korean Patients
- Choroidal Venous Pulsations at an Arterio-venous Crossing in Polypoidal Choroidal Vasculopathy
- Photodynamic Therapy with Verteporfin in Polypoidal Choroidal Vasculopathy
- A Case of Polypoidal Choroidal Vasculopathy and Serous Retinal Detachment in a Bilateral Dome-shaped Macula
- Initial Factors Associated with Resistance to Intravitreal Aflibercept Injection in Polypoidal Choroidal Vasculopathy