Korean J Gastroenterol.
2024 Apr;83(4):167-171. 10.4166/kjg.2024.030.
Successful Transcatheter Arterial Embolization of Abdominal Wall Hematoma from the Left Deep Circumflex Iliac Artery after Abdominal Paracentesis in a Patient with Liver Cirrhosis: Case Report and Literature Review
- Affiliations
-
- 1Departments of Internal Medicine, Chonnam National University Medical School, Gwangju, Korea
- 2Departments of Radiology, Chonnam National University Medical School, Gwangju, Korea
- KMID: 2555651
- DOI: http://doi.org/10.4166/kjg.2024.030
Abstract
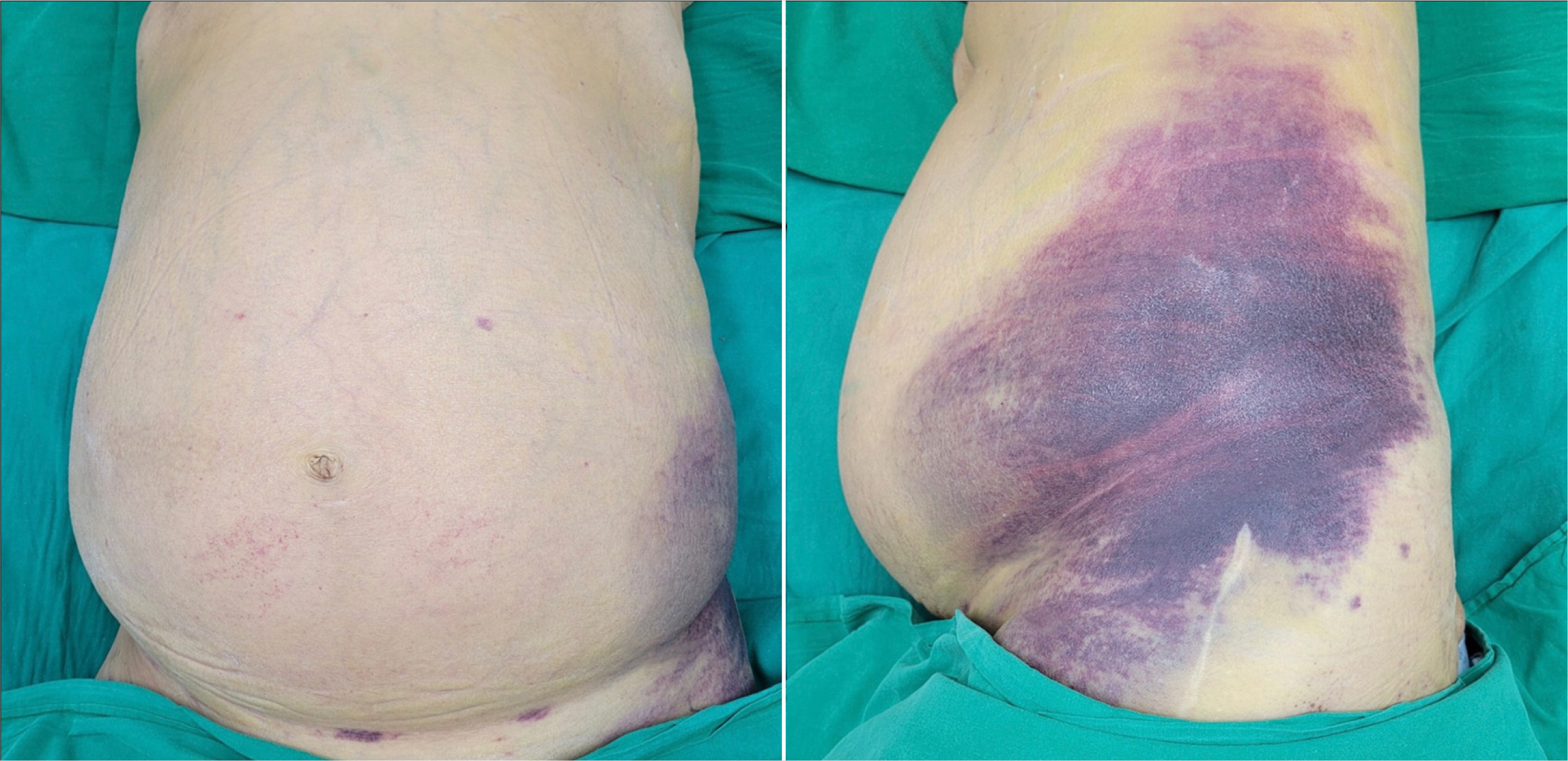
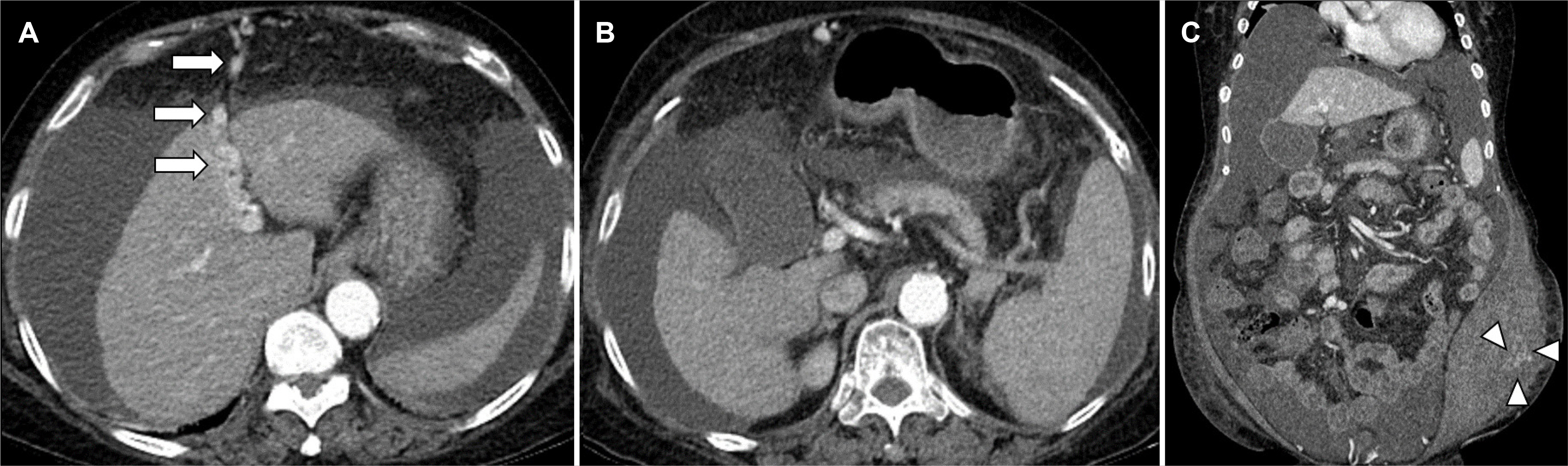
- The occurrence of an abdominal wall hematoma caused by abdominal paracentesis in patients with liver cirrhosis is rare. This paper presents a case of an abdominal wall hematoma caused by abdominal paracentesis in a 67-year-old woman with liver cirrhosis with a review of the relevant literature. Two days prior, the patient underwent abdominal paracentesis for symptom relief for refractory ascites at a local clinic. Upon admission, a physical examination revealed purpuric patches with swelling and mild tenderness in the left lower quadrant of the abdominal wall. Abdominal computed tomography revealed advanced liver cirrhosis with splenomegaly, tortuous dilatation of the para-umbilical vein, a large volume of ascites, and a large acute hematoma at the left lower quadrant of the abdominal wall. An external iliac artery angiogram showed the extravasation of contrast media from the left deep circumflex iliac artery. Embolization of the target arterial branches using N-butyl-2-cyanoacrylate was then performed, and the bleeding was stopped. The final diagnosis was an abdominal wall hematoma from the left deep circumflex iliac artery after abdominal paracentesis in a patient with liver cirrhosis.
Keyword
Figure
Reference
-
1. GBD 2017 Cirrhosis Collaborators. The global, regional, and national burden of cirrhosis by cause in 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol. 2020; 5:245–266. DOI: 10.1016/S2468-1253(19)30349-8. PMID: 31981519.2. Huang DQ, Terrault NA, Tacke F, et al. 2023; Global epidemiology of cirrhosis- aetiology, trends and predictions. Nat Rev Gastroenterol Hepatol. 20:388–398. DOI: 10.1038/s41575-023-00759-2. PMID: 36977794. PMCID: PMC10043867.
Article3. Jagdish RK, Roy A, Kumar K, et al. 2023; Pathophysiology and management of liver cirrhosis: from portal hypertension to acute-onchronic liver failure. Front Med (Lausanne). 10:1060073. DOI: 10.3389/fmed.2023.1060073. PMID: 37396918. PMCID: PMC10311004.
Article4. Tapper EB, Parikh ND. 2023; Diagnosis and management of cirrhosis and its complications: A review. JAMA. 329:1589–1602. DOI: 10.1001/jama.2023.5997. PMID: 37159031.
Article5. Tonon M, Piano S. 2023; Cirrhosis and portal hypertension: How do we deal with ascites and its consequences. Med Clin North Am. 107:505–516. DOI: 10.1016/j.mcna.2022.12.004. PMID: 37001950.6. Chandel K, Rana S, Patel RK, Tripathy TP, Mukund A. 2022; Bedside USG-guided paracentesis - A technical note for beginners. J Med Ultrasound. 30:215–216. DOI: 10.4103/jmu.jmu_141_21. PMID: 36484053. PMCID: PMC9724473.
Article7. Sharzehi K, Jain V, Naveed A, Schreibman I. 2014; Hemorrhagic complications of paracentesis: a systematic review of the literature. Gastroenterol Res Pract. 2014:985141. DOI: 10.1155/2014/985141. PMID: 25580114. PMCID: PMC4280650.
Article8. Lin S, Wang M, Zhu Y, et al. 2015; Hemorrhagic complications following abdominal paracentesis in acute on chronic liver failure: A propensity score analysis. Medicine (Baltimore). 94:e2225. DOI: 10.1097/MD.0000000000002225. PMID: 26656363. PMCID: PMC5008508.9. Webster ST, Brown KL, Lucey MR, Nostrant TT. 1996; Hemorrhagic complications of large volume abdominal paracentesis. Am J Gastroenterol. 91:366–368.10. Rozen WM, Ashton MW, Taylor GI. 2008; Reviewing the vascular supply of the anterior abdominal wall: redefining anatomy for increasingly refined surgery. Clin Anat. 21:89–98. DOI: 10.1002/ca.20585. PMID: 18189276.
Article11. Konerding MA, Gaumann A, Shumsky A, Schlenger K, Hockel M. 1997; The vascular anatomy of the inner anterior abdominal wall with special reference to the transversus and rectus abdominis musculoperitoneal (TRAMP) composite flap for vaginal reconstruction. Plast Reconstr Surg. 99:705–710. discussion 711–712. DOI: 10.1097/00006534-199703000-00016. PMID: 9047190.
Article12. Thein T, Kreidler J, Stocker E, Herrmann M. 1997; Morphology and blood supply of the iliac crest applied to jaw reconstruction. Surg Radiol Anat. 19:217–225. DOI: 10.1007/BF01627860. PMID: 9381326.
Article13. Murthy SV, Hussain ST, Gupta S, Thulkar S, Seenu V. 2002; Pseudoaneurysm of inferior epigastric artery following abdominal paracentesis. Indian J Gastroenterol. 21:197–198.14. Kalantari J, Nashed MH, Smith JC. 2019; Post paracentesis deep circumflex iliac artery injury identified at angiography, an underreported complication. CVIR Endovasc. 2:24. DOI: 10.1186/s42155-019-0068-y. PMID: 32026994. PMCID: PMC6966403.
Article15. Sakai H, Sheer TA, Mendler MH, Runyon BA. 2005; Choosing the location for non-image guided abdominal paracentesis. Liver Int. 25:984–986. DOI: 10.1111/j.1478-3231.2005.01149.x. PMID: 16162157.
Article16. Rimola J, Perendreu J, Falcó J, Fortuño JR, Massuet A, Branera J. 2007; Percutaneous arterial embolization in the management of rectus sheath hematoma. AJR Am J Roentgenol. 188:W497–502. DOI: 10.2214/AJR.06.0861. PMID: 17515337.
Article17. Day RW, Huettl EA, Naidu SG, Eversman WG, Douglas DD, O'Donnell ME. 2014; Successful coil embolization of circumflex iliac artery pseudoaneurysms following paracentesis. Vasc Endovascular Surg. 48:262–266. DOI: 10.1177/1538574413518115. PMID: 24399129.
Article18. Arnold C, Haag K, Blum HE, Rössle M. 1997; Acute hemoperitoneum after large-volume paracentesis. Gastroenterology. 113:978–982. DOI: 10.1016/S0016-5085(97)70210-5. PMID: 9287992.
Article19. Moon SN. 2019; Transarterial embolization for incorrectable abdominal wall hematoma after abdominal paracentesis. Korean J Intern Med. 34:938–939. DOI: 10.3904/kjim.2017.339. PMID: 29294599. PMCID: PMC6610186.
Article20. Kang JW, Kim YD, Hong JS, et al. 2012; [A case of lateral abdominal wall hematoma treated with transcatheter arterial embolization]. Korean J Gastroenterol. 59:185–188. Korean. DOI: 10.4166/kjg.2012.59.2.185. PMID: 22387839.
Article21. Park YJ, Lee SY, Kim SH, Kim IH, Kim SW, Lee SO. 2011; Transcatheter coil embolization of the inferior epigastric artery in a huge abdominal wall hematoma caused by paracentesis in a patient with liver cirrhosis. Korean J Hepatol. 17:233–237. DOI: 10.3350/kjhep.2011.17.3.233. PMID: 22102392. PMCID: PMC3304649.
Article22. Morita S, Tsuji T, Yamagiwa T, Otsuka H, Inokuchi S. 2009; Arterial embolization for traumatic lethal lateral abdominal wall hemorrhage in a liver cirrhosis patient. Chin J Traumatol. 12:250–251.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Lateral Abdominal Wall Hematoma Treated with Transcatheter Arterial Embolization
- Expanding Hematoma of the Abdominal Wall Caused by Spontaneous Rupture of a Deep Circumflex Iliac Artery:Report of A Case Treated by Coil Embolization
- Transcatheter coil embolization of the inferior epigastric artery in a huge abdominal wall hematoma caused by paracentesis in a patient with liver cirrhosis
- Successful Angiographic Embolization of Superficial Circumflex Iliac Artery Rupture Caused by Blunt Abdominal Trauma: A Case Report
- Transarterial embolization for incorrectable abdominal wall hematoma after abdominal paracentesis