J Korean Rheum Assoc.
2009 Dec;16(4):271-280.
Alterations in the Kinetics of CD4+ T Cell Responses with Aging
- Affiliations
-
- 1Section of Rheumatology, School of Medicine, Yale University, New Haven, Connecticut, USA. insoo.kang@yale.edu
- 2Department of Radiology, School of Medicine, Hallym University, Chuncheon, Korea.
- 3Department of Orthopedics, CHA Gumi Medical Center, CHA University, Gumi, Korea.
Abstract
OBJECTIVE
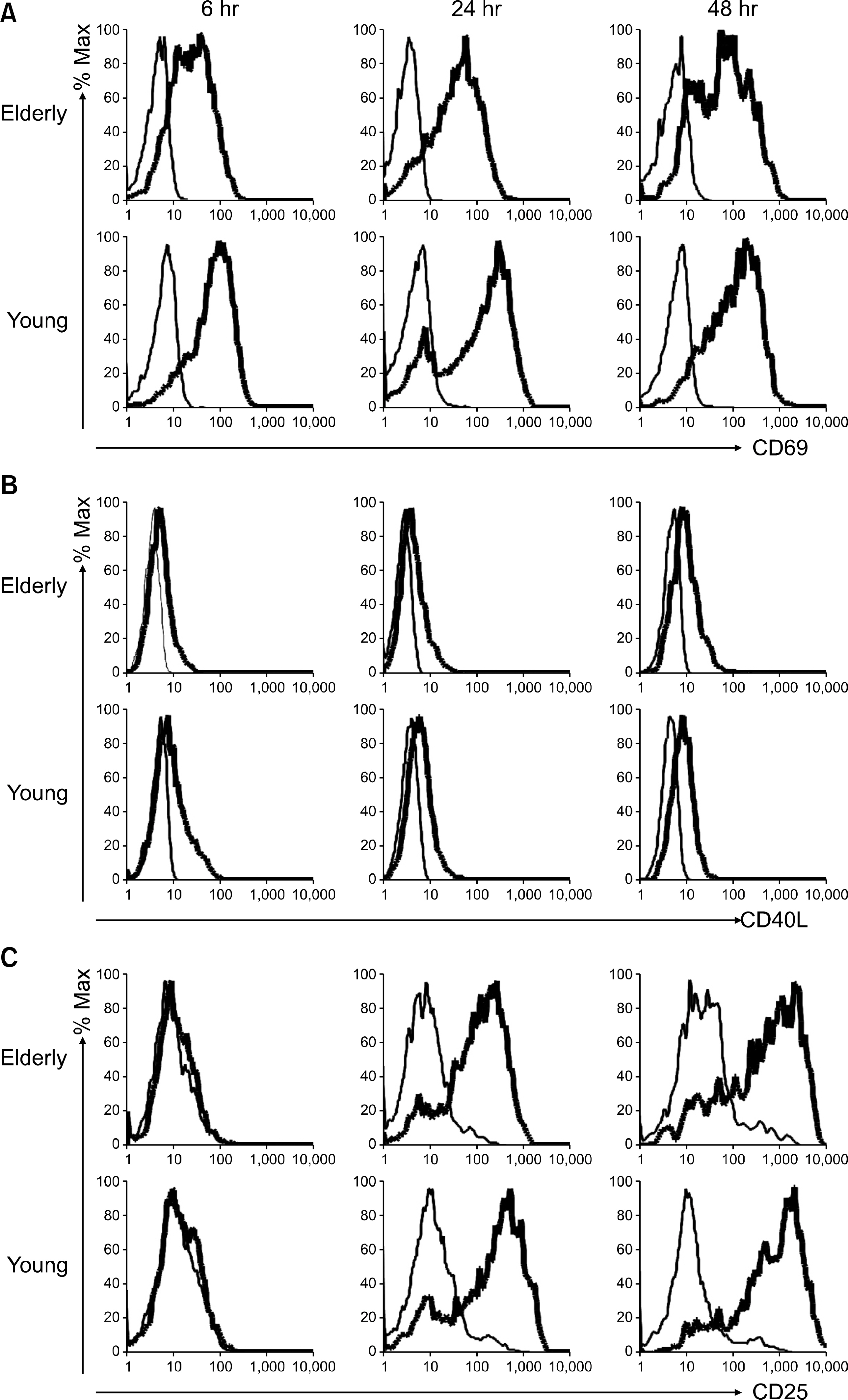
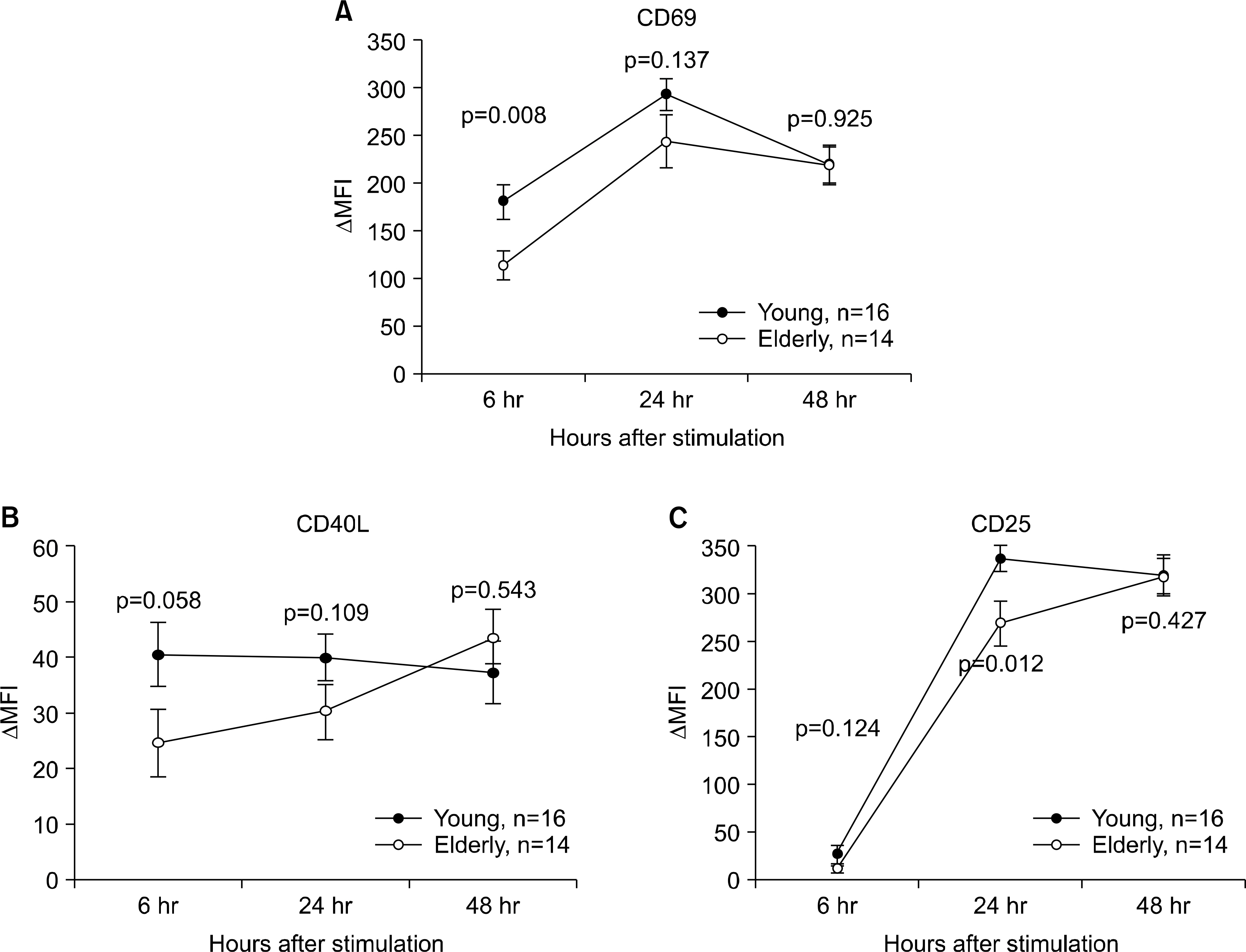
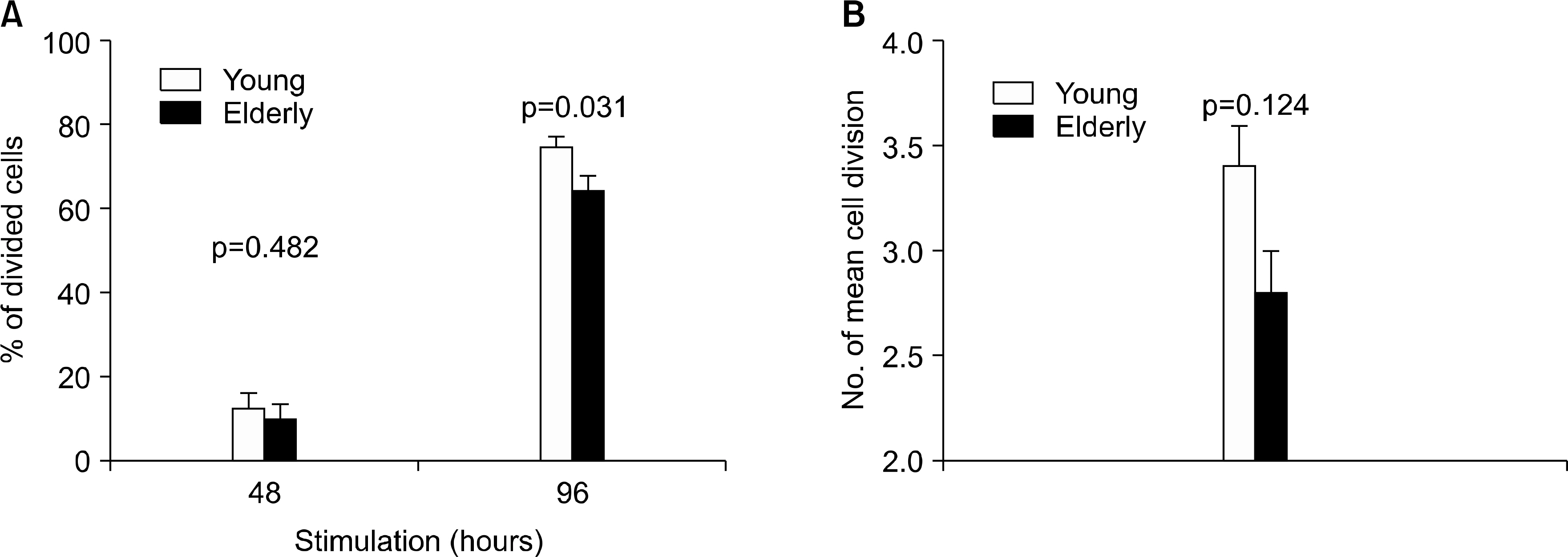
Alterations in the immune system occur with aging, and these contribute to an increased risk of infection and malignancy. The age-associated changes in T cell immunity range from single cell function to the maintenance of cell populations. We investigated the kinetics of CD4+ T cell activation and proliferation in young and elderly subjects after stimulating their peripheral blood mononuclear cells with anti-CD3 and anti-CD28 antibodies (Abs). METHODS: The expressions of the activation markers CD69, CD40L and CD25 on the CD4+ T cells from young (n=14) and elderly (n=19) were analyzed at 6, 24 and 48 hours (hrs) of T cell receptor (TCR) stimulation by using flow cytometry. In the same individuals, the CD4+ T cell proliferation was determined at 48 and 96 hrs of TCR stimulation by using the CFSE dilution method. RESULTS: The elderly had decreased CD69 and CD40L expressions on the CD4+ T cells at 6 hrs of stimulation, as compared to that of the young patients. The elderly also had a decreased CD25 expression on the CD4+ T cells at 24 hrs of stimulation. However, the two groups had similar levels of the CD25, CD69 and CD40L expressions at 48 hrs of stimulation. The elderly had decreased CD4+ T cell proliferation at 96 hrs of stimulation, as compared to that of the young, although both groups had similar levels of CD4+ T cell proliferation at 48 hrs of stimulation. CONCLUSION: Our findings suggest that the elderly have altered kinetics of CD4+ T cell activation and proliferation in response to anti-CD3 and -CD28 Ab stimulation, and that such an altered response is governed by the duration of stimulation.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Linton PJ, Dorshkind K. Age-related changes in lymphocyte development and function. Nat Immunol. 2004; 5:133–9.
Article2. Miller RA. Aging and Immune Function. In: Paul WE, ed. Fundamental Immunology. 4th ed. p.947–966. Philadelphia, Lippincott-Raven,. 1999.3. Naylor K, Li G, Vallejo AN, Lee WW, Koetz K, Bryl E, et al. The influence of age on T cell generation and TCR diversity. J Immunol. 2005; 174:7446–52.
Article4. Nikolich-Zugich J. T cell aging: naive but not young. J Exp Med. 2005; 201:837–40.5. Solana R, Pawelec G, Tarazona R. Aging and innate immunity. Immunity. 2006; 24:491–4.
Article6. Castle SC. Clinical relevance of age-related immune dysfunction. Clin Infect Dis. 2000; 31:578–85.
Article7. Haynes BF, Markert ML, Sempowski GD, Patel DD, Hale LP. The role of the thymus in immune reconstitution in aging, bone marrow transplantation, and HIV-1 infection. Annu Rev Immunol. 2000; 18:529–60.
Article8. Goronzy JJ, Weyand CM. T cell development and receptor diversity during aging. Curr Opin Immunol. 2005; 17:468–75.
Article9. Kaech SM, Wherry EJ, Ahmed R. Effector and memory T-cell differentiation: implications for vaccine development. Nat Rev Immunol. 2002; 2:251–62.
Article10. Jameson SC. Maintaining the norm: T-cell homeostasis. Nat Rev Immunol. 2002; 2:547–56.
Article11. Goronzy JJ, Lee WW, Weyand CM. Aging and T-cell diversity. Exp Gerontol. 2007; 42:400–6.
Article12. Yung RL. Changes in immune function with age. Rheum Dis Clin North Am. 2000; 26:455–73.
Article13. Czesnikiewicz-Guzik M, Lee WW, Cui D, Hiruma Y, Lamar DL, Yang ZZ, et al. T cell subset-specific susceptibility to aging. Clin Immunol. 2008; 127:107–18.
Article14. Kang I, Hong MS, Nolasco H, Park SH, Dan JM, Choi JY, et al. Age-associated change in the frequency of memory CD4+ T cells impairs long term CD4+ T cell responses to influenza vaccine. J Immunol. 2004; 173:673–81.15. Ginn-Pease ME, Whisler RL. Alterations in the expression of interleukin-2R subunits by activated T cells from elderly humans are uncoupled from aberrancies in G1/S progression. J Interferon Cytokine Res. 2001; 21:515–21.
Article16. Pawelec G, Adibzadeh M, Solana R, Beckman I. The T cell in the ageing individual. Mech Ageing Dev. 1997; 93:35–45.17. Schindowski K, Frohlich L, Maurer K, Muller WE, Eckert A. Age-related impairment of human T lym-phocytes' activation: specific differences between CD4 (+) and CD8 (+) subsets. Mech Ageing Dev. 2002; 123:375–90.18. Fernandez-Gutierrez B, Jover JA, De Miguel S, Hernandez-Garcia C, Vidan MT, Ribera JM, et al. Early lymphocyte activation in elderly humans: impaired T and T-dependent B cell responses. Exp Gerontol. 1999; 34:217–29.19. Beckman I, Dimopoulos K, Xu XN, Bradley J, Henschke P, Ahern M. T cell activation in the elderly: evidence for specific deficiencies in T cell/accessory cell interactions. Mech Ageing Dev. 1990; 51:265–76.
Article20. Douziech N, Seres I, Larbi A, Szikszay E, Roy PM, Arcand M, et al. Modulation of human lymphocyte proliferative response with aging. Exp Gerontol. 2002; 37:369–87.
Article21. Tortorella C, Pisconti A, Piazzolla G, Antonaci S. APC-dependent impairment of T cell proliferation in aging: role of CD28- and IL-12/IL-15-mediated signaling. Mech Ageing Dev. 2002; 123:1389–402.
Article22. Sansoni P, Fagnoni F, Vescovini R, Mazzola M, Brianti V, Bologna G, et al. T lymphocyte proliferative capability to defined stimuli and costimulatory CD28 pathway is not impaired in healthy centenarians. Mech Ageing Dev. 1997; 96:127–36.
Article23. Glimm H, Eaves CJ. Direct evidence for multiple self-renewal divisions of human in vivo repopulating hematopoietic cells in short-term culture. Blood. 1999; 94:2161–8.
Article24. Banchereau J, Bazan F, Blanchard D, Briere F, Galizzi JP, van Kooten C, et al. The CD40 antigen and its ligand. Annu Rev Immunol. 1994; 12:881–922.
Article25. Smith KA. The interleukin 2 receptor. Annu Rev Cell Biol. 1989; 5:397–425.
Article26. Smith-Garvin JE, Koretzky GA, Jordan MS. T cell activation. Annu Rev Immunol. 2009; 27:591–619.
Article27. Frentsch M, Arbach O, Kirchhoff D, Moewes B, Worm M, Rothe M, et al. Direct access to CD4+ T cells specific for defined antigens according to CD154 expression. Nat Med. 2005; 11:1118–24.
Article28. Kahi S, Cozon GJ, Greenland T, Wallon M, Gay-Andrieu F, Peyron F. A rapid flow cytometric method to explore cellular immunity against Toxoplasma gondii in humans. Clin Diagn Lab Immunol. 1998; 5:745–8.29. Maino VC, Suni MA, Ruitenberg JJ. Rapid flow cytometric method for measuring lymphocyte subset activation. Cytometry. 1995; 20:127–33.
Article30. Michalek J, Collins RH, Durrani HP, Vaclavkova P, Ruff LE, Douek DC, et al. Definitive separation of graft-versus-leukemia- and graft-versus-host-specific CD4+ T cells by virtue of their receptor beta loci sequences. Proc Natl Acad Sci USA. 2003; 100:1180–4.31. Eisenbraun MD, Tamir A, Miller RA. Altered composition of the immunological synapse in an anergic, age-dependent memory T cell subset. J Immunol. 2000; 164:6105–12.
Article32. Garcia GG, Miller RA. Single-cell analyses reveal two defects in peptide-specific activation of naive T cells from aged mice. J Immunol. 2001; 166:3151–7.
Article33. Tamir A, Eisenbraun MD, Garcia GG, Miller RA. Age-dependent alterations in the assembly of signal transduction complexes at the site of T cell/APC interaction. J Immunol. 2000; 165:1243–51.
Article34. Sallusto F, Lenig D, Forster R, Lipp M, Lanzavecchia A. Two subsets of memory T lymphocytes with distinct homing potentials and effector functions. Nature. 1999; 401:708–12.
Article35. Slagboom PE, Droog S, Boomsma DI. Genetic determination of telomere size in humans: a twin study of three age groups. Am J Hum Genet. 1994; 55:876–82.36. Weng NP, Hathcock KS, Hodes RJ. Regulation of telomere length and telomerase in T and B cells: a mechanism for maintaining replicative potential. Immunity. 1998; 9:151–7.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Role of CD4 T Cell Help in CD8 T Cell Differentiation and Function During Chronic Infection and Cancer
- Kinetics of IFN-gamma and IL-17 Production by CD4 and CD8 T Cells during Acute Graft-versus-Host Disease
- The Kinetics of Secondary Response of Antigen-Specific CD4+ T Cells Primed in vitro with Antigen
- Role for CD40 and CD40L Expression in Generating CD8 T Cell Response to Minor Histcompatibility Antigen, H60
- Comprehensive Analysis of Epstein-Barr Virus LMP2A-Specific CD8+ and CD4+ T Cell Responses Restricted to Each HLA Class I and II Allotype Within an Individual