Korean J Radiol.
2011 Feb;12(1):15-24. 10.3348/kjr.2011.12.1.15.
Diffusion and Perfusion Characteristics of MELAS (Mitochondrial Myopathy, Encephalopathy, Lactic Acidosis, and Stroke-Like Episode) in Thirteen Patients
- Affiliations
-
- 1Department of Radiology and Center for Imaging Science, Samsung Medical Center, Sungkyunkwan University, School of Medicine, Seoul 135-710, Korea.
- 2Department of Radiology, Inha University Hospital, Incheon 400-103, Korea. kanlim@inha.ac.kr
- 3Department of Neurology, Inha University Hospital, Incheon 400-103, Korea.
- KMID: 991678
- DOI: http://doi.org/10.3348/kjr.2011.12.1.15
Abstract
OBJECTIVE
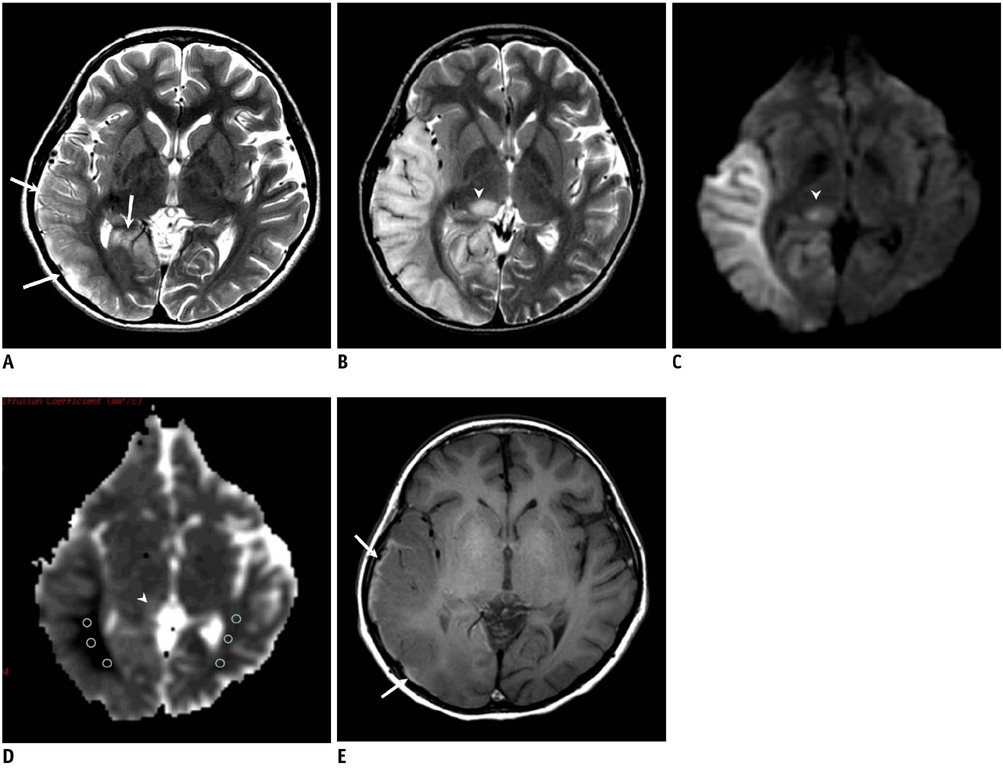
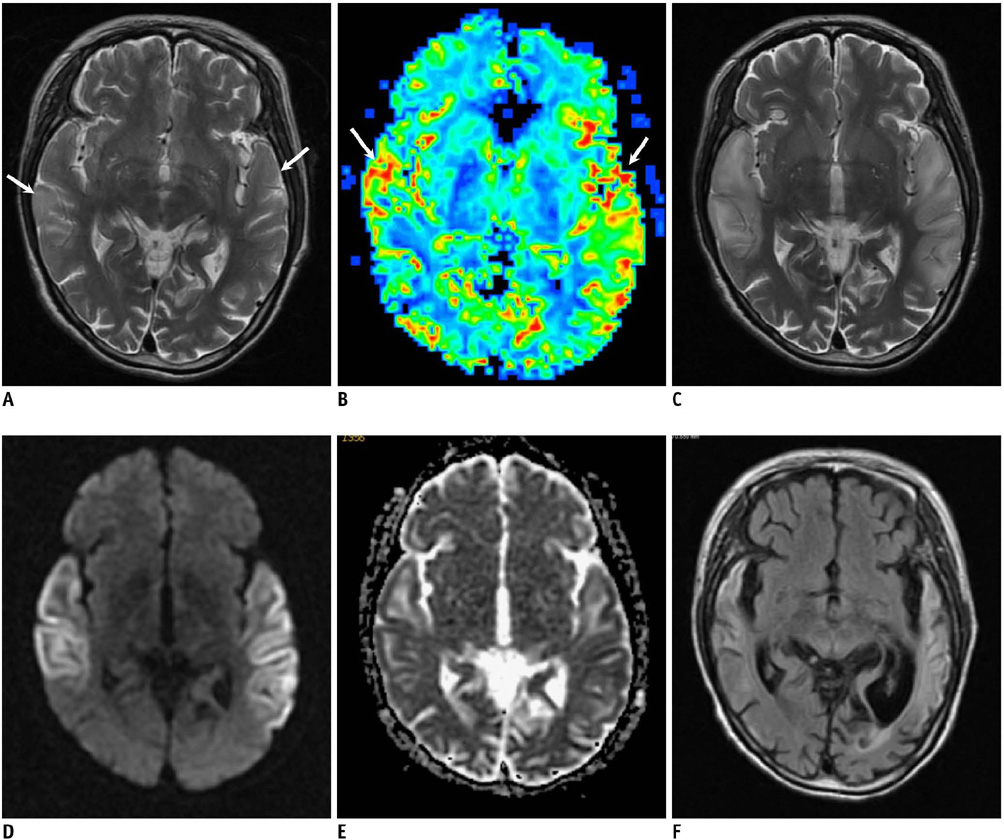
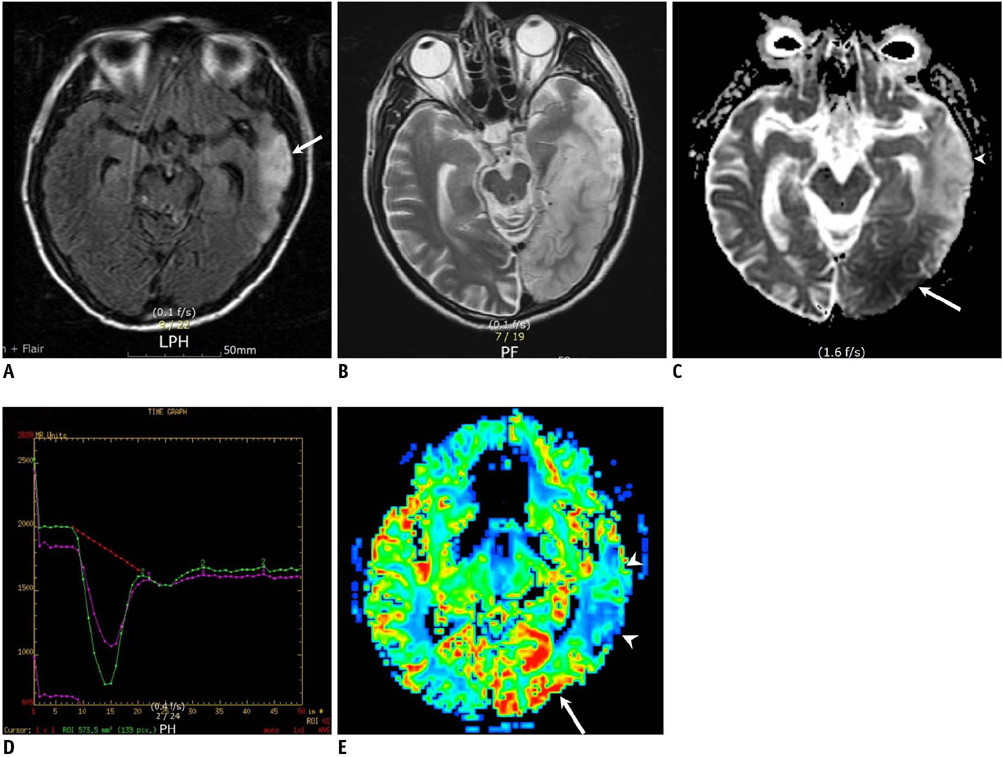
We analyzed the diffusion and perfusion characteristics of acute MELAS (mitochondrial myopathy, encephalopathy, lactic acidosis, and stroke-like episode) lesions in a large series to investigate the controversial changes of the apparent diffusion coefficient (ADC) that were reported in prior studies.
MATERIALS AND METHODS
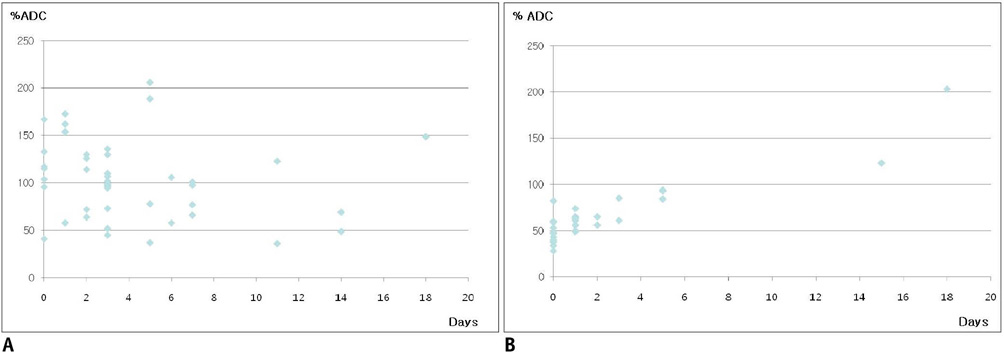
We analyzed 44 newly appearing lesions during 28 stroke-like episodes in 13 patients with MELAS. We performed a visual assessment of the MR images including the ADC and perfusion maps, comparison of the ADC between the normal and abnormal areas, comparison of % ADC between the 44 MELAS lesions and the 30 acute ischemic infarcts. In addition, the patterns of evolution on follow-up MR images were analyzed.
RESULTS
Decreased, increased, and normal ADCs were noted in 16 (36%), 16 (36%), and 12 (27%) lesions, respectively. The mean % ADC was 102 +/- 40.9% in the MELAS and 64 +/- 17.8% in the acute vascular infarcts (p < 0.001), while perfusion imaging demonstrated hyper-perfusion in six acute MELAS lesions. On follow-up images, resolution, progression, and tissue loss were noted in 10, 4, and 17 lesions, respectively.
CONCLUSION
The cytotoxic edema gradually evolves following an acute stroke-like episode in patients with MELAS, and this may overlap with hyper-perfusion and vasogenic edema. The edematous swelling may be reversible or it may evolve to encephalomalacia, suggesting irreversible damage.
MeSH Terms
Figure
Reference
-
1. Kim IO, Kim JH, Kim WS, Hwang YS, Yeon KM, Han MC. Mitochondrial myopathy-encephalopathy-lactic acidosis-and strokelike episodes (MELAS) syndrome: CT and MR findings in seven children. AJR Am J Roentgenol. 1996. 166:641–645.2. Ohama E, Ohara S, Ikuta F, Tanaka K, Nishizawa M, Miyatake T. Mitochondrial angiopathy in cerebral blood vessels of mitochondrial encephalomyopathy. Acta Neuropathol. 1987. 74:226–233.3. Iizuka T, Sakai F, Suzuki N, Hata T, Tsukahara S, Fukuda M, et al. Neuronal hyperexcitability in stroke-like episodes of MELAS syndrome. Neurology. 2002. 59:816–824.4. Schaefer PW, Buonanno FS, Gonzalez RG, Schwamm LH. Diffusion-weighted imaging discriminates between cytotoxic and vasogenic edema in a patient with eclampsia. Stroke. 1997. 28:1082–1085.5. Yoneda M, Maeda M, Kimura H, Fujii A, Katayama K, Kuriyama M. Vasogenic edema on MELAS: a serial study with diffusion-weighted MR imaging. Neurology. 1999. 53:2182–2184.6. Oppenheim C, Galanaud D, Samson Y, Sahel M, Dormont D, Wechsler B, et al. Can diffusion weighted magnetic resonance imaging help differentiate stroke from stroke-like events in MELAS? J Neurol Neurosurg Psychiatry. 2000. 69:248–250.7. Ohshita T, Oka M, Imon Y, Watanabe C, Katayama S, Yamaguchi S, et al. Serial diffusion-weighted imaging in MELAS. Neuroradiology. 2000. 42:651–656.8. Yonemura K, Hasegawa Y, Kimura K, Minematsu K, Yamaguchi T. Diffusion-weighted MR imaging in a case of mitochondrial myopathy, encephalopathy, lactic acidosis, and strokelike episodes. AJNR Am J Neuroradiol. 2001. 22:269–272.9. Kolb SJ, Costello F, Lee AG, White M, Wong S, Schwartz ED, et al. Distinguishing ischemic stroke from the stroke-like lesions of MELAS using apparent diffusion coefficient mapping. J Neurol Sci. 2003. 216:11–15.10. Abe K, Yoshimura H, Tanaka H, Fujita N, Hikita T, Sakoda S. Comparison of conventional and diffusion-weighted MRI and proton MR spectroscopy in patients with mitochondrial encephalomyopathy, lactic acidosis, and stroke-like events. Neuroradiology. 2004. 46:113–117.11. Jian-Ren L. Precipitation of stroke-like event by chickenpox in a child with MELAS syndrome. Neurol India. 2005. 53:323–325.12. Alemdar M, Iseri P, Selekler M, Budak F, Demirci A, Komsuoglu SS. MELAS presented with status epilepticus and Anton-Babinski syndrome; value of ADC mapping in MELAS. J Neuropsychiatry Clin Neurosci. 2007. 19:482–483.13. Ito H, Mori K, Harada M, Minato M, Naito E, Takeuchi M, et al. Serial brain imaging analysis of stroke-like episodes in MELAS. Brain Dev. 2008. 30:483–488.14. Wang XY, Noguchi K, Takashima S, Hayashi N, Ogawa S, Seto H. Serial diffusion-weighted imaging in a patient with MELAS and presumed cytotoxic oedema. Neuroradiology. 2003. 45:640–643.15. Iizuka T, Sakai F, Kan S, Suzuki N. Slowly progressive spread of the stroke-like lesions in MELAS. Neurology. 2003. 61:1238–1244.16. Mizrachi IB, Gomez-Hassan D, Blaivas M, Trobe JD. Pitfalls in the diagnosis of mitochondrial encephalopathy with lactic acidosis and stroke-like episodes. J Neuroophthalmol. 2006. 26:38–43.17. Bi WL, Baehring JM, Lesser RL. Evolution of brain imaging abnormalities in mitochondrial encephalomyopathy with lactic acidosis and stroke-like episodes. J Neuroophthalmol. 2006. 26:251–256.18. Tzoulis C, Bindoff LA. Serial diffusion imaging in a case of mitochondrial encephalomyopathy, lactic acidosis, and stroke-like episodes. Stroke. 2009. 40:e15–e17.19. Sheerin F, Pretorius PM, Briley D, Meagher T. Differential diagnosis of restricted diffusion confined to the cerebral cortex. Clin Radiol. 2008. 63:1245–1253.20. Hasegawa Y, Formato JE, Latour LL, Gutierrez JA, Liu KF, Garcia JH, et al. Severe transient hypoglycemia causes reversible change in the apparent diffusion coefficient of water. Stroke. 1996. 27:1648–1655.21. Hasegawa D, Orima H, Fujita M, Nakamura S, Takahashi K, Ohkubo S, et al. Diffusion-weighted imaging in kainic acid-induced complex partial status epilepticus in dogs. Brain Res. 2003. 983:115–127.22. Bradley DP, Smith JM, Smith MI, Bockhorst KH, Papadakis NG, Hall LD, et al. Cortical spreading depression in the feline brain following sustained and transient stimuli studied using diffusion-weighted imaging. J Physiol. 2002. 544:39–56.23. Tsujikawa T, Yoneda M, Shimizu Y, Uematsu H, Toyooka M, Ikawa M, et al. Pathophysiologic evaluation of MELAS strokes by serially quantified MRS and CASL perfusion images. Brain Dev. 2010. 32:143–149.24. Clark JM, Marks MP, Adalsteinsson E, Spielman DM, Shuster D, Horoupian D, et al. MELAS: Clinical and pathologic correlations with MRI, xenon/CT, and MR spectroscopy. Neurology. 1996. 46:223–227.25. Ooiwa Y, Uematsu Y, Terada T, Nakai K, Itakura T, Komai N, et al. Cerebral blood flow in mitochondrial myopathy, encephalopathy, lactic acidosis, and strokelike episodes. Stroke. 1993. 24:304–309.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Myopathy, Encephalopathy, Lactic Acidosis and Stroke-Like Episodes (MEALS) Syndrome with Intracardiac Thrombus
- General Anesthesia with Sevoflurane for a Patient with MELAS (Mitochondrial Myopathy, Encephalopathy, Lactic Acidosis, Stroke-like Episodes) Syndrome: A case report
- Status Epilepticus as the Initial Manifestation of Mitochondrial Myopathy, Encephalopathy, Lactic Acidosis, and Stroke-Like Episodes Syndrome
- Vascular Hyperemia and Crossed Cerebellar Diaschisis in MELAS Patient Presented as Stroke-Like Episode and Seizure
- Wolff-Parkinson-White Syndrome in a Patient With Mitochondrial Encephalopathy, Lactic Acidosis and Stroke-Like Episodes Syndrome