Korean J Ophthalmol.
2007 Jun;21(2):74-78. 10.3341/kjo.2007.21.2.74.
Sustainability of Orthokeratology as Demonstrated by Corneal Topography
- Affiliations
-
- 1Department of Ophthalmology, Bundang Jaesang General Hospital, Daejin Medical Center, Sungnam, Korea. dmc_ot@yahoo.co.kr
- KMID: 1101907
- DOI: http://doi.org/10.3341/kjo.2007.21.2.74
Abstract
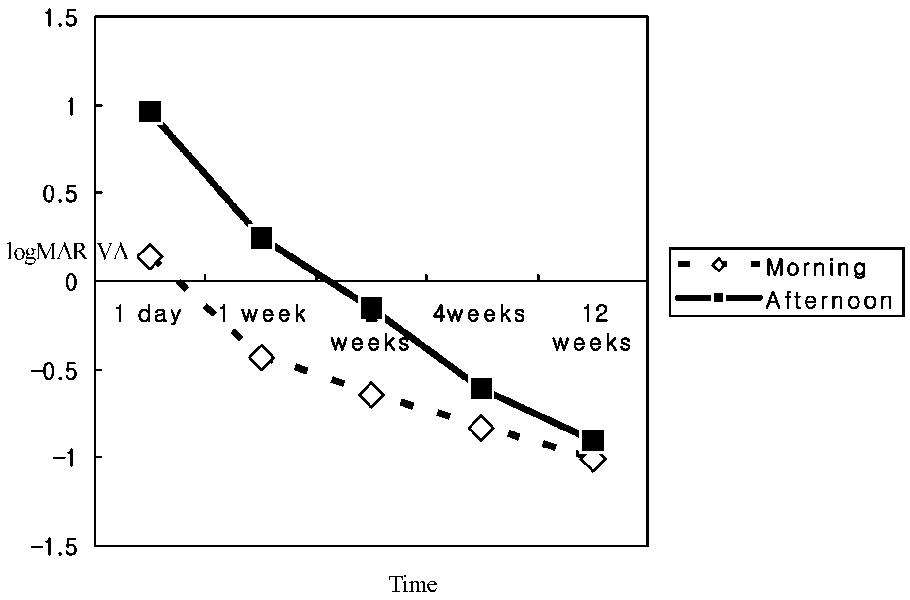
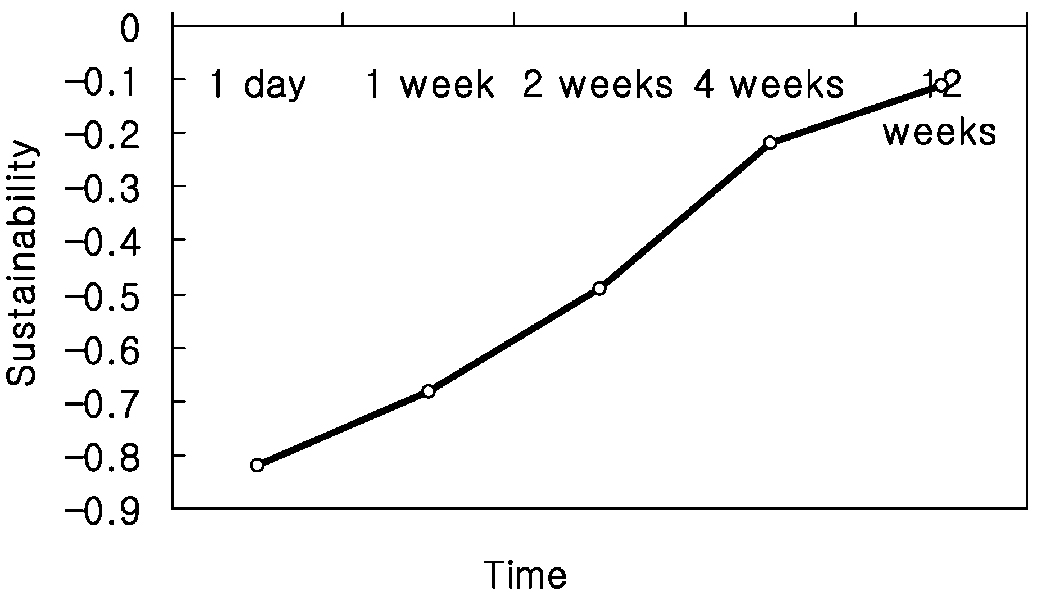
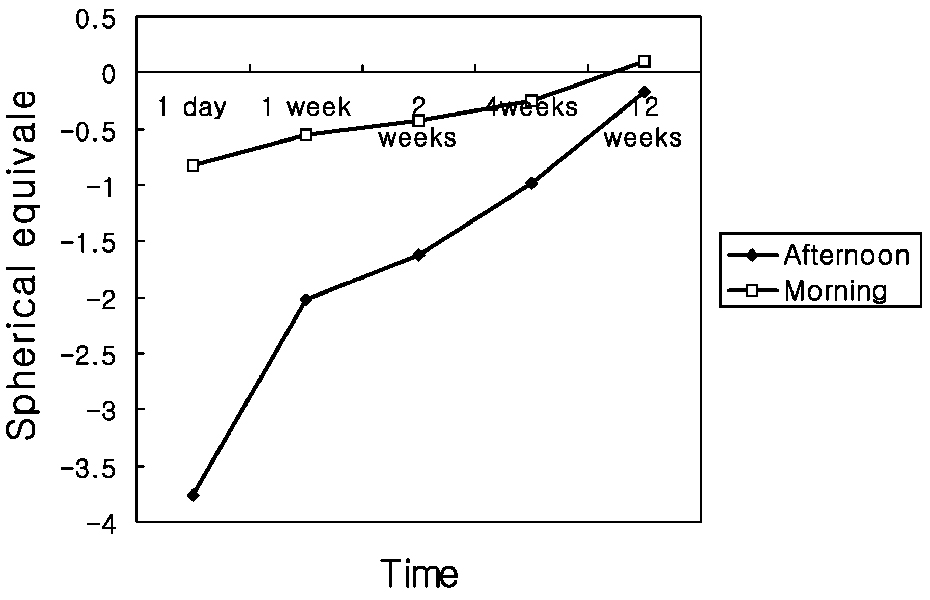
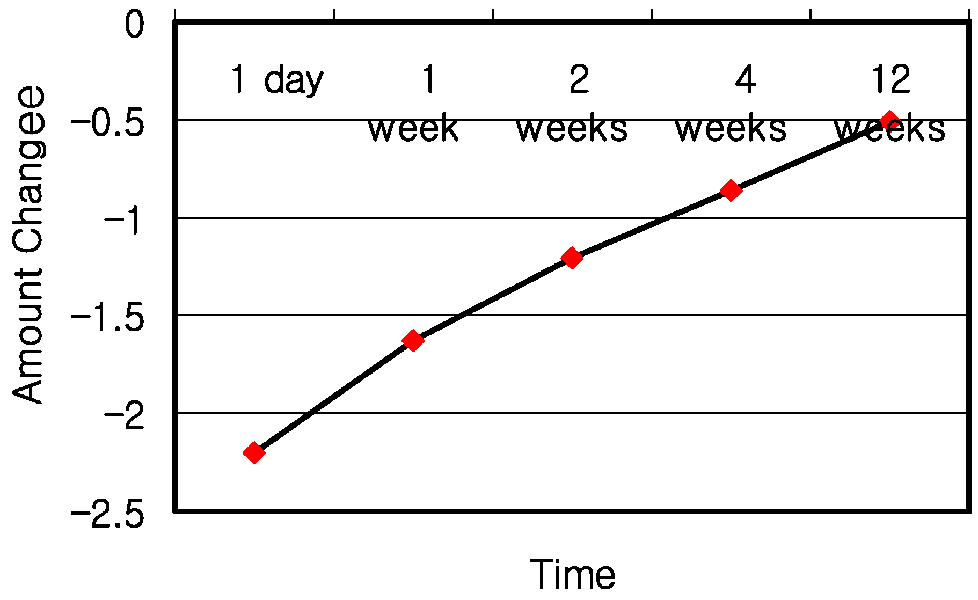
- PURPOSE: To determine the sustaining effects of orthokeratology. METHODS: This study enrolled 58 eyes with moderate myopia. LK-DM lenses (Lucid Korea Dream Lens(TM)) were fitted daily for at least eight hours on an overnight regimen. The effects of orthokeratology and it's sustainability throughout the day were recorded twice; immediately after removal in the morning and eight hours later. Sustainability was measured by comparing the changes from morning to afternoon for best uncorrected visual acuity, apical corneal power, keratometric values, spherical equivalent and induced astigmatism. RESULTS: UCVA demonstrated improved values at all follow up periods. Fluctuations during the day stabilized after 4 weeks of lens wear. K values averaged a mean of 42.4 mm at baseline, and reduced to 40.9 mm by week 12. Unaided logMAR visual acuity changed from 0.94+/-0.14 at baseline to -0.11+/-0.17 by week 12. The sustainability of orthokeratology, defined as the difference between morning and afternoon values of unaided logMAR visual acuity, increased from -0.82 on day 1 to -0.11 on week 12. CONCLUSIONS: UCVA and spherical refractive error did not change to a significant degree after 4 weeks. Although statistically insignificant minute fluctuations during the day were observed up to week 12, these fluctuations decreased to a statistically significant level after week 4.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
The Relationship Between Asphericity and Visual Acuity After Wearing Reverse-Geometry Lens
Jung Hwa Na, Jeong Hoon Choi, Ji Wook Yang, Young Chun Lee, Su Young Kim
J Korean Ophthalmol Soc. 2009;50(5):670-676. doi: 10.3341/jkos.2009.50.5.670.Analysis of Refractive Error and Corneal Asphericity in Elementary School Students in Ilsan City
Su Young Kim, Jeong Hoon Choi, Young Hoon Park, Bong Soon Chang, Ki Choong Mah, Young Chun Lee
J Korean Ophthalmol Soc. 2008;49(8):1317-1322. doi: 10.3341/jkos.2008.49.8.1317.
Reference
-
1. Wlodyga RJ, Bryla C. Corneal molding: the easy way. Contact Lens Spectrum. 1989. 4:58–65.2. Nichols JJ, Marsich MM, Nguyen M, et al. Overnight orthokeratology. Optom Vis Sci. 2000. 77:252–259.3. Swarbrick HA, Alharbi A. Overnight orthokeratology induces central corneal epithelial thinning. Invest Ophthalmol Vis Sci. 2001. 42:S597.4. Chang JW, Choi TH, Lee HB. J Korean Ophthalmol Soc. 2004. 45:908–912.5. Shin DB, Yang KM, Lee SB, et al. J Korean Ophthalmol Soc. 2003. 44:1748–1756.6. Kerns RL. Research in orthokeratology. Part VIII: results, conclusions and discussion of techniques. J Am Optom Assoc. 1978. 49:308–314.7. Binder PS, May CH, Grant SC. An evaluation of orthokeratology. Ophthalmology. 1980. 87:729–744.8. Polse KA, Brand RJ, Schwalbe JS, et al. The Berkeley Orthokeratology Study. Part II: efficacy and duration. Am J Optom Physiol Opt. 1983. 60:187–198.9. Coon LJ. Orthokeratology. Part II: evaluating the Tabb method. J Am Optom Assoc. 1984. 55:409–418.10. Mandell RB, Helen RS. Stability of the corneal contour. Am Acad Optom. 1968. 45:797–806.11. Carney LG, Clark BA. Experimental deformation of the in vivo cornea. Am Acad Optom. 1972. 49:28–34.12. Horner DG, Armitage KS, Wormsley KA, Mandell RB. Corneal molding recovery after contact lens wear. Optom Vis Sci. 1992. 69:S156–S157.13. Swarbrick HA, Wong G, O'Leary DJ. Corneal response to orthokeratology. Optom Vis Sci. 1998. 75:791–799.14. Yoon YM, Kim MK, Lee JL. J Korean Ophthalmol Soc. 2005. 46:1478–1485.15. Mountford J. An analysis of the changes in corneal shape and refractive error induced by accelerated orthokeratology. ICLC. 1997. 24:128–144.16. Swarbrick HA, Wong G, O'Leary DJ. Corneal response to orthokeratology. Optom Vis Sci. 1998. 75:791–799.17. Lui W-O, Edwards MH. Orthokeratology in low myopia. Part 1: efficacy and predictability. Cont Lens Anterior Eye. 2000. 23:77–89.18. Soni PS, Horner DG. Bennett ES, Weissman BA, editors. Orthokeratology. Clinical Contact Lens Practice. 1994. Philadelphia: Lippincott;1–7.19. Mountford J, Pesudovs K. An analysis of the astigmatic changes induced by accelerated orthokeratology. Clin Exp Optom. 2002. 85:284–293.20. Freeman RA. Predicting stable changes in orthokeratology. Contact Lens Forum. 1978. 3:21–31.21. Lui W-O, Edwards MH. Orthokeratology in low myopia. Part 2: corneal topographic changes and safety over 100 days. Cont Lens Anterior Eye. 2000. 23:90–99.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Patient Evaluation for Orthothokeratology Lens
- Correction of Limbus-to-Limbus Corneal Astigmatism with Toric Orthokeratology Lenses
- Effect of Toric Orthokeratology Lenses in Patients with Limbus to Limbus Corneal Astigmatism
- Clinical Characteristics of Prescribing Orthokeratology Lenses in Adult
- Major Complications of Overnight Orthokeratology Lens for Myopic Correction