Korean J Ophthalmol.
2008 Sep;22(3):190-193. 10.3341/kjo.2008.22.3.190.
Resolution of Severe Macular Edema in Adult Coats' Disease with Intravitreal Triamcinolone and Bevacizumab Injection
- Affiliations
-
- 1Department of Ophthalmology, School of Medicine, Dongsan Medical Center, Keimyung University, Daegu, Korea. eyedr@dreamwiz.com
- KMID: 1070757
- DOI: http://doi.org/10.3341/kjo.2008.22.3.190
Abstract
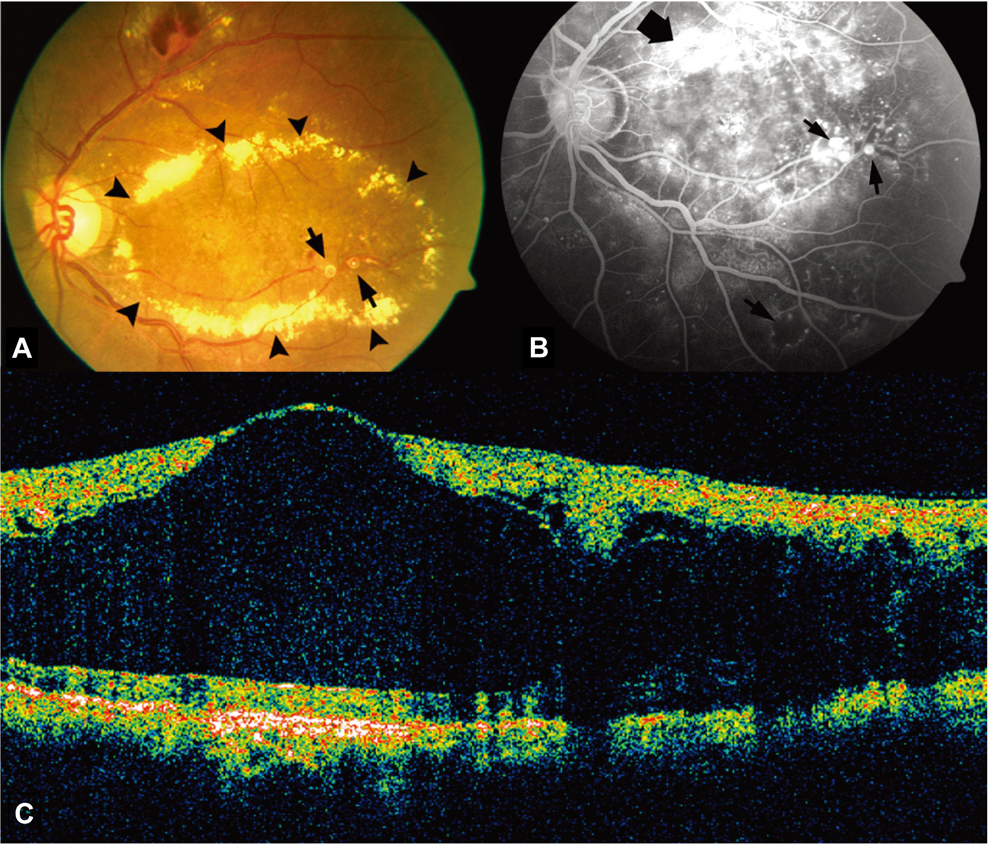
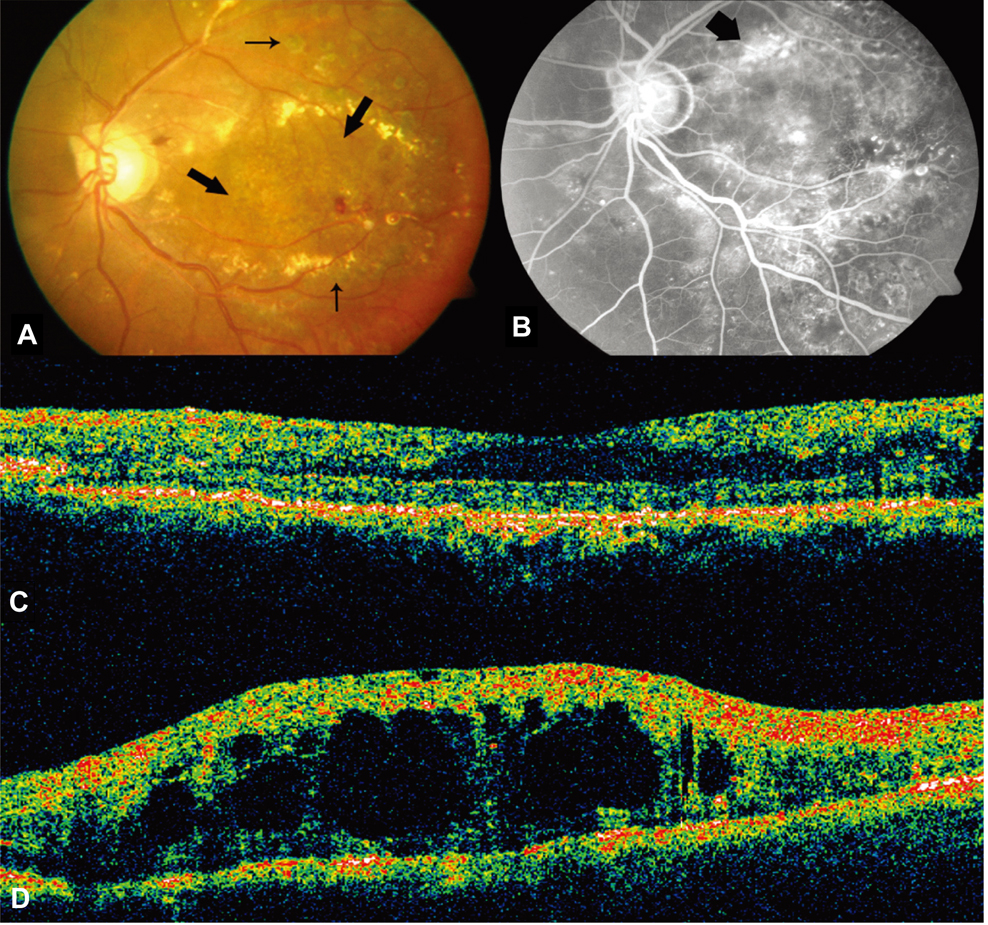
- A 47 year old male patient visited our hospital with the chief complaint of deterioration of the visual acuity in the left eye. The fundus examination revealed thick hard exudates, multiple aneurysms and telangiectasias of the retinal vessels in the posterior pole. Fluorescein angiography demonstrated massive leakage over an area of the aneurysms. Optical coherence tomography (Stratus OCT; Zeiss-Humphrey, Dubin, CA) revealed diffuse and marked thickening of the retina. Laser photocoagulation was performed under the diagnosis of Coats' disease. However, the treatment could not be performed satisfactorily. On the first and 6th weeks, an intravitreal injection of bevacizumab and triamcinolone acetonide was administered, and laser photocoagulation was again attempted. The effectiveness of eachagent on retinal edema was evaluated at the follow-up performed at 1, 2, 5, 7, 10 weeks and 6 months after the injection. At one week after the intravitreal bevacizumab injection, there was no improvement. An intravitreal injection of triamcinolone acetonide was performed 6 weeks after the initial diagnosis,which resulted in a reduction in the thickness of the macular edema. Therefore, laser photocoagulation was performed sufficiently on telangiectasias. The follow-up at 6 months showed a relative increase in the macular edema, but there was reduced leakage from the telangiectasias compared with the previous angiograph.
MeSH Terms
-
Angiogenesis Inhibitors/*therapeutic use
Antibodies, Monoclonal/*therapeutic use
Drug Therapy, Combination
Fluorescein Angiography
Glucocorticoids/*therapeutic use
Humans
Injections
Laser Coagulation
Macular Edema/*drug therapy/etiology
Male
Middle Aged
Retinal Diseases/complications/*drug therapy/surgery
Retinal Vessels/pathology
Telangiectasis/complications/*drug therapy/surgery
Tomography, Optical Coherence
Triamcinolone Acetonide/*therapeutic use
Vascular Endothelial Growth Factor A/antagonists & inhibitors
Vitreous Body
Figure
Cited by 1 articles
-
Intravitreal Ranibizumab Injection in Adult-onset Coats' Disease: A Case Report
Han Ul Kim, Seong Hwan Shin, Sung Pyo Park
J Korean Ophthalmol Soc. 2017;58(7):870-874. doi: 10.3341/jkos.2017.58.7.870.
Reference
-
1. Smithen LM, Brown GC, Brucker AJ, et al. Coats' disease diagnosed in adulthood. Ophthalmology. 2005. 112:1072–1078.2. Shields JA, Shields CL, Honavar SG, et al. Classification and management of Coats disease: the 2000 Proctor Lecture. Am J Ophthalmol. 2001. 131:572–583.3. Jones JH, Kroll AJ, Lou PL, Ryan EA. Coats' disease. Int Ophthalmol Clin. 2001. 41:189–198.4. Shields JA, Shields CL. Review: Coats disease. The 2001 LuEsther. T Mertz Lecture. Retina. 2002. 22:80–91.5. Shields JA, Shields CL, Honavar SG, Demirci H. Clinical variations and complications of Coats disease in 150 cases. The 2000 Sanford Gifford Memorial Lecture. Am J Ophthalmol. 2001. 131:561–571.6. Couvillion SS, Margolis R, Mavrofjides E, et al. Laser treatment of Coats' disease. J Pediatr Ophthalmol Strabismus. 2005. 42:367–368.7. Adam RS, Kertes PJ, Lam WC. Observations on the management of Coats' disease: less is more. Br J Ophthalmol. 2007. 91:303–306.8. Patelli F, Zumbo G, Fasolino G, et al. Treatment and outcome of exudative retinal detachment in Coats disease: a case report. Semin Ophthalmol. 2004. 19:117–118.9. Sun Y, Jain A, Moshfeghi DM. Elevated vascular endothelial growth factor levels in Coats disease: rapid response to pegaptanib sodium. Graefes Arch Clin Exp Ophthalmol. 2007. 245:1387–1389.10. Jarin RR, Teoh SCB, Lim TH. Resolution of severe macular oedema in adult Coat's syndrome with high-dose intravitreal triamcinolone acetonide. Eye. 2006. 20:163–165.11. Tripathi R, Ashton N. Electron microscopical study of Coat's disease. Br J Ophthalmol. 1971. 55:289–301.12. Jonas J. Intravitreal triamcinolone acetonide as treatment for extonsive exudative retinal detachment. Br J Ophthalmol. 2004. 88:587–588.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intravitreal Bevacizumab Injection in Adult Coats' Disease
- Comparison of Intravitreal Bevacizumab Alone Injection and Intravitreal Combination Low-Dose Bevacizumab-Triamcinolone Injection or Diabetic Macular Edema
- Intravitreal Triamcinolone Injection with or Without Bevacizumab for Diabetic Macular Edema
- Short-Term Results of Dexamethasone Intravitreal Implant in Patients with Refractory Diabetic Macular Edema
- Intravitreal Triamcinolone Versus Bevacizumab for Treatment of Diabetic Macular Edema