Korean J Radiol.
2001 Mar;2(1):28-36. 10.3348/kjr.2001.2.1.28.
Contrast Media in Abdominal Computed Tomography: Optimization of Delivery Methods
- Affiliations
-
- 1Seoul Natl Univ Hosp,Dept Radiol Chongno Gu,28 Yongon Dong, Seoul 110744, South Korea.
- KMID: 754120
- DOI: http://doi.org/10.3348/kjr.2001.2.1.28
Abstract
OBJECTIVE
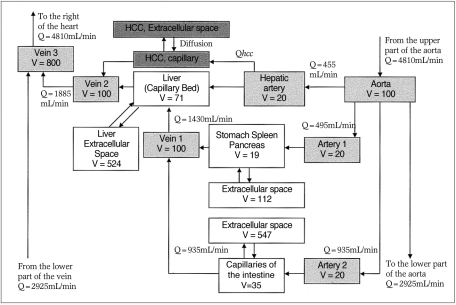
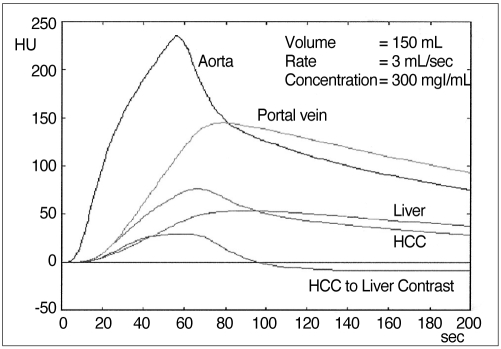
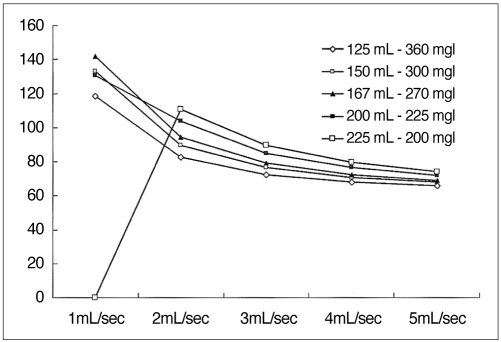
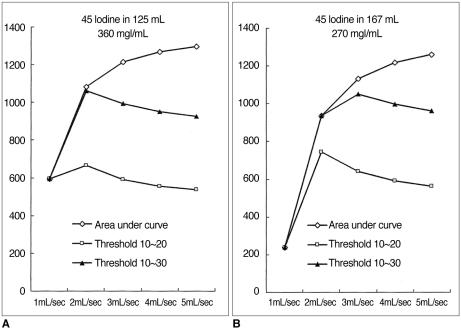
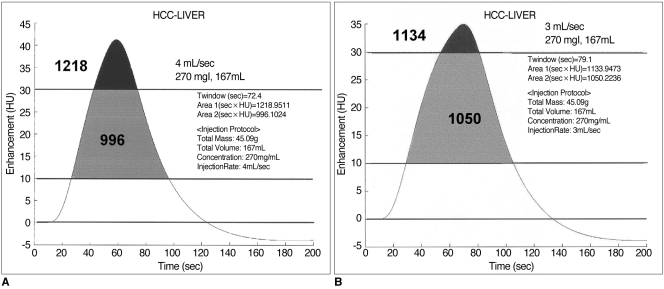
To provide a systematic overview of the effects of various parameters on contrast enhancement within the same population, an animal experiment as well as a computer-aided simulation study was performed. MATERIALS AND METHODS: In an animal experiment, single-level dynamic CT through the liver was performed at 5-second intervals just after the injection of contrast medium for 3 minutes. Combinations of three different amounts (1, 2, 3 mL/kg), concentrations (150, 200, 300 mgI/mL), and injection rates (0.5, 1, 2 mL/sec) were used. The CT number of the aorta (A), portal vein (P) and liver (L) was measured in each image, and time-attenuation curves for A, P and L were thus obtained. The degree of maximum enhancement (Imax) and time to reach peak enhancement (Tmax) of A, P and L were determined, and times to equilibrium (Teq) were analyzed. In the computed-aided simulation model, a program based on the amount, flow, and diffusion coefficient of body fluid in various compartments of the human body was designed. The input variables were the concen-trations, volumes and injection rates of the contrast media used. The program generated the time-attenuation curves of A, P and L, as well as liver-to-hepatocel-lular carcinoma (HCC) contrast curves. On each curve, we calculated and plotted the optimal temporal window (time period above the lower threshold, which in this experiment was 10 Hounsfield units), the total area under the curve above the lower threshold, and the area within the optimal range. RESULTS: A. Animal Experiment: At a given concentration and injection rate, an increased volume of contrast medium led to increases in Imax A, P and L. In addition, Tmax A, P, L and Teq were prolonged in parallel with increases in injection time The time-attenuation curve shifted upward and to the right. For a given volume and injection rate, an increased concentration of contrast medium increased the degree of aortic, portal and hepatic enhancement, though Tmax A, P and L remained the same. The time-attenuation curve shifted upward. For a given volume and concentration of contrast medium, changes in the injection rate had a prominent effect on aortic enhancement, and that of the portal vein and hepatic parenchyma also showed some increase, though the effect was less prominent. A increased in the rate of contrast injection led to shifting of the time enhancement curve to the left and upward. B. Computer Simulation: At a faster injection rate, there was minimal change in the degree of hepatic attenuation, though the duration of the optimal temporal window decreased. The area between 10 and 30 HU was greatest when contrast media was delivered at a rate of 2 -3 mL/sec. Although the total area under the curve increased in proportion to the injection rate, most of this increase was above the upper threshould and thus the temporal window was narrow and the optimal area decreased. CONCLUSION: Increases in volume, concentration and injection rate all resulted in improved arterial enhancement. If cost was disregarded, increasing the injection volume was the most reliable way of obtaining good quality enhancement. The optimal way of delivering a given amount of contrast medium can be calculated using a computer-based mathematical model.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Optimal scan delay depending on contrast material injection duration in abdominal multi-phase computed tomography of pancreas and liver in normal Beagle dogs
Soo-Young Choi, In Lee, Ji-Won Seo, Hyun-Young Park, Ho-Jung Choi, Young-Won Lee
J Vet Sci. 2016;17(4):555-561. doi: 10.4142/jvs.2016.17.4.555.Three-dimensional CT angiography of the canine hepatic vasculature
Yucheol Jeong, Changyun Lim, Sunkyoung Oh, Joohyun Jung, Jinhwa Chang, Junghee Yoon, Mincheol Choi
J Vet Sci. 2008;9(4):407-413. doi: 10.4142/jvs.2008.9.4.407.
Reference
-
1. Cox IH, Foley WD, Hoffman RG. Right window for dynamic hepatic CT. Radiology. 1991; 181:18–21. PMID: 1887031.
Article2. Heiken JP, Brink JA, McClennan BL, et al. Dynamic contrast-enhanced CT of the liver: comparison of contrast medium injection rates and uniphasic and biphasic injection protocols. Radiology. 1993; 187:327–331. PMID: 8475268.
Article3. Foley WD, Hoffmann RG, Quiroz FA, Kahn CE, Perret RS. Hepatic helical CT: contrast material injection protocol. Radiology. 1994; 192:367–371. PMID: 8029399.
Article4. Birnbaum BA, Jacobs JE, Yin D. Hepatic enhancement during helical CT: a comparison of moderate rate uniphasic and biphasic contrast injection protocols. AJR. 1995; 165:853–858. PMID: 7676980.
Article5. Kim T, Murakami T, Takahashi S, et al. Effects of injection rates of contrast material on arterial hepatic CT. AJR. 1998; 171:429–432. PMID: 9694469.6. Garcia PA, Bonaldi VM, Bret PM, et al. Effect of rate of contrast medium injection on hepatic enhancement at CT. Radiology. 1996; 199:185–189. PMID: 8633144.
Article7. Han JK, Kim AY, Lee KY, et al. Factors influencing vascular and hepatic enhancement at CT: experimental study of injection protocol using a canine model. J Comput Assist Tomogr. 2000; 24:400–406. PMID: 10864075.9. Bae KT, Heiken JP, Brink JA. Aortic and hepatic contrast medium enhancement at CT. Part I: Prediction with a computer model. Radiology. 1998; 207:647–655. PMID: 9609886.
Article10. Kim S, Kim JH, Han JK, Lee KH, Min B. Prediction of optimal injection protocol for tumor detection in contrast-enhanced dynamic hepatic CT using simulation of lesion-to-liver contrast enhancement. Comput Med Imaging Graph. 2000; 24:317–327. PMID: 10940609.11. Chambers TP, Baron RL, Lush RM. Hepatic CT enhancement. Part I: Alteration in the volume of contrast material within the same patients. Radiology. 1994; 193:513–517. PMID: 7972770.12. Chambers TP, Baron RL, Lush RM. Hepatic CT enhancement. Part II: Alteration in the volume and rate of injection within the same patients. Radiology. 1994; 193:518–522. PMID: 7972771.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Innovation and Optimization of Contrast Media Administration in Computed Tomography
- Preparative fasting before contrast-enhanced computed tomography
- Transient Orbitofacial Angioedema due to Intravenous Iodinated Contrast Media During Computed Tomography: CT Findings
- Compartment Syndrome of the Upper Extremity Induced by Extravasation of Contrast Media after Computed Tomography: A Case Report
- Computed Tomographic Dacfyocystography using Rayvist(R)