Korean J Ophthalmol.
2008 Jun;22(2):137-142. 10.3341/kjo.2008.22.2.137.
Reorganization of Photoreceptor Layer on Optical Coherence Tomography Concurrent with Visual Improvement after Macular Hole Surgery
- Affiliations
-
- 1Department of Ophthalmology, College of Medicine, Pusan National University, Pusan, Korea. jlee@pusan.ac.kr
- KMID: 1099010
- DOI: http://doi.org/10.3341/kjo.2008.22.2.137
Abstract
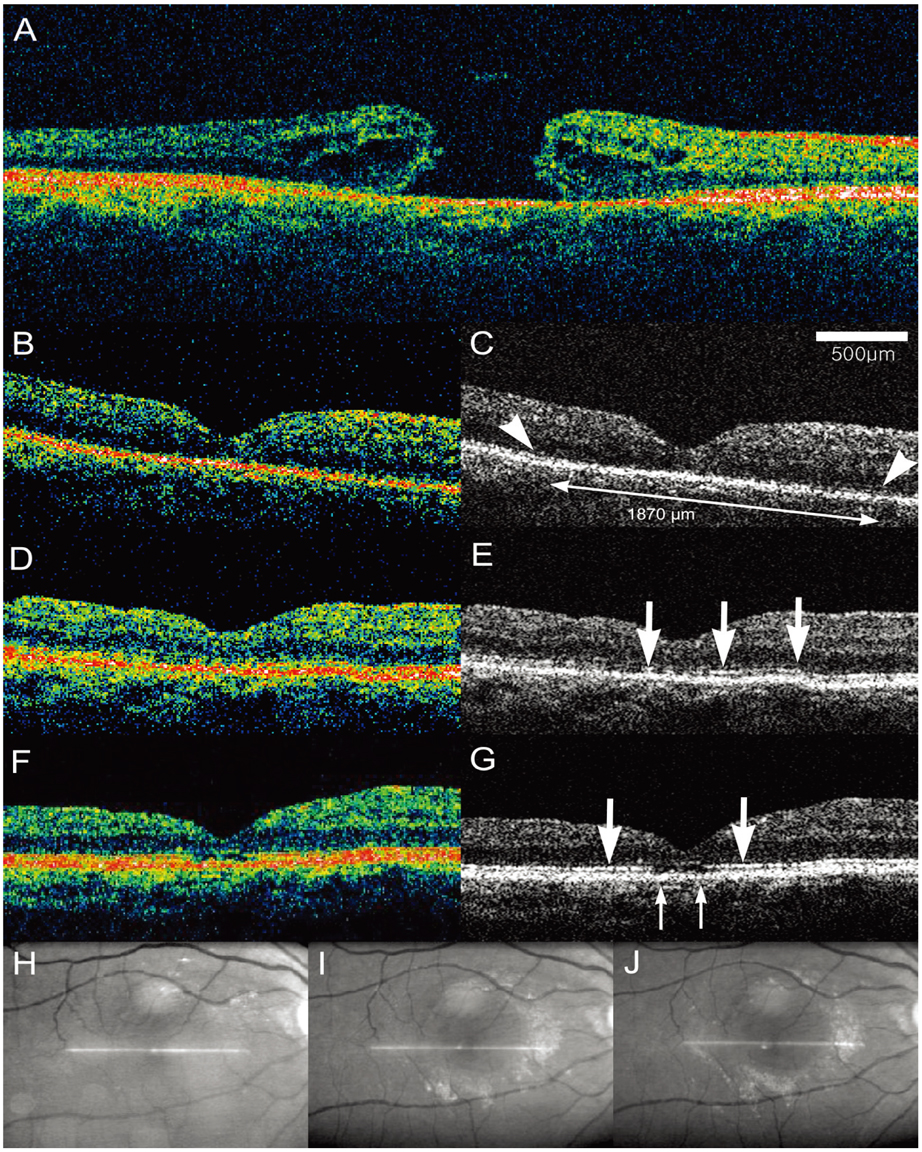
- To report three cases in which reorganization of the photoreceptor layer on optical coherence tomography (OCT) was concurrent with long-term visual recovery after macular hole surgery. Serial OCT scans of three eyes in which visual acuity continued to improve for 1 or more years after successful macular hole surgery were reviewed. Case 1. At postoperative four weeks, visual acuity was 20/100 with disorganized photoreceptor layer on OCT. The photoreceptor layer had been reorganized and visual acuity had improved to 20/25 by 1 year. Case 2. Two weeks after the operation, visual acuity was 20/125 and disorganization of the photoreceptor layer was noted. Visual acuity improved to 20/50 by four months. The photoreceptor layer had been partly reorganized and had appearance of a broken line. Visual acuity had improved to 20/40 and the photoreceptor layer had been reorganized further with a residual defect on OCT by 15 months. Case 3. Visual acuity at two weeks was 20/100. OCT revealed disorganization of the photoreceptor layer. Six months after the operation, the partly reorganized photoreceptor layer appeared as a broken line and visual acuity had reached 20/80. Visual acuity had improved further to 20/40 by 1 year, concurrent with improved organization of the photoreceptor layer. The reorganization of the photoreceptor layer plays a part in long-term improvement of visual acuity after macular hole surgery.
MeSH Terms
Figure
Reference
-
1. Ullrich S, Haritoglou C, Gass C, et al. Macular hole size as a prognostic factor in macular hole surgery. Br J Ophthalmol. 2002. 86:390–393.2. Kusuhara S, Teraoka Escaño MF, Fujii S, et al. Prediction of postoperative visual outcome based on hole configuration by optical coherence tomography in eyes with idiopathic macular holes. Am J Ophthalmol. 2004. 138:709–716.3. Yu SI, Kim HW, Yun IH. The evaluation of prognostic factors after vitrectomy for idiopathic macular hole with OCT. J Korean Ophthalmol Soc. 2007. 48:513–520.4. Kitaya N, Hikichi T, Kagokawa H, et al. Irregularity of photoreceptor layer after successful macular hole surgery prevents visual acuity improvement. Am J Ophthalmol. 2004. 138:308–310.5. Ko TH, Fujimoto JG, Duker JS, et al. Comparison of ultrahigh- and standard-resolution optical coherence tomography for imaging macular hole pathology and repair. Ophthalmology. 2004. 111:2033–2043.6. Villate N, Lee JE, Venkatraman A, Smiddy WE. Photoreceptor layer features in eyes with closed macular holes: Optical coherence tomography findings and correlation with visual outcomes. Am J Ophthalmol. 2005. 139:280–289.7. Lee JE, Kim EH, Oum BS. Relationship between visual acuity and photoreceptor layer or foveal thickness on optical coherence tomography after macular hole surgery. J Korean Ophthalmol Soc. 2006. 47:1966–1971.8. Moshfeghi AA, Flynn HW, Elner SG, et al. Persistent outer retinal defect after successful macular hole repair. Am J Ophthalmol. 2005. 139:183–184.9. Leonard RE, Smiddy WE, Flynn HW Jr, Feuer W. Long-term visual outcomes in patients with successful macular hole surgery. Ophthalmology. 1997. 104:1648–1652.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Evaluation of Correlation Between OCT Findings and Delayed Visual Acuity Improvement After Macular Hole Surgery
- Relationship between Visual Acuity and Photoreceptor Layer or Foveal Thickness on Optical Coherence Tomography after Macular Hole Surgery
- Recovery Course of Macular Structure after Macular Hole Surgery: Using a Spectral Domain Optical Coherence Tomography Image
- Long-Term Visual Outcomes and Prognostic Factors for Successful Idiopathic Macular Hole
- Correlation of Preoperative Optical Coherence Tomography with Preand Postoperative Visual Acuity of Macular Hole