J Korean Med Sci.
2024 May;39(17):e141. 10.3346/jkms.2024.39.e141.
Antibiotic Use in Korean Children Diagnosed With Acute Bronchiolitis: Analysis of the National Health Insurance Reimbursement Data
- Affiliations
-
- 1Department of Pediatrics, Eunpyeong St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Department of Pediatrics, Hangang Sacred Heart Hospital, College of Medicine, Hallym University, Seoul, Korea
- KMID: 2555494
- DOI: http://doi.org/10.3346/jkms.2024.39.e141
Abstract
- Background
Acute bronchiolitis, the most common lower respiratory tract infection in infants, is mostly caused by respiratory viruses. However, antibiotics are prescribed to about 25% of children with acute bronchiolitis. This inappropriate use of antibiotics for viral infections induces antibiotic resistance. This study aimed to determine the antibiotic prescription rate and the factors associated with antibiotic use in children with acute bronchiolitis in Korea, where antibiotic use and resistance rates are high.
Methods
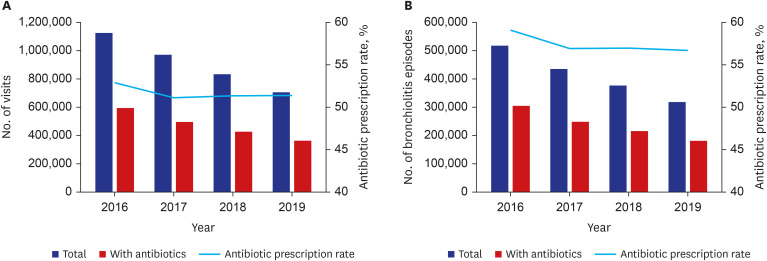
Healthcare data of children aged < 24 months who were diagnosed with acute bronchiolitis between 2016 and 2019 were acquired from the National Health Insurance system reimbursement claims data. Antibiotic prescription rates and associated factors were evaluated.
Results
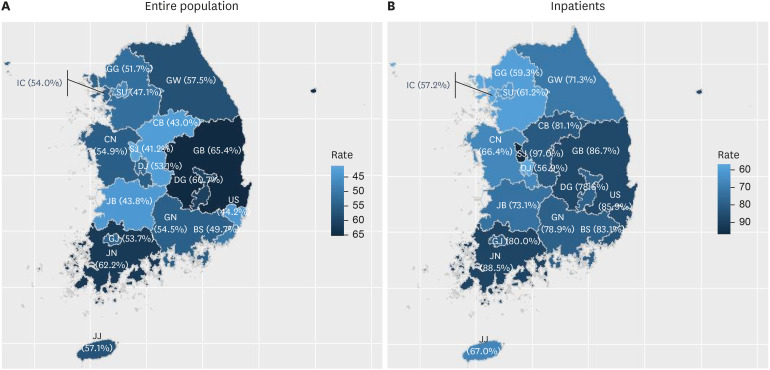
A total of 3,638,424 visits were analyzed. The antibiotic prescription rate was 51.8%, which decreased over time (P < 0.001). In the multivariate analysis, toddlers (vs. infants), non-capital areas (vs. capital areas), primary clinics and non-tertiary hospitals (vs. tertiary hospitals), inpatients (vs. outpatients), and non-pediatricians (vs. pediatricians) showed a significant association with antibiotic prescription (P < 0.001). Fourteen cities and provinces in the non-capital area exhibited a wide range of antibiotic prescription rates ranging from 41.2% to 65.4%, and five (35.7%) of them showed lower antibiotic prescription rates than that of the capital area.
Conclusion
In Korea, the high antibiotic prescription rates for acute bronchiolitis varied by patient age, region, medical facility type, clinical setting, and physician specialty. These factors should be considered when establishing strategies to promote appropriate antibiotic use.
Keyword
Figure
Reference
-
1. Ralston SL, Lieberthal AS, Meissner HC, Alverson BK, Baley JE, Gadomski AM, et al. Clinical practice guideline: the diagnosis, management, and prevention of bronchiolitis. Pediatrics. 2014; 134(5):e1474–e1502. PMID: 25349312.2. Dalziel SR, Haskell L, O’Brien S, Borland ML, Plint AC, Babl FE, et al. Bronchiolitis. Lancet. 2022; 400(10349):392–406. PMID: 35785792.3. Korean Centers for Disease Control and Prevention. Guidelines for the Antibiotic Use in Children with Lower Respiratory Tract Infections. Cheongju, Korea: Korean Centers for Disease Control and Prevention;2017.4. World Health Organization. Antimicrobial resistance. Updated 2023. Accessed January 3, 2024. https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance .5. Lovegrove MC, Geller AI, Fleming-Dutra KE, Shehab N, Sapiano MR, Budnitz DS. US emergency department visits for adverse drug events from antibiotics in children, 2011–2015. J Pediatric Infect Dis Soc. 2019; 8(5):384–391. PMID: 30137509.6. Samtani B, Gray N, Omand J, Keown-Stoneman C, Aglipay M, Birken C, et al. Early life antibiotic prescription for upper respiratory tract infection is associated with higher antibiotic use in childhood. J Pediatric Infect Dis Soc. 2022; 11(12):559–564. PMID: 36067011.7. Miller SA, Wu RKS, Oremus M. The association between antibiotic use in infancy and childhood overweight or obesity: a systematic review and meta-analysis. Obes Rev. 2018; 19(11):1463–1475. PMID: 30035851.8. McDonnell L, Gilkes A, Ashworth M, Rowland V, Harries TH, Armstrong D, et al. Association between antibiotics and gut microbiome dysbiosis in children: systematic review and meta-analysis. Gut Microbes. 2021; 13(1):1870402. PMID: 33651651.9. Choe YJ, Shin JY. Trends in the use of antibiotics among Korean children. Korean J Pediatr. 2019; 62(4):113–118. PMID: 30852884.10. Shin SM, Shin JY, Kim MH, Lee SH, Choi S, Park BJ. Prevalence of antibiotic use for pediatric acute upper respiratory tract infections in Korea. J Korean Med Sci. 2015; 30(5):617–624. PMID: 25931794.11. Health Insurance Review & Assessment service. Quality assessment. Updated 2023. Accessed January 3, 2024. https://www.hira.or.kr/ra/eval/getDiagEvlView.do?pgmid=HIRAA030004000100 .12. Snyder RL, King LM, Hersh AL, Fleming-Dutra KE. Unnecessary antibiotic prescribing in pediatric ambulatory care visits for bronchitis and bronchiolitis in the United States, 2006-2015. Infect Control Hosp Epidemiol. 2021; 42(5):612–615. PMID: 33059780.13. Kim JA, Yoon S, Kim LY, Kim DS. Towards actualizing the value potential of Korea Health Insurance Review and Assessment (HIRA) data as a resource for health research: Strengths, limitations, applications, and strategies for optimal use of HIRA data. J Korean Med Sci. 2017; 32(5):718–728. PMID: 28378543.14. HIRA Bigdata Open Portal. Updated 2023. Accessed January 4, 2024. https://opendata.hira.or.kr/home.do .15. World Health Organization. The WHO AWaRe (Access, Watch, Reserve) Antibiotic Book. Geneva, Switzerland: World Health Organization;2022.16. Korean Centers for Disease Control and Prevention. Guidelines for the Antibiotic Use in Children with Acute Upper Respiratory Tract Infections. Cheongju, Korea: Korean Centers for Disease Control and Prevention;2016.17. KOrean Statistical Information Service. Updated 2023. Accessed January 4, 2024. https://kosis.kr/eng/ .18. Chae J, Kim B, Kim DS. Changes in antibiotic consumption patterns after the implementation of the National Action Plan according to the Access, Watch, Reserve (AWaRe) classification system. Int J Infect Dis. 2022; 122:345–351. PMID: 35705118.19. Barbieri E, Cantarutti A, Cavagnis S, Cantarutti L, Baraldi E, Giaquinto C, et al. Impact of bronchiolitis guidelines publication on primary care prescriptions in the Italian pediatric population. NPJ Prim Care Respir Med. 2021; 31(1):15. PMID: 33741991.20. Oakley E, Brys T, Borland M, Neutze J, Phillips N, Krieser D, et al. Medication use in infants admitted with bronchiolitis. Emerg Med Australas. 2018; 30(3):389–397. PMID: 29573212.21. Obolski U, Kassem E, Na’amnih W, Tannous S, Kagan V, Muhsen K. Unnecessary antibiotic treatment of children hospitalised with respiratory syncytial virus (RSV) bronchiolitis: risk factors and prescription patterns. J Glob Antimicrob Resist. 2021; 27:303–308. PMID: 34718202.22. Johnson LW, Robles J, Hudgins A, Osburn S, Martin D, Thompson A. Management of bronchiolitis in the emergency department: impact of evidence-based guidelines? Pediatrics. 2013; 131(Suppl 1):S103–S109. PMID: 23457145.23. Parikh K, Hall M, Mittal V, Montalbano A, Mussman GM, Morse RB, et al. Establishing benchmarks for the hospitalized care of children with asthma, bronchiolitis, and pneumonia. Pediatrics. 2014; 134(3):555–562. PMID: 25136044.24. Papenburg J, Fontela PS, Freitas RR, Burstein B. Inappropriate antibiotic prescribing for acute bronchiolitis in US emergency departments, 2007–2015. J Pediatric Infect Dis Soc. 2019; 8(6):567–570. PMID: 30657968.25. Pittet LF, Glangetas A, Barazzone-Argiroffo C, Gervaix A, Posfay-Barbe KM, Galetto-Lacour A, et al. Factors associated with nonadherence to the American Academy of Pediatrics 2014 bronchiolitis guidelines: a retrospective study. PLoS One. 2023; 18(5):e0285626. PMID: 37200253.26. Wolf ER, Richards A, Lavallee M, Sabo RT, Schroeder AR, Schefft M, et al. Patient, provider, and health care system characteristics associated with overuse in bronchiolitis. Pediatrics. 2021; 148(4):e2021051345. PMID: 34556548.27. Fontoura-Matias J, Moreira-Sousa D, Freitas A, Azevedo I. Management of bronchiolitis in Portugal, 2000-2015: do guidelines have an impact? Pediatr Pulmonol. 2020; 55(1):198–205. PMID: 31456354.28. House SA, Marin JR, Hall M, Ralston SL. Trends over time in use of nonrecommended tests and treatments since publication of the American Academy of Pediatrics bronchiolitis guideline. JAMA Netw Open. 2021; 4(2):e2037356. PMID: 33587138.29. Zipursky A, Kuppermann N, Finkelstein Y, Zemek R, Plint AC, Babl FE, et al. International practice patterns of antibiotic therapy and laboratory testing in bronchiolitis. Pediatrics. 2020; 146(2):e20193684. PMID: 32661190.30. Huang IA, Jaing TH, Wu CT, Chang CJ, Hsia SH, Huang N. A tale of two systems: practice patterns of a single group of emergency medical physicians in Taiwan and China. BMC Health Serv Res. 2017; 17(1):642. PMID: 28893261.31. Florin TA, Byczkowski T, Ruddy RM, Zorc JJ, Test M, Shah SS. Variation in the management of infants hospitalized for bronchiolitis persists after the 2006 American Academy of Pediatrics bronchiolitis guidelines. J Pediatr. 2014; 165(4):786–792.e1. PMID: 25015578.32. Zetts RM, Stoesz A, Smith BA, Hyun DY. Outpatient antibiotic use and the need for increased antibiotic stewardship efforts. Pediatrics. 2018; 141(6):e20174124. PMID: 29793986.33. Hulscher ME, Grol RP, van der Meer JW. Antibiotic prescribing in hospitals: a social and behavioural scientific approach. Lancet Infect Dis. 2010; 10(3):167–175. PMID: 20185095.34. Guo S, Sun Q, Zhao X, Shen L, Zhen X. Prevalence and risk factors for antibiotic utilization in Chinese children. BMC Pediatr. 2021; 21(1):255. PMID: 34074254.35. Bond SE, Chubaty AJ, Adhikari S, Miyakis S, Boutlis CS, Yeo WW, et al. Outcomes of multisite antimicrobial stewardship programme implementation with a shared clinical decision support system. J Antimicrob Chemother. 2017; 72(7):2110–2118. PMID: 28333302.36. Knight J, Michal J, Milliken S, Swindler J. Effects of a remote antimicrobial stewardship program on antimicrobial use in a regional hospital system. Pharmacy (Basel). 2020; 8(1):41. PMID: 32188001.37. Montejo M, Paniagua N, Pijoan JI, Saiz-Hernando C, Castelo S, Martin V, et al. Reducing unnecessary treatment of bronchiolitis across a large regional health service in Spain. Pediatrics. 2022; 150(5):e2021053888. PMID: 36222087.38. van Houten CB, Naaktgeboren C, Buiteman BJM, van der Lee M, Klein A, Srugo I, et al. Antibiotic overuse in children with respiratory syncytial virus lower respiratory tract infection. Pediatr Infect Dis J. 2018; 37(11):1077–1081. PMID: 29601448.39. Guerrero-Del-Cueto F, Ramos-Fernandez JM, Leiva-Gea I, Reina-Moreno E, Ortiz-Ortigosa A, Carazo-Gallego B, et al. Bronchiolitis before and after the SARS-CoV-2 pandemic: twelve years of experience in a Spanish paediatric hospital. Pediatr Pulmonol. 2023; 58(4):1201–1209. PMID: 36653064.40. Titus MO, Wright SW. Prevalence of serious bacterial infections in febrile infants with respiratory syncytial virus infection. Pediatrics. 2003; 112(2):282–284. PMID: 12897274.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The process by which new health technology is listed for insurance coverage
- Policy alternatives of drug cost containment in health insurance
- Methods and Applications to estimate the Conversion Factor of Resource-based Relative Value Scale for Nurse-Midwife's Delivery Service in the National Health Insurance
- Trend of Antibiotic Use in Children with Acute Otitis Media in Korea
- A New Healthcare Policy in Korea Part 1: Expanded Reimbursement Coverage of Brain MRI, Brain/Neck MRA, and Head and Neck MRI by National Health Insurance