Cardiovasc Prev Pharmacother.
2025 Apr;7(2):21-27. 10.36011/cpp.2025.7.e6.
Clinical and preclinical obesity: cardiovascular implications of a new diagnostic paradigm
- Affiliations
-
- 1Department of Family Medicine, Korea University Guro Hospital, Korea University College of Medicine, Seoul, Korea
- KMID: 2567378
- DOI: http://doi.org/10.36011/cpp.2025.7.e6
Abstract
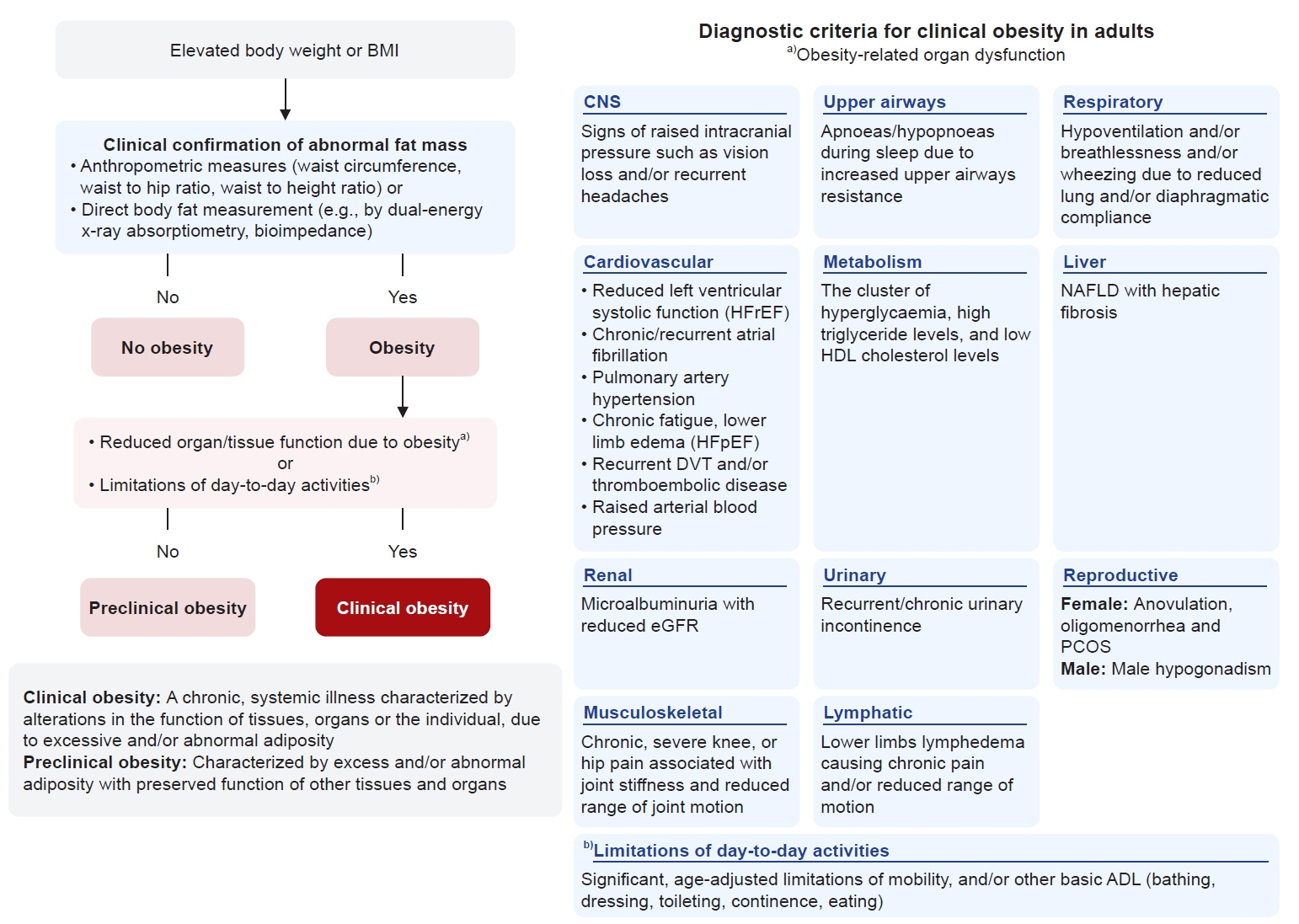
- The traditional definition of obesity, relying solely on body mass index, inadequately captures individual health status and is insufficient for guiding therapeutic interventions. In January 2025, The Lancet Diabetes & Endocrinology Commission proposed a paradigm-shifting redefinition that introduces the concepts of “clinical obesity” and “preclinical obesity.” Clinical obesity is defined as a chronic, systemic illness characterized by excess adiposity resulting in functional impairments in tissues, organs, or overall individual health. In contrast, preclinical obesity involves excess adiposity without current functional impairment. This review examines the significance of this new diagnostic paradigm for cardiovascular disease prevention and risk assessment. From a cardiovascular perspective, the new framework offers several advantages: it facilitates personalized intervention strategies based on individual risk profiles, refines cardiovascular risk assessments by incorporating body fat distribution and functional parameters, promotes more efficient resource allocation, and shifts treatment goals toward functional improvements beyond mere weight loss. Although further research is required to evaluate practical implementation and long-term outcomes, this novel approach represents a substantial advancement in obesity management and cardiovascular disease prevention.
Keyword
Figure
Reference
-
1. Huh Y, Nam GE. Overcoming increasing morbid obesity in Korea. J Obes Metab Syndr. 2021; 30:77–80. DOI: 10.7570/jomes21052. PMID: 34187966.
Article2. Rubino F, Cummings DE, Eckel RH, Cohen RV, Wilding JP, Brown WA, et al. Definition and diagnostic criteria of clinical obesity. Lancet Diabetes Endocrinol. 2025; 13:221–62. DOI: 10.1016/s2213-8587(24)00316-4. PMID: 39824205.
Article3. Gomez-Ambrosi J, Silva C, Galofre JC, Escalada J, Santos S, Millan D, et al. Body mass index classification misses subjects with increased cardiometabolic risk factors related to elevated adiposity. Int J Obes (Lond). 2012; 36:286–94. DOI: 10.1038/ijo.2011.100. PMID: 21587201.
Article4. Romero-Corral A, Somers VK, Sierra-Johnson J, Thomas RJ, Collazo-Clavell ML, Korinek J, et al. Accuracy of body mass index in diagnosing obesity in the adult general population. Int J Obes (Lond). 2008; 32:959–66. DOI: 10.1038/ijo.2008.11. PMID: 18283284.
Article5. Despres JP. Body fat distribution and risk of cardiovascular disease: an update. Circulation. 2012; 126:1301–13. DOI: 10.1161/circulationaha.111.067264. PMID: 22949540.6. Ross R, Neeland IJ, Yamashita S, Shai I, Seidell J, Magni P, et al. Waist circumference as a vital sign in clinical practice: a consensus statement from the IAS and ICCR Working Group on Visceral Obesity. Nat Rev Endocrinol. 2020; 16:177–89. DOI: 10.1038/s41574-019-0310-7. PMID: 32020062.
Article7. Czernichow S, Kengne AP, Stamatakis E, Hamer M, Batty GD. Body mass index, waist circumference and waist-hip ratio: which is the better discriminator of cardiovascular disease mortality risk? Evidence from an individual-participant meta-analysis of 82 864 participants from nine cohort studies. Obes Rev. 2011; 12:680–7. DOI: 10.1111/j.1467-789x.2011.00879.x. PMID: 21521449.8. Dale CE, Fatemifar G, Palmer TM, White J, Prieto-Merino D, Zabaneh D, et al. Causal associations of adiposity and body fat distribution with coronary heart disease, stroke subtypes, and type 2 diabetes mellitus: a Mendelian randomization analysis. Circulation. 2017; 135:2373–88. DOI: 10.1161/circulationaha.116.026560. PMID: 28500271.
Article9. Chait A, den Hartigh LJ. Adipose tissue distribution, inflammation and its metabolic consequences, including diabetes and cardiovascular disease. Front Cardiovasc Med. 2020; 7:22. DOI: 10.3389/fcvm.2020.00022. PMID: 32158768.
Article10. Garvey WT, Kwon S, Zheng D, Shaughnessy S, Wallace P, Hutto A, et al. Effects of insulin resistance and type 2 diabetes on lipoprotein subclass particle size and concentration determined by nuclear magnetic resonance. Diabetes. 2003; 52:453–62. DOI: 10.2337/diabetes.52.2.453. PMID: 12540621.
Article11. Lear SA, Humphries KH, Kohli S, Birmingham CL. The use of BMI and waist circumference as surrogates of body fat differs by ethnicity. Obesity (Silver Spring). 2007; 15:2817–24. DOI: 10.1038/oby.2007.334. PMID: 18070773.
Article12. Kim MK, Han K, Kwon HS, Song KH, Yim HW, Lee WC, et al. Normal weight obesity in Korean adults. Clin Endocrinol (Oxf). 2014; 80:214–20. DOI: 10.1111/cen.12162. PMID: 23362933.13. Rhee EJ, Lee MK, Kim JD, Jeon WS, Bae JC, Park SE, et al. Metabolic health is a more important determinant for diabetes development than simple obesity: a 4-year retrospective longitudinal study. PLoS One. 2014; 9:e98369. DOI: 10.1371/journal.pone.0098369. PMID: 24870949.
Article14. WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004; 363:157–63. DOI: 10.1016/s0140-6736(03)15268-3. PMID: 14726171.15. Deurenberg P, Deurenberg-Yap M, Guricci S. Asians are different from Caucasians and from each other in their body mass index/body fat per cent relationship. Obes Rev. 2002; 3:141–6. DOI: 10.1046/j.1467-789x.2002.00065.x. PMID: 12164465.
Article16. Emerging Risk Factors Collaboration, Wormser D, Kaptoge S, Di Angelantonio E, Wood AM, Pennells L, et al. Separate and combined associations of body-mass index and abdominal adiposity with cardiovascular disease: collaborative analysis of 58 prospective studies. Lancet. 2011; 377:1085–95. DOI: 10.1016/s0140-6736(11)60105-0. PMID: 21397319.
Article17. Powell-Wiley TM, Poirier P, Burke LE, Despres JP, Gordon-Larsen P, Lavie CJ, et al. Obesity and cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2021; 143:e984–1010. DOI: 10.1161/cir.0000000000000973. PMID: 33882682.
Article18. Zhou Z, Parra-Soto S, Boonpor J, Petermann-Rocha F, Welsh P, Mark PB, et al. Exploring the underlying mechanisms linking adiposity and cardiovascular disease: a prospective cohort study of 404,332 UK biobank participants. Curr Probl Cardiol. 2023; 48:101715. DOI: 10.1016/j.cpcardiol.2023.101715. PMID: 37004891.
Article19. Khan SS, Ning H, Wilkins JT, Allen N, Carnethon M, Berry JD, et al. Association of body mass index with lifetime risk of cardiovascular disease and compression of morbidity. JAMA Cardiol. 2018; 3:280–7. DOI: 10.1001/jamacardio.2018.0022. PMID: 29490333.
Article20. Sattar N, Deanfield J, Delles C. Impact of intentional weight loss in cardiometabolic disease: what we know about timing of benefits on differing outcomes? Cardiovasc Res. 2024; 119:e167–71. DOI: 10.1093/cvr/cvac186. PMID: 36683167.
Article21. Neeland IJ, Poirier P, Despres JP. Cardiovascular and metabolic heterogeneity of obesity: clinical challenges and implications for management. Circulation. 2018; 137:1391–406. DOI: 10.1161/circulationaha.117.029617. PMID: 29581366.
Article22. Borlaug BA, Jensen MD, Kitzman DW, Lam CS, Obokata M, Rider OJ. Obesity and heart failure with preserved ejection fraction: new insights and pathophysiological targets. Cardiovasc Res. 2023; 118:3434–50. DOI: 10.1093/cvr/cvac120. PMID: 35880317.
Article23. Kenchaiah S, Evans JC, Levy D, Wilson PW, Benjamin EJ, Larson MG, et al. Obesity and the risk of heart failure. N Engl J Med. 2002; 347:305–13. DOI: 10.1056/nejmoa020245. PMID: 12151467.
Article24. Obokata M, Reddy YN, Pislaru SV, Melenovsky V, Borlaug BA. Evidence supporting the existence of a distinct obese phenotype of heart failure with preserved ejection fraction. Circulation. 2017; 136:6–19. DOI: 10.1161/circulationaha.116.026807. PMID: 28381470.
Article25. van Woerden G, Gorter TM, Westenbrink BD, Willems TP, van Veldhuisen DJ, Rienstra M. Epicardial fat in heart failure patients with mid-range and preserved ejection fraction. Eur J Heart Fail. 2018; 20:1559–66. DOI: 10.1002/ejhf.1283. PMID: 30070041.
Article26. Kosiborod MN, Abildstrom SZ, Borlaug BA, Butler J, Rasmussen S, Davies M, et al. Semaglutide in patients with heart failure with preserved ejection fraction and obesity. N Engl J Med. 2023; 389:1069–84. DOI: 10.1056/nejmoa2306963. PMID: 37622681.27. Kitzman DW, Brubaker P, Morgan T, Haykowsky M, Hundley G, Kraus WE, et al. Effect of caloric restriction or aerobic exercise training on peak oxygen consumption and quality of life in obese older patients with heart failure with preserved ejection fraction: a randomized clinical trial. JAMA. 2016; 315:36–46. DOI: 10.1001/jama.2015.17346. PMID: 26746456.
Article28. Husain M, Birkenfeld AL, Donsmark M, Dungan K, Eliaschewitz FG, Franco DR, et al. Oral semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med. 2019; 381:841–51. DOI: 10.1056/nejmoa1901118. PMID: 31185157.
Article29. Marso SP, Bain SC, Consoli A, Eliaschewitz FG, Jodar E, Leiter LA, et al. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med. 2016; 375:1834–44. DOI: 10.1056/nejmoa1607141. PMID: 27633186.
Article30. Lincoff AM, Brown-Frandsen K, Colhoun HM, Deanfield J, Emerson SS, Esbjerg S, et al. Semaglutide and cardiovascular outcomes in obesity without diabetes. N Engl J Med. 2023; 389:2221–32. DOI: 10.1056/nejmoa2307563. PMID: 37952131.
Article31. Gerstein HC, Colhoun HM, Dagenais GR, Diaz R, Lakshmanan M, Pais P, et al. Dulaglutide and cardiovascular outcomes in type 2 diabetes (REWIND): a double-blind, randomised placebo-controlled trial. Lancet. 2019; 394:121–30. DOI: 10.1016/s0140-6736(19)31149-3. PMID: 31189511.32. Drucker DJ. The cardiovascular biology of glucagon-like peptide-1. Cell Metab. 2016; 24:15–30. DOI: 10.1016/j.cmet.2016.06.009. PMID: 27345422.
Article33. Bluher M. Obesity: global epidemiology and pathogenesis. Nat Rev Endocrinol. 2019; 15:288–98. DOI: 10.1038/s41574-019-0176-8. PMID: 30814686.
Article34. Lavie CJ, Laddu D, Arena R, Ortega FB, Alpert MA, Kushner RF. Healthy weight and obesity prevention: JACC Health Promotion Series. J Am Coll Cardiol. 2018; 72:1506–31. DOI: 10.1016/j.jacc.2018.08.1037. PMID: 30236314.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Metabolic and Cardiovascular Implications of a Metabolically Healthy Obesity Phenotype
- Growth and Puberty in Obese Children and Implications of Body Composition
- Understanding Obesity-Related High Output Heart Failure and Its Implications
- The Influence of Obesity and Metabolic Health on Vascular Health
- The Transformative Impact of New Anti-Obesity Medications: A Paradigm Shift in Medical Practice?