Korean J Ophthalmol.
2011 Feb;25(1):8-14. 10.3341/kjo.2011.25.1.8.
Factors Influencing Corneal Flap Thickness in Laser In Situ Keratomileusis with a Femtosecond Laser
- Affiliations
-
- 1Department of Ophthalmology and Visual Science, Seoul St. Mary's Hospital, The Catholic University of Korea School of Medicine, Seoul, Korea. ckjoo@catholic.ac.kr
- KMID: 994405
- DOI: http://doi.org/10.3341/kjo.2011.25.1.8
Abstract
- PURPOSE
To evaluate factors responsible for the variability between intended and achieved corneal-flap thickness during femtosecond laser-assisted laser in situ keratomileusis (LASIK).
METHODS
A prospective, nonrandomized, case study was performed on 35 eyes of 18 consecutive patients who underwent LASIK surgery using the 60 kHz femtosecond laser microkeratome. Eyes were assigned to three different thickness groups, with 110-, 120-, or 130-microm cut depths. Anterior segment optical coherence tomography was used to assess the morphology of 35 LASIK flaps at postoperative one week postoperatively. The flap thickness was assessed at seven measuring points across each flap. Patient age, preoperative spherical equivalent, manual keratometry, preoperative central pachymetry, and regional variability of the cornea were evaluated to determine where they influenced the achieved corneal flap thickness.
RESULTS
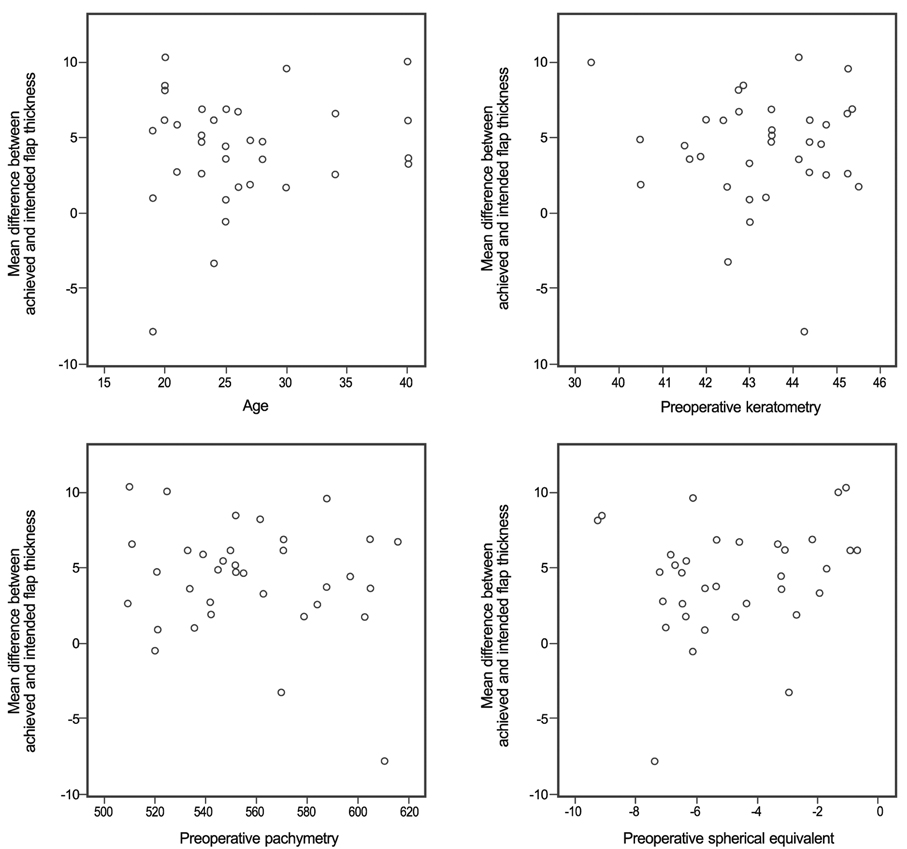
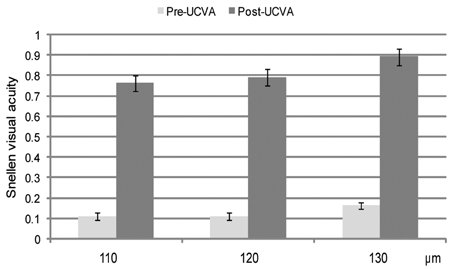
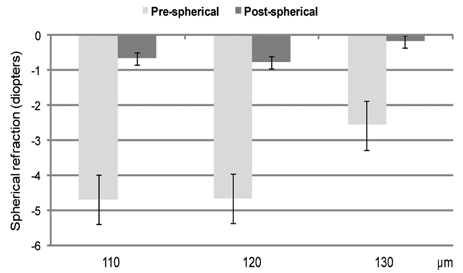
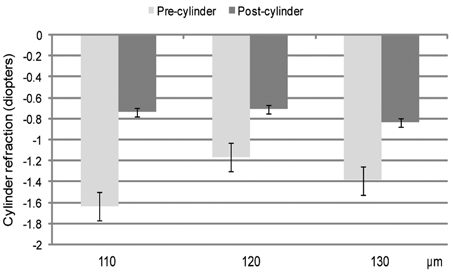
Cuttings of all flaps were easily performed without any intraoperative complications. Flap-thickness measurements had a mean of 115.21 +/- 4.98 microm (intended thickness, 110 microm), 121.90 +/- 5.79 microm (intended, 120 microm), and 134.38 +/- 5.04 microm (intended, 130 microm), respectively. There was no significant difference between the 110-microm and 120-microm groups when compared with the 130-microm group (one-way analysis of variance test, p > 0.05). Patients' age, preoperative spherical equivalent, manual keratometry, and preoperative central pachymetry did not affect the achieved flap thickness (Pearson correlations test, p > 0.05). The reproducibility of flap thickness in the central 1.5-mm radius area was more accurate than that in the peripheral 3.0 to 4.0-mm radius area (paired samples t-test, p < 0.05).
CONCLUSIONS
Femtosecond laser-assisted LASIK is likely to reproduce a reliable thickness of the corneal flap, which is independent of corneal shape factors or refractive status. Future studies should focus on variations in corneal biomechanical factors, which may also play an important role in determining flap thickness.
MeSH Terms
Figure
Reference
-
1. Choudhri SA, Feigenbaum SK, Pepose JS. Factors predictive of LASIK flap thickness with the Hansatome zero compression microkeratome. J Refract Surg. 2005. 21:253–259.2. Seiler T, Quurke AW. Iatrogenic keratectasia after LASIK in a case of forme fruste keratoconus. J Cataract Refract Surg. 1998. 24:1007–1009.3. Seiler T, Koufala K, Richter G. Iatrogenic keratectasia after laser in situ keratomileusis. J Refract Surg. 1998. 14:312–317.4. Koch DD. The riddle of iatrogenic keratectasia. J Cataract Refract Surg. 1999. 25:453–454.5. Yildirim R, Aras C, Ozdamar A, et al. Reproducibility of corneal flap thickness in laser in situ keratomileusis using the Hansatome microkeratome. J Cataract Refract Surg. 2000. 26:1729–1732.6. Giledi O, Mulhern MG, Espinosa M, et al. Reproducibility of LASIK flap thickness using the Hansatome microkeratome. J Cataract Refract Surg. 2004. 30:1031–1037.7. Krueger RR, Dupps WJ Jr. Biomechanical effects of femtosecond and microkeratome-based flap creation: prospective contralateral examination of two patients. J Refract Surg. 2007. 23:800–807.8. Alió JL, Piñero DP. Very high-frequency digital ultrasound measurement of the LASIK flap thickness profile using the IntraLase femtosecond laser and M2 and Carriazo-Pendular microkeratomes. J Refract Surg. 2008. 24:12–23.9. Choi SK, Kim JH, Lee D, et al. Creation of an extremely thin flap using IntraLase femtosecond laser. J Cataract Refract Surg. 2008. 34:864–867.10. Kohnen T, Thomala MC, Cichocki M, Strenger A. Internal anterior chamber diameter using optical coherence tomography compared with white-to-white distances using automated measurements. J Cataract Refract Surg. 2006. 32:1809–1813.11. Li Y, Netto MV, Shekhar R, et al. A longitudinal study of LASIK flap and stromal thickness with high-speed optical coherence tomography. Ophthalmology. 2007. 114:1124–1132.12. Pallikaris IG, Papatzanaki ME, Stathi EZ, et al. Laser in situ keratomileusis. Lasers Surg Med. 1990. 10:463–468.13. Behrens A, Langenbucher A, Kus MM, et al. Experimental evaluation of two current-generation automated microkeratomes: the Hansatome and the Supratome. Am J Ophthalmol. 2000. 129:59–67.14. Sarkisian KA, Petrov AA. Experience with the Nidek MK-2000 microkeratome in 1,220 cases. J Refract Surg. 2001. 17:2 Suppl. S252–S254.15. Choi YI, Park SJ, Song BJ. Corneal flap dimensions in laser in situ keratomileusis using the innovatome automatic microkeratome. Korean J Ophthalmol. 2000. 14:7–11.16. Shemesh G, Dotan G, Lipshitz I. Predictability of corneal flap thickness in laser in situ keratomileusis using three different microkeratomes. J Refract Surg. 2002. 18:3 Suppl. S347–S351.17. Spadea L, Cerrone L, Necozione S, Balestrazzi E. Flap measurements with the Hansatome microkeratome. J Refract Surg. 2002. 18:149–154.18. Arbelaez MC. Nidek MK 2000 microkeratome clinical evaluation. J Refract Surg. 2002. 18:3 Suppl. S357–S360.19. Flanagan GW, Binder PS. Precision of flap measurements for laser in situ keratomileusis in 4428 eyes. J Refract Surg. 2003. 19:113–123.20. Solomon KD, Donnenfeld E, Sandoval HP, et al. Flap thickness accuracy: comparison of 6 microkeratome models. J Cataract Refract Surg. 2004. 30:964–977.21. Duffey RJ. Thin flap laser in situ keratomileusis: flap dimensions with the Moria LSK-One manual microkeratome using the 100-microm head. J Cataract Refract Surg. 2005. 31:1159–1162.22. Solomon KD, Donnenfeld E, Sandoval HP, et al. Flap thickness accuracy: comparison of 6 microkeratome models. J Cataract Refract Surg. 2004. 30:964–977.23. Holzer MP, Vargas LG, Sandoval HP, et al. Corneal flap complications in refractive surgery. Part 1: development of an experimental animal model. J Cataract Refract Surg. 2003. 29:795–802.24. Ambrósio R Jr, Wilson SE. Complications of laser in situ keratomileusis: etiology, prevention, and treatment. J Refract Surg. 2001. 17:350–379.25. Kurtz RM, Horvath C, Liu HH, et al. Lamellar refractive surgery with scanned intrastromal picosecond and femtosecond laser pulses in animal eyes. J Refract Surg. 1998. 14:541–548.26. Sarayba MA, Juhasz T, Chuck RS, et al. Femtosecond laser posterior lamellar keratoplasty: a laboratory model. Cornea. 2005. 24:328–333.27. Soong HK, Mian S, Abbasi O, Juhasz T. Femtosecond laser-assisted posterior lamellar keratoplasty: initial studies of surgical technique in eye bank eyes. Ophthalmology. 2005. 112:44–49.28. Seitz B, Langenbucher A, Hofmann-Rummelt C, et al. Nonmechanical posterior lamellar keratoplasty using the femtosecond laser (femto-plak) for corneal endothelial decompensation. Am J Ophthalmol. 2003. 136:769–772.29. Seitz B, Brünner H, Viestenz A, et al. Inverse mushroom-shaped nonmechanical penetrating keratoplasty using a femtosecond laser. Am J Ophthalmol. 2005. 139:941–944.30. Jonas JB, Vossmerbaeumer U. Femtosecond laser penetrating keratoplasty with conical incisions and positional spikes. J Refract Surg. 2004. 20:397.31. Pfaeffl WA, Kunze M, Zenk U, et al. Predictive factors of femtosecond laser flap thickness measured by online optical coherence pachymetry subtraction in sub-Bowman keratomileusis. J Cataract Refract Surg. 2008. 34:1872–1880.32. Binder PS. Flap dimensions created with the IntraLase FS laser. J Cataract Refract Surg. 2004. 30:26–32.33. Sutton G, Hodge C. Accuracy and precision of LASIK flap thickness using the IntraLase femtosecond laser in 1000 consecutive cases. J Refract Surg. 2008. 24:802–806.34. Li Y, Shekhar R, Huang D. Corneal pachymetry mapping with high-speed optical coherence tomography. Ophthalmology. 2006. 113:792-9.e2.35. von Jagow B, Kohnen T. Corneal architecture of femtosecond laser and microkeratome flaps imaged by anterior segment optical coherence tomography. J Cataract Refract Surg. 2009. 35:35–41.36. Dawson DG, Grossniklaus HE, McCarey BE, Edelhauser HF. Biomechanical and wound healing characteristics of corneas after excimer laser keratorefractive surgery: is there a difference between advanced surface ablation and sub-Bowman's keratomileusis? J Refract Surg. 2008. 24:S90–S96.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Reproducibility of IntraLASIK Flap Thickness Measured with Optical Coherence Tomography
- The Consistency of Corneal Flap Thickness and Size in LASIK using the Innovatome Automatic Micro keratome
- The Analysis of Epithelial Ingrowth after LASIK Using a Femtosecond Laser
- The Change of Eyeball Contour and Factors Affecting Corneal Flap using Automated Microkeratome in LASIK
- Central Corneal Thickness Measured by Four Different Methods in Normal and Post-Femtosecond Laser-Assisted LASIK Eyes