Korean J Ophthalmol.
2011 Apr;25(2):84-89. 10.3341/kjo.2011.25.2.84.
Clinical Characteristics and Outcomes of Cataract Surgery in Highly Myopic Koreans
- Affiliations
-
- 1Department of Ophthalmology, St. Mary's Hospital, The Catholic University of Korea School of Medicine, Seoul, Korea. sara514@catholic.ac.kr
- KMID: 1111868
- DOI: http://doi.org/10.3341/kjo.2011.25.2.84
Abstract
- PURPOSE
To evaluate the clinical characteristics and outcomes of cataract surgery in highly myopic Korean subjects.
METHODS
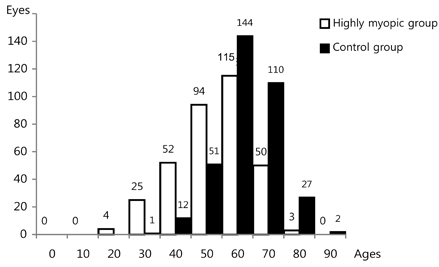
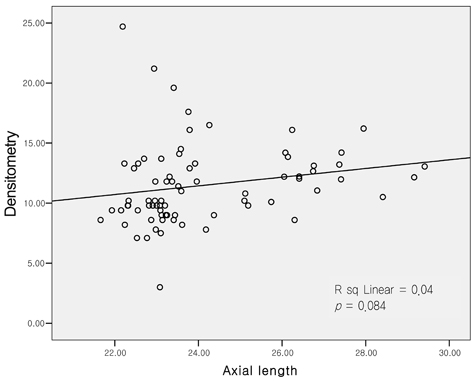
We retrospectively reviewed the medical records of 694 eyes of 694 patients who underwent cataract surgery. The case group included 347 eyes of 347 patients whose axial lengths (AXL) were > or =26.00 mm, and the control group included 347 eyes of 347 patients with AXL between 22.00 and 25.99 mm. Cataract density was determined preoperatively using the Pentacam Scheimpflug imaging system. We compared age at operation, cataract type, coexisting disease, visual prognosis, and complications.
RESULTS
The mean age at the time of the operation was 59.60 +/- 12.28 years in the case group and 67.47 +/- 11.36 years in the control group. The case group had a larger proportion of nuclear cataracts and posterior subcapsular cataracts (PSC), 40.63% and 26.22%, respectively, versus 25.07% and 11.82%, respectively, in the control group. Postoperative corrected visual acuity showed a negative correlation with AXL (R2 = 0.172), and severe funduscopic findings were related to poor visual prognosis (p = 0.05). The incidence of retinal detachment in the case group after cataract surgery was 1.72%, compared with 0.28% in the control group.
CONCLUSIONS
Highly myopic eyes tend to develop cataracts earlier than normal eyes and to have a higher prevalence of coexisting disease and complications, such as retinal detachment. Nuclear cataracts and PSC were more common in the highly myopic group. Poor visual prognosis was associated with longer axial length and retinal myopic degeneration.
Keyword
MeSH Terms
-
Aged
*Asian Continental Ancestry Group
Cataract/*complications/epidemiology/physiopathology
*Cataract Extraction
Female
Follow-Up Studies
Humans
Male
Middle Aged
Myopia/*complications/epidemiology/physiopathology
Postoperative Period
*Refraction, Ocular
Republic of Korea/epidemiology
Retrospective Studies
*Visual Acuity
Figure
Cited by 2 articles
-
Axial Length Change after Implantable Collamer Lens Implantation
Ju Yong Seok, Damho Lee, Haksu Kyung, Joon Mo Kim
J Korean Ophthalmol Soc. 2013;54(11):1675-1679. doi: 10.3341/jkos.2013.54.11.1675.Risk Factors for Cataract Formation after Implantable Collamer Lens Implantation: Over a Mean 7.5-Year Follow-Up Period
Damho Lee, Ju Yong Seok, Hak Su Kyung, Joon Mo Kim
J Korean Ophthalmol Soc. 2015;56(6):835-846. doi: 10.3341/jkos.2015.56.6.835.
Reference
-
1. Wang TJ, Chiang TH, Wang TH, et al. Changes of the ocular refraction among freshmen in National Taiwan University between 1988 and 2005. Eye (Lond). 2009. 23:1168–1169.2. Lee SJ, Kim JM, Yu BC, et al. Prevalence of myopia in 19-year-old men in gyeongsangnam-do, Ulsan and Busan in 2002. J Korean Ophthalmol Soc. 2009. 50:1392–1403.3. Hyung SM, Kim DM, Hong C, Youn DH. Optic disc of the myopic eye: relationship between refractive errors and morphometric characteristics. Korean J Ophthalmol. 1992. 6:32–35.4. Suzuki Y, Iwase A, Araie M, et al. Risk factors for open-angle glaucoma in a Japanese population: the Tajimi Study. Ophthalmology. 2006. 113:1613–1617.5. Mayama C, Suzuki Y, Araie M, et al. Myopia and advanced-stage open-angle glaucoma. Ophthalmology. 2002. 109:2072–2077.6. Lee YA, Shih YF, Lin LL, et al. Association between high myopia and progression of visual field loss in primary open-angle glaucoma. J Formos Med Assoc. 2008. 107:952–957.7. Perkins ES. Cataract: refractive error, diabetes, and morphology. Br J Ophthalmol. 1984. 68:293–297.8. Weale R. A note on a possible relation between refraction and a disposition for senile nuclear cataract. Br J Ophthalmol. 1980. 64:311–314.9. Brown NA, Hill AR. Cataract: the relation between myopia and cataract morphology. Br J Ophthalmol. 1987. 71:405–414.10. Praveen MR, Shah GD, Vasavada AR, et al. A study to explore the risk factors for the early onset of cataract in India. Eye (Lond). 2010. 24:686–694.11. Lim R, Mitchell P, Cumming RG. Refractive associations with cataract: the Blue Mountains Eye Study. Invest Ophthalmol Vis Sci. 1999. 40:3021–3026.12. Wong TY, Klein BE, Klein R, et al. Refractive errors and incident cataracts: the Beaver Dam Eye Study. Invest Ophthalmol Vis Sci. 2001. 42:1449–1454.13. Tosi GM, Casprini F, Malandrini A, et al. Phacoemulsification without intraocular lens implantation in patients with high myopia: long-term results. J Cataract Refract Surg. 2003. 29:1127–1131.14. Mehdizadeh M, Ashraf H. Prevalence of cataract type in relation to axial length in subjects with high myopia and emmetropia in an Indian population. Am J Ophthalmol. 2008. 146:329–330.15. Chen SN, Lin KK, Chao AN, et al. Nuclear sclerotic cataract in young patients in Taiwan. J Cataract Refract Surg. 2003. 29:983–988.16. Kirkwood BJ, Hendicott PL, Read SA, Pesudovs K. Repeatability and validity of lens densitometry measured with Scheimpflug imaging. J Cataract Refract Surg. 2009. 35:1210–1215.17. Kim JS, Chung SH, Joo CK. Clinical application of a Scheimpflug system for lens density measurements in phacoemulsification. J Cataract Refract Surg. 2009. 35:1204–1209.18. Tsai CY, Chang TJ, Kuo LL, et al. Visual outcomes and associated risk factors of cataract surgeries in highly myopic Taiwanese. Ophthalmologica. 2008. 222:130–135.19. Fernandez-Vega L, Alfonso JF, Villacampa T. Clear lens extraction for the correction of high myopia. Ophthalmology. 2003. 110:2349–2354.20. Kubaloglu A, Yazicioglu T, Tacer S. Small incision clear lens extraction for correction of high myopia. Eur J Ophthalmol. 2004. 14:1–6.21. Pucci V, Morselli S, Romanelli F, et al. Clear lens phacoemulsification for correction of high myopia. J Cataract Refract Surg. 2001. 27:896–900.22. Lee KH, Lee JH. Long-term results of clear lens extraction for severe myopia. J Cataract Refract Surg. 1996. 22:1411–1415.23. Ripandelli G, Scassa C, Parisi V, et al. Cataract surgery as a risk factor for retinal detachment in very highly myopic eyes. Ophthalmology. 2003. 110:2355–2361.24. Ravalico G, Michieli C, Vattovani O, Tognetto D. Retinal detachment after cataract extraction and refractive lens exchange in highly myopic patients. J Cataract Refract Surg. 2003. 29:39–44.25. Jacobi FK, Hessemer V. Pseudophakic retinal detachment in high axial myopia. J Cataract Refract Surg. 1997. 23:1095–1102.26. Colin J, Robinet A, Cochener B. Retinal detachment after clear lens extraction for high myopia: seven-year follow-up. Ophthalmology. 1999. 106:2281–2284.27. Alio JL, Ruiz-Moreno JM, Shabayek MH, et al. The risk of retinal detachment in high myopia after small incision coaxial phacoemulsification. Am J Ophthalmol. 2007. 144:93–98.28. Chylack LT Jr, Wolfe JK, Singer DM, et al. The Longitudinal Study of Cataract Study Group. The Lens Opacities Classification System III. Arch Ophthalmol. 1993. 111:831–836.29. Micelli-Ferrari T, Vendemiale G, Grattagliano I, et al. Role of lipid peroxidation in the pathogenesis of myopic and senile cataract. Br J Ophthalmol. 1996. 80:840–843.30. Zigler JS Jr, Bodaness RS, Gery I, Kinoshita JH. Effects of lipid peroxidation products on the rat lens in organ culture: a possible mechanism of cataract initiation in retinal degenerative disease. Arch Biochem Biophys. 1983. 225:149–156.31. Klein BE, Klein R, Linton KL, et al. Assessment of cataracts from photographs in the Beaver Dam Eye Study. Ophthalmology. 1990. 97:1428–1433.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Outcome of Minus Diopter Posterior Chamber Lens
- The Refractive Change After Cataract Surgery in Patients With Acute Primary Angle Closure
- Clinical Evaluation of Accommodative Intraocular Lens Implantation in High Myopic Eyes
- Myopic Shift after Implantation of a Novel Diffractive Trifocal Intraocular Lens in Korean Eyes
- Myopic Shift and Cataract Change after Lens Sparing Vitrectomy in Patients with Idiopathic Epiretinal Membrane in Their 5th and 6th Decade