J Korean Acad Nurs.
2011 Jun;41(3):423-431. 10.4040/jkan.2011.41.3.423.
Predictive Bayesian Network Model Using Electronic Patient Records for Prevention of Hospital-Acquired Pressure Ulcers
- Affiliations
-
- 1Department of Nursing, Inha University, Incheon, Korea. insook.cho@inha.ac.kr
- 2Department of Nursing, Seoul National University Bundang Hospital, Seongnam, Korea.
- KMID: 1015492
- DOI: http://doi.org/10.4040/jkan.2011.41.3.423
Abstract
- PURPOSE
The study was designed to determine the discriminating ability of a Bayesian network (BN) for predicting risk for pressure ulcers.
METHODS
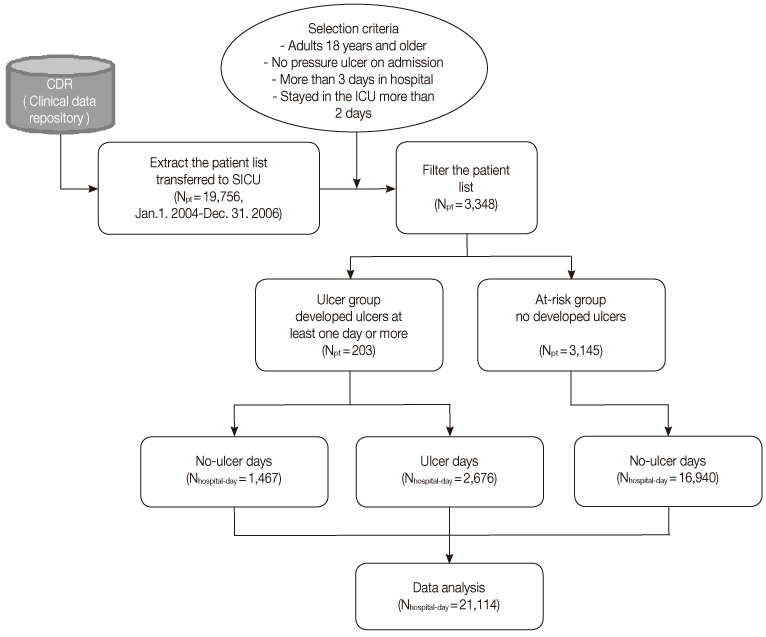
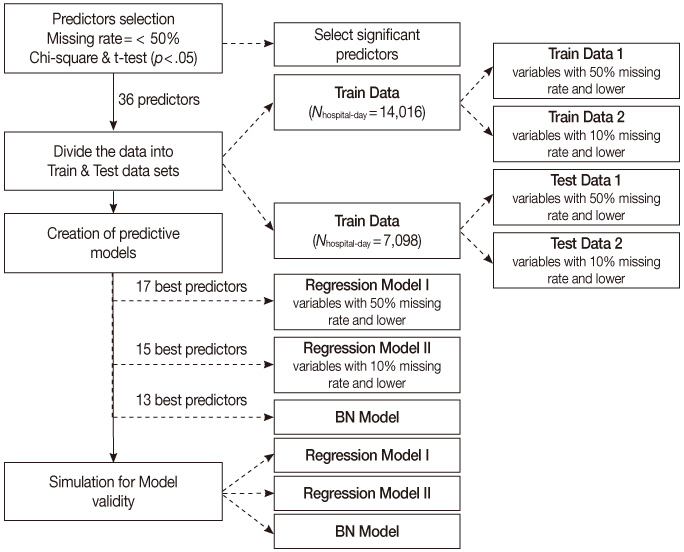
Analysis was done using a retrospective cohort, nursing records representing 21,114 hospital days, 3,348 patients at risk for ulcers, admitted to the intensive care unit of a tertiary teaching hospital between January 2004 and January 2007. A BN model and two logistic regression (LR) versions, model-I and -II, were compared, varying the nature, number and quality of input variables. Classification competence and case coverage of the models were tested and compared using a threefold cross validation method.
RESULTS
Average incidence of ulcers was 6.12%. Of the two LR models, model-I demonstrated better indexes of statistical model fits. The BN model had a sensitivity of 81.95%, specificity of 75.63%, positive and negative predictive values of 35.62% and 96.22% respectively. The area under the receiver operating characteristic (AUROC) was 85.01% implying moderate to good overall performance, which was similar to LR model-I. However, regarding case coverage, the BN model was 100% compared to 15.88% of LR.
CONCLUSION
Discriminating ability of the BN model was found to be acceptable and case coverage proved to be excellent for clinical use.
MeSH Terms
Figure
Cited by 2 articles
-
Reusability of EMR Data for Applying Cubbin and Jackson Pressure Ulcer Risk Assessment Scale in Critical Care Patients
Eunkyung Kim, Mona Choi, JuHee Lee, Young Ah Kim
Healthc Inform Res. 2013;19(4):261-270. doi: 10.4258/hir.2013.19.4.261.Development and Evaluation of Electronic Health Record Data-Driven Predictive Models for Pressure Ulcers
Seul Ki Park, Hyeoun-Ae Park, Hee Hwang
J Korean Acad Nurs. 2019;49(5):575-585. doi: 10.4040/jkan.2019.49.5.575.
Reference
-
1. Baumgarten M, Margolis DJ, Localio AR, Kagan SH, Lowe RA, Konsian B, et al. Extrinsic risk factors for pressure ulcers early in the hospital stay: A nested case-control study. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences. 2008. 63:408–413.2. Beeckman D, Schoonhoven L, Fletcher J, Furtado K, Gunningberg L, Heyman H, et al. EPUAP classification system for pressure ulcers: European reliability study. Journal of Advanced Nursing. 2007. 60:682–691. doi:10.1111/j.1365-2648.2007.04474.x.3. Bergstrom N, Braden B, Kemp M, Champagne M, Ruby E. Predicting pressure ulcer risk: A multisite study of the predictive validity of the Braden Scale. Nursing Research. 1998. 47:261–269. doi:10.1097/00006199-199809000-00005.4. Brown SJ. The Braden Scale: A review of the research evidence. Orthopaedic Nursing. 2004. 23:30–38. doi:10.1097/00006416-200401000-00010.5. Burnside ES, Rubin DL, Shachter RD. Using a Bayesian network to predict the probability and type of breast cancer represented by microcalcifications on mammography. Studies in Health Technology And Informatics. 2004. 107(Pt 1):13–17.6. Cho I, Noh M. Braden Scale: Evaluation of clinical usefulness in an intensive care unit. Journal of Advanced Nursing. 2010. 66:293–302. doi:10.1111/j.1365-2648.2009.05153.x.7. Cho I, Yoon HY, Park SI, Lee HS. Availability of nursing data in an electronic nursing record system for a development of a risk assessment. Journal of Korean Society of Medical Informatics. 2008. 14:161–168.8. Cios KJ, Moore GW. Uniqueness of medical data mining. Artificial Intelligence in Medicine. 2002. 26:1–24. doi:10.1016/S0933-3657(02)00049-0.9. Cover TM, Thomas JA. Elements of information theory. 1991. New York: John Wiley & Sons.10. De Laat EH, Pickkers P, Schoonhoven L, Verbeek AL, Feuth T, van Achterberg T. Guideline implementation results in a decrease of pressure ulcer incidence in critically ill patients. Critical Care Medicine. 2007. 35:815–820. doi:10.1097/01.CCM.0000257072.10313.56.11. Defloor T, Grypdonck MF. Pressure ulcers: Validation of two risk assessment scales. Journal of Clinical Nursing. 2005. 14:373–382. doi:10.1111/j.1365-2702.2004.01058.x.12. Fernandez G. Statistical data mining using SAS applications. 2010. 2nd ed. Minnesota: CRC Press.13. Fischer JE, Bachmann LM, Jaeschke R. A readers' guide to the interpretation of diagnostic test properties: Clinical example of sepsis. Intensive Care Medicine. 2003. 29:1043–1051. doi:10.1007/s00134-003-1761-8.14. Fogerty MD, Abumrad NN, Nanney L, Arbogast PG, Poulose B, Barbul A. Risk factors for pressure ulcers in acute care hospitals. Wound Repair and Regeneration. 2008. 16:11–18. doi:10.1111/j.1524-475X.2007.00327.x.15. Harrison JH. Introduction to the mining of clinical data. Clinics in Laboratory Medicine. 2008. 28:1–7. doi:10.1016/j.cll.2007.10.001.16. Hatanaka N, Yamamoto Y, Ichihara K, Mastuo S, Nakamura Y, Watanabe M, et al. A new predictive indicator for development of pressure ulcers in bedridden patients based on common laboratory tests results. Journal of Clinical Pathology. 2008. 61:514–518. doi:10.1136/jcp.2007.050195.17. Jones KR, Fennie K, Lenihan A. Evidence-based management of chronic wounds. Advances in Skin and Wound Care. 2007. 20:591–600. doi:10.1097/01.ASW.0000284936.32707.8d.18. Korb KB, Nicholson AE. Bayesian artificial intelligence. 2004. London: Chapman & Hall/CRC press.19. Lee KO, Shin HJ, Park HA, Jeong HM, Lee MH, Choi EH, et al. Patient severity classification in a medical ICU using APACHE III and patient severity classification tool. Journal of Korean Academy of Nursing. 2000. 30:1243–1253.20. Lee SM, Abbott P, Johantgen M. Logistic regression and Bayesian networks to study outcomes using large data sets. Nursing Research. 2005. 54:133–138. doi:10.1097/00006199-200503000-00009.21. Lee YH, Jeong IS, Jeon SS. A comparative study on the predictive validity among presusre ulcer risk assessment scales. Journal of Korean Academy of Nursing. 2003. 33:162–169.22. Lucas PJF, van der Gaag LC, Abu-Hanna A. Bayesian network in biomedicine and health-care. Artificial Intelligence in Medicine. 2004. 30:201–214. doi:10.1016/j.artmed.2003.11.001.23. Park HS, Park KY, Yu SM. Factors influencing the development of pressure ulcers in surgical patients. Journal of Korean Academy of Nursing. 2005. 35:125–134.24. Pesut D. Weaver C, Delaney C, Weber P, Carr R, editors. 21st century nursing knowledge work: Reasoning into the future. Nursing and informatics for the 21st century: Cases, practice, and the future. 2006. Chicago: HIMSS Press;14–17.25. Russo CA, Steiner C, Spector W. Rep. No. HCUP Statistical Brief #64. Hospitalizations related to pressure ulcers, 2006. 2008. Rockville, MD: Agency for Healthcare Research and Quality.26. Schoonhoven L, Haalboom JR, Bousema MT, Algra A, Grobbee DE, Grypdonck MH, et al. Prospective cohort study of routine use of risk assessment scales for prediction of pressure ulcers. British Medical Journal. 2002. 325:797–800. doi:10.1136/bmj.325.7368.797.27. Thede LQ, Sewell JP. Informatics and nursing: Competencies and applications. 2010. 3rd ed. Philadelphia: Wolters Kluwer Health | Lippincott Williams & Wilkins.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Bayesian Network Approaches to Health Services Research
- Development and Evaluation of Electronic Health Record Data-Driven Predictive Models for Pressure Ulcers
- A Hybrid Bayesian Network Model for Predicting Breast Cancer Prognosis
- Reusability of EMR Data for Applying Cubbin and Jackson Pressure Ulcer Risk Assessment Scale in Critical Care Patients
- Availability of nursing data in an electronic nursing record system for a development of a risk assessment tool for pressure ulcers