Korean J Ophthalmol.
2013 Oct;27(5):384-387. 10.3341/kjo.2013.27.5.384.
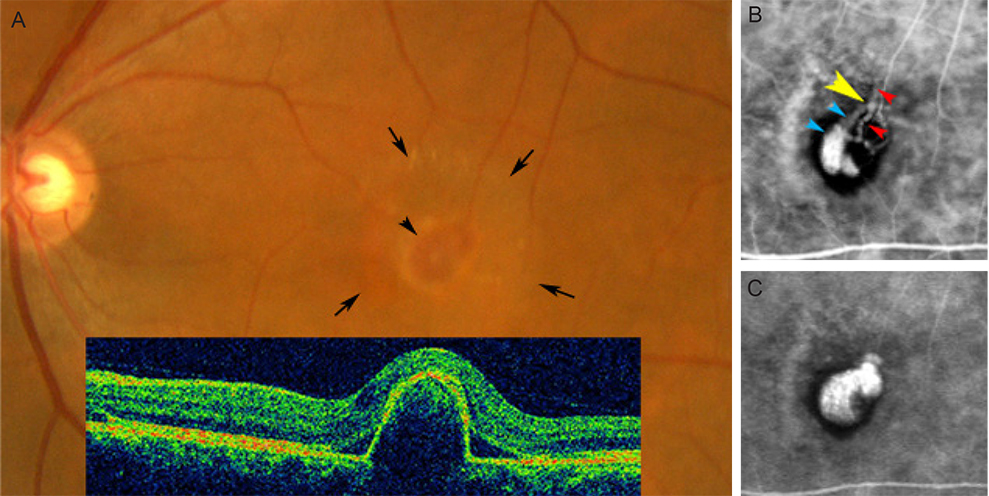
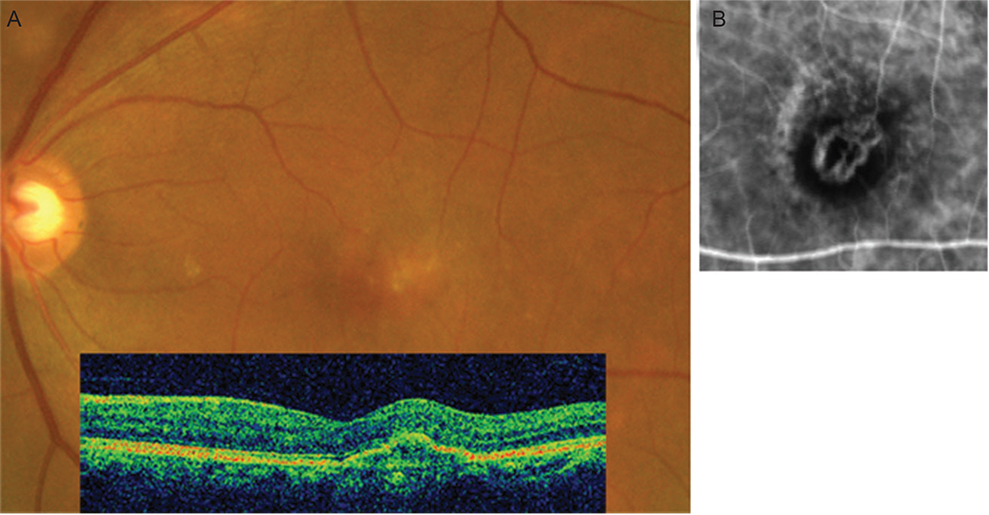
Choroidal Venous Pulsations at an Arterio-venous Crossing in Polypoidal Choroidal Vasculopathy
- Affiliations
-
- 1Unoki Eye Clinic, Kagoshima, Japan. akiko@m2.kufm.kagoshima-u.ac.jp
- 2Department of Ophthalmology, Kagoshima University Graduate School of Medical and Dental Sciences, Kagoshima, Japan.
- KMID: 1707295
- DOI: http://doi.org/10.3341/kjo.2013.27.5.384
Abstract
- It has been reported that pulsations in abnormal vessels are observed on indocyanine green (ICG) angiography in half of patients with polypoidal choroidal vasculopathy (PCV), although the mechanism of the pulsation is unknown. In this study, we report a case of PCV showing venous pulsations at an arterio-venous (A-V) crossing, and discuss a possible mechanism of polypoidal vessel formation and pulsations in PCV. A 66-year-old female presented with a reddish-orange elevated lesion and serous retinal detachment in the macula of her left eye, and was diagnosed as PCV. She was treated with photodynamic therapy (PDT), and followed-up through routine examinations, including ICG angiography. ICG angiography at presentation showed a branching vascular network and choroidal venules with dye leakage (polypoidal vessels) in the left eye. Pulsations, supposedly of venous origin, were observed at an A-V crossing in the abnormal vessels. Within 3 months after PDT, the polypoidal vessel ceased to leak and the pulsations vanished. The reddish-orange lesion gradually decreased in size with complete disappearance of retinal detachment. This study suggests that an unusual compression at an A-V crossing may make a venule polypoidal, and fluctuations of blood flow and pressure in the venule may cause pulsatile movements of the vessel wall.
Keyword
MeSH Terms
Figure
Reference
-
1. Yuzawa M, Mori R, Kawamura A. The origins of polypoidal choroidal vasculopathy. Br J Ophthalmol. 2005; 89:602–607.2. Okubo A, Ito M, Sameshima M, et al. Pulsatile blood flow in the polypoidal choroidal vasculopathy. Ophthalmology. 2005; 112:1436–1441.3. Levine DN. Spontaneous pulsation of the retinal veins. Microvasc Res. 1998; 56:154–165.4. Jacks AS, Miller NR. Spontaneous retinal venous pulsation: aetiology and significance. J Neurol Neurosurg Psychiatry. 2003; 74:7–9.5. Frangieh GT, Green WR, Barraquer-Somers E, Finkelstein D. Histopathologic study of nine branch retinal vein occlusions. Arch Ophthalmol. 1982; 100:1132–1140.6. Kuroiwa S, Tateiwa H, Hisatomi T. Pathological features of surgically excised polypoidal choroidal vasculopathy membranes. Clin Experiment Ophthalmol. 2004; 32:297–302.7. Okubo A, Sameshima M, Uemura A, et al. Clinicopathological correlation of polypoidal choroidal vasculopathy revealed by ultrastructural study. Br J Ophthalmol. 2002; 86:1093–1098.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Photodynamic Therapy with Verteporfin in Polypoidal Choroidal Vasculopathy
- The Variants of Macular Choroidal Veins in ICG Angiography
- Peripapillary Choroidal Thickness Change of Polypoidal Choroidal Vasculopathy after Anti-vascular Endothelial Growth Factor
- Changes of Network Vessels after Photodynamic Therapy in Polypoidal Choroidal Vasculopathy
- polypoidal Choroidal Vasculopathy