Korean J Ophthalmol.
2018 Feb;32(1):16-22. 10.3341/kjo.2017.0060.
Myopic Shift after Implantation of a Novel Diffractive Trifocal Intraocular Lens in Korean Eyes
- Affiliations
-
- 1Department of Ophthalmology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. tychung@skku.edu
- 2Department of Preventive Medicine, Catholic University School of Medicine, Seoul, Korea.
- 3Department of Ophthalmology, Saevit Eye Hospital, Goyang, Korea.
- 4Department of Ophthalmology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 2402715
- DOI: http://doi.org/10.3341/kjo.2017.0060
Abstract
- PURPOSE
To evaluate the clinical outcomes of cataract surgery using novel diffractive trifocal intraocular lenses (IOLs) in Koreans.
METHODS
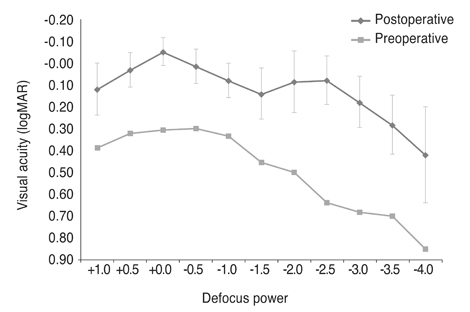
This was a retrospective, consecutive, interventional study of cataract surgery using POD FineVision IOL implantation. Complete ophthalmologic examinations were performed preoperatively and postoperatively. Defocus curves were assessed over a range of +1.5 to −4.0 diopters in 0.5-diopter steps at one month postoperatively. Uncorrected distant visual acuity, uncorrected intermediate visual acuity, uncorrected near visual acuity, corrected distant visual acuity, distant-corrected intermediate visual acuity, and distant-corrected near visual acuity were assessed one month postoperatively, and manifest refraction was performed during every visit.
RESULTS
The study analyzed 31 eyes in 20 patients. There were statistically significant improvements in uncorrected distance visual acuity, uncorrected intermediate visual acuity, uncorrected near visual acuity, corrected distance visual acuity, distance-corrected intermediate visual acuity, and distance-corrected near visual acuity (p < 0.001). The final postoperative refractive outcomes showed statistically significant myopic shifts compared to the target refraction based on SRK/T, SRK-II, Haigis, and Hoffer Q formulas (p < 0.001).
CONCLUSIONS
POD FineVision IOLs provide stable visual restoration with improvements of near and intermediate vision in presbyopic eyes. POD FineVision IOLs show myopic shift in a Korean population; therefore, surgeons should be cautious when selecting IOL power in such patients.
MeSH Terms
Figure
Reference
-
1. Agresta B, Knorz MC, Kohnen T, et al. Distance and near visual acuity improvement after implantation of multifocal intraocular lenses in cataract patients with presbyopia: a systematic review. J Refract Surg. 2012; 28:426–435.
Article2. Mesci C, Erbil H, Ozdoker L, et al. Visual acuity and contrast sensitivity function after accommodative and multifocal intraocular lens implantation. Eur J Ophthalmol. 2010; 20:90–100.
Article3. Calladine D, Evans JR, Shah S, Leyland M. Multifocal versus monofocal intraocular lenses after cataract extraction. Cochrane Database Syst Rev. 2012; (9):CD003169.
Article4. Cochener B, Lafuma A, Khoshnood B, et al. Comparison of outcomes with multifocal intraocular lenses: a meta-analysis. Clin Ophthalmol. 2011; 5:45–56.5. Hutz WW, Eckhardt HB, Rohrig B, Grolmus R. Intermediate vision and reading speed with array, Tecnis, and ReSTOR intraocular lenses. J Refract Surg. 2008; 24:251–256.
Article6. Jonker SM, Bauer NJ, Makhotkina NY, et al. Comparison of a trifocal intraocular lens with a ‡3.0 D bifocal IOL: results of a prospective randomized clinical trial. J Cataract Refract Surg. 2015; 41:1631–1640.
Article7. Cochener B. Prospective clinical comparison of patient outcomes following implantation of trifocal or bifocal intraocular lenses. J Refract Surg. 2016; 32:146–151.
Article8. Alio JL, Montalban R, Pena-Garcia P, et al. Visual outcomes of a trifocal aspheric diffractive intraocular lens with microincision cataract surgery. J Refract Surg. 2013; 29:756–761.
Article9. Cochener B, Vryghem J, Rozot P, et al. Clinical outcomes with a trifocal intraocular lens: a multicenter study. J Refract Surg. 2014; 30:762–768.
Article10. Marques EF, Ferreira TB. Comparison of visual outcomes of 2 diffractive trifocal intraocular lenses. J Cataract Refract Surg. 2015; 41:354–363.
Article11. Mendicute J, Kapp A, Levy P, et al. Evaluation of visual outcomes and patient satisfaction after implantation of a diffractive trifocal intraocular lens. J Cataract Refract Surg. 2016; 42:203–210.
Article12. Mojzis P, Pena-Garcia P, Liehneova I, et al. Outcomes of a new diffractive trifocal intraocular lens. J Cataract Refract Surg. 2014; 40:60–69.
Article13. Sheppard AL, Shah S, Bhatt U, et al. Visual outcomes and subjective experience after bilateral implantation of a new diffractive trifocal intraocular lens. J Cataract Refract Surg. 2013; 39:343–349.
Article14. Vryghem JC, Heireman S. Visual performance after the implantation of a new trifocal intraocular lens. Clin Ophthalmol. 2013; 7:1957–1965.
Article15. Poyales F, Garzon N, Rozema JJ, et al. Stability of a novel intraocular lens design: comparison of two trifocal lenses. J Refract Surg. 2016; 32:394–402.
Article16. Kwon YK, Kim HK, Lee JH. Clinical outcomes of diffractive trifocal intraocular lens in both eyes: a 6-month follow-up. J Korean Ophthalmol Soc. 2015; 56:1331–1337.
Article17. Aristodemou P, Knox Cartwright NE, et al. Intraocular lens formula constant optimization and partial coherence interferometry biometry: refractive outcomes in 8108 eyes after cataract surgery. J Cataract Refract Surg. 2011; 37:50–62.
Article18. Olsen T. Improved accuracy of intraocular lens power calculation with the Zeiss IOLMaster. Acta Ophthalmol Scand. 2007; 85:84–87.
Article19. User Group for Laser Interference Biometry. Zeiss IOL-Master [Internet]. [place unknown]: User Group for Laser Interference Biometry;2016. cited 2016 Apr 24. Available from: http://ocusoft.de/ulib/c1.htm.20. Qin B, Tang M, Li Y, et al. Anterior segment dimensions in Asian and Caucasian eyes measured by optical coherence tomography. Ophthalmic Surg Lasers Imaging. 2012; 43:135–142.
Article21. Wang YE, Li Y, Wang D, et al. Comparison of factors associated with occludable angle between american Caucasians and ethnic Chinese. Invest Ophthalmol Vis Sci. 2013; 54:7717–7723.
Article22. Sheard R. Optimising biometry for best outcomes in cataract surgery. Eye (Lond). 2014; 28:118–125.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of the Visual Outcomes after Cataract Surgery with Implantation of a Bifocal and Trifocal Diffractive Intraocular Lens
- Trifocal versus Bifocal Diffractive Intraocular Lens Implantation after Cataract Surgery or Refractive Lens Exchange: a Meta-analysis
- Clinical Outcomes of Diffractive Aspheric Trifocal Intraocular Lens Implantation
- Effects of Bifocal versus Trifocal Diffractive Intraocular Lens Implantation on Visual Quality after Cataract Surgery
- Clinical Outcomes of Diffractive Trifocal Intraocular Lens in Both Eyes: A 6-Month Follow-Up