Korean J Schizophr Res.
2024 Apr;27(1):1-13. 10.16946/kjsr.2024.27.1.1.
A Review of Mobile App-Based Psychosocial Intervention for Personal and Clinical Recovery for People With Psychosis
- Affiliations
-
- 1Department of Clinical Psychology, Yong-In Mental Hospital, Yoingin, Korea
- 2WHO Collaborating Centre for Psychosocial Rehabilitation and Community Mental Health, Yoingin, Korea
- KMID: 2554836
- DOI: http://doi.org/10.16946/kjsr.2024.27.1.1
Abstract
Objectives
The social and economic costs of severe mental illness, including psychosis, are increasing, and methods to reduce costs such as a mobile app-based approach have been tried more than ever. This study aims to explore and analyze the methods that have been used in previous studies for mobile app-based psychosocial interventions for personal and clinical recovery of psychosis.
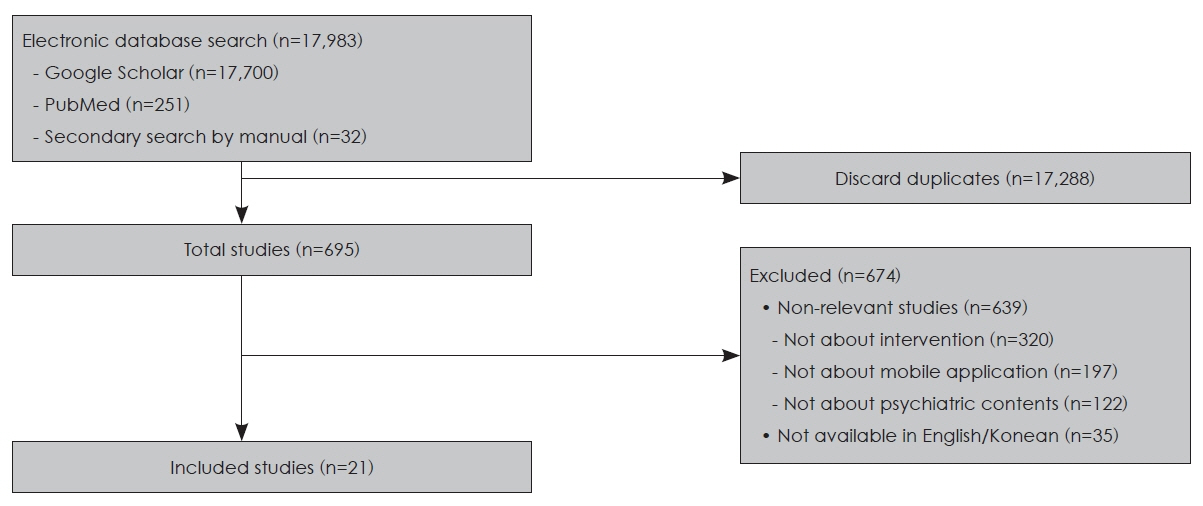
Methods
To identify mobile apps associated with psychosis, psychotic disorder, and other related terms, we searched for literature published from 2017 to 2023 (n=21). After classifying them into personal and clinical recovery, we qualitatively analyzed each study’s topics, objectives, measurement tools, results, and other aspects.
Results
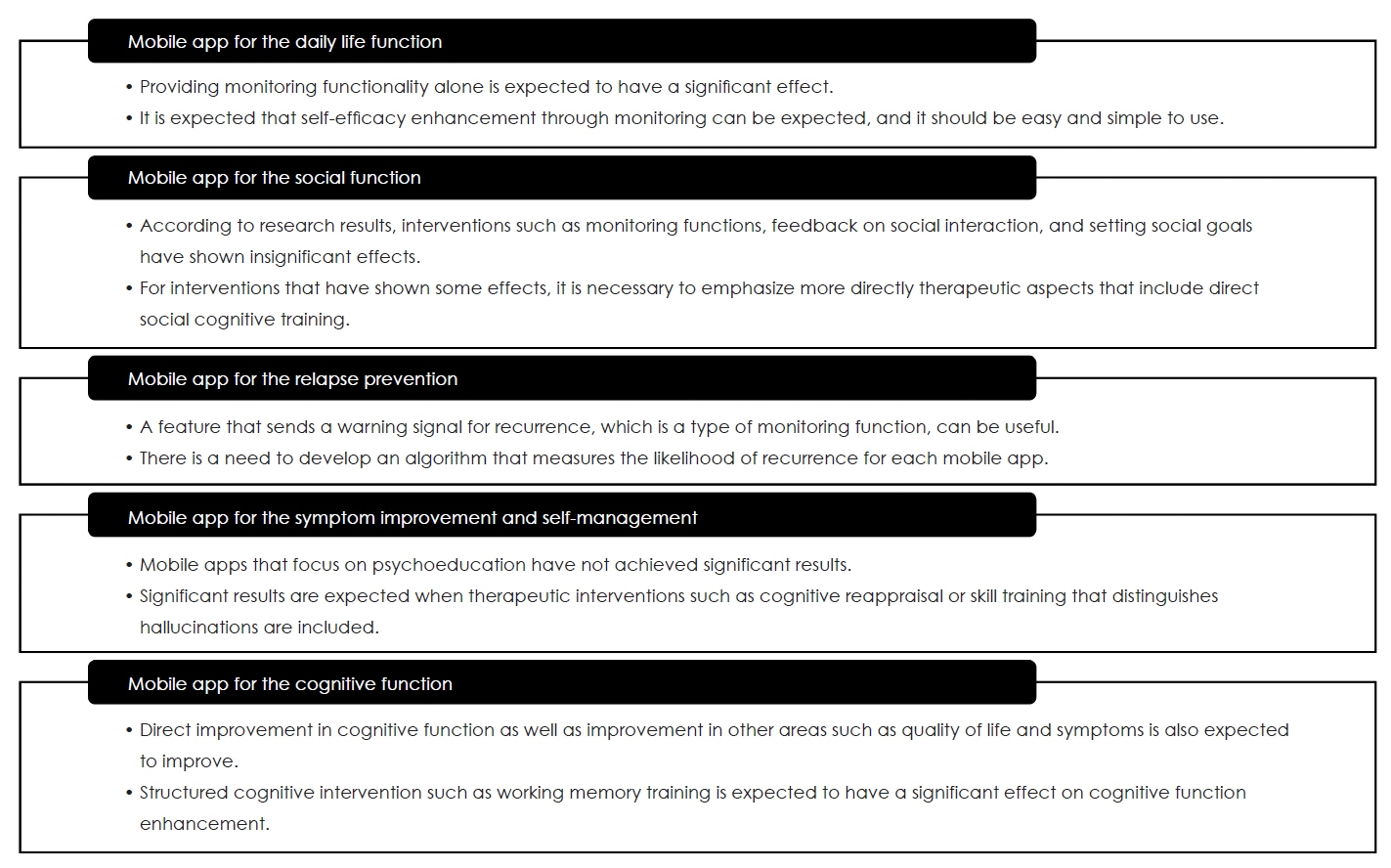
For personal recovery, the focus was mainly on improving daily living, self-management, and cognitive and social function improvement, and for clinical recovery, the focus was mainly on preventing symptom recurrence and managing symptoms. Mobile apps for improving daily living functions, cognitive functions, and relapse prevention have significant effects. While mobile apps for improving social function and symptom management mainly reported smaller effects.
Conclusion
The results of this study suggest that mobile app-based psychosocial interventions for personal and clinical recovery of psychosis are likely to be utilized. Finally, the significance and limitations of the studies were discussed.
Keyword
Figure
Reference
-
1. Korean National Mental Health Center. National Mental Health Statistics;2021.2. König H, König HH, Gallinat J, Lambert M, Karow A, Peth J, et al. Excess costs of mental disorders by level of severity. Soc Psychiatry Psychiatr Epidemiol. 2023; 58:973–985.
Article3. The National Mental Health and Welfare Commission. The socioeconomic costs of the mental illness. National Mental Health Trends. 2019; 14:1–3.4. O’Donoghue B, O’Connor K, Thompson A, McGorry P. The need for early intervention for psychosis to persist throughout the COVID-19 pandemic and beyond. Ir J Psychol Med. 2021; 38:214–219.
Article5. Morgan VA, McGrath JJ, Jablensky A, Badcock JC, Waterreus A, Bush R, et al. Psychosis prevalence and physical, metabolic and cognitive co-morbidity: data from the second Australian national survey of psychosis. Psychol Med. 2014; 44:2163–2176.
Article6. Furukawa TA, Levine SZ, Tanaka S, Goldberg Y, Samara M, Davis JM, et al. Initial severity of schizophrenia and efficacy of antipsychotics: Participant-level meta-analysis of 6 placebo-controlled studies. JAMA Psychiatry. 2015; 72:14–21. https://doi.org/10.1001/jamapsychiatry.2014.2127.
Article7. Gaebel W, Riesbeck M, Wobrock T. Schizophrenia guidelines across the world: A selective review and comparison. Intl Rev Psychiatry. 2011; 4:379–387.
Article8. Bach P. ACT with the Seriously Mentally Ill. In A Practical Guide to Acceptance and Commitment Therapy. NY: Springer;2004. p. 185–208.9. Miner CR, Rosenthal RN, Hellerstein DJ. Prediction of Compliance with Outpatient Referral in Patients With Schizophrenia and Psychoactive Substance Use Disorders. Arch Gen Psychiatry. 1997; 8:706–712.
Article10. Anthony WA. Recovery From Mental Illness: The Guiding Vision of the Mental Health Service System in the 1990s. Psychosoc Rehab J. 1993; 4:11–23.
Article11. WHO Mental Health and Substance Use Team. Recovery and the right to health. WHO QualityRights Core training: mental health and social services. World Health Organization;2019.12. Slade M, Williams J, Bird V, Leamy M, Le Boutillier C. Recovery grows up. J Ment Health. Informa Healthcare. 2012; 2:99–103.13. Conradi HJ, Ormel J, De Jonge P. Symptom profiles of DSM-IVdefined remission, recovery, relapse, and recurrence of depression: the role of the core symptoms. Depress Anxiety. 2012; 29:638–645.
Article14. Wunderink L, Sytema S, Nienhuis FJ, Wiersma D. Clinical recovery in first-episode psychosis. Schizophr Bull. 2009; 35:362–369.
Article15. Bäckström M, Lund K, Eklund M. Exploring mediators of the recovery process over time among mental health service users, using a mixed model regression analysis based on cluster RCT data. BMC Psychiatry. 2020; 520:1–12.
Article16. Jeong NR and Woo JH. Systematic Literature Review and Meta-analysis on Acceptance-Commitment Therapy for Psychotic Disorder Based on the Perspective of Recovery. J Rehab Psychol. 2021; 28:41–62.17. Jagtap S, Romanowska S, Leibovitz T, Onno KA, Burhan AM, Best MW. Can cognitive remediation therapy be delivered remotely? A review examining feasibility and acceptability of remote interventions. Schizophr Res Cogn. 2022; 102238:1–7.
Article18. Davies A, Mueller J. mHealth, eHealth and Related Term. In Developing medical apps and mHealth interventions: a guide for researchers, physicians and informaticians. NY: Springer;2020.19. Lee SE, Shin H, Hur JW. mHealth for Mental Health in the COVID-19 Era. Kor J Clin Psychol. 2020; 39:325–354.
Article20. Jeong NR, Kim EJ. Development and effects of mobile app-based Acceptance-Commitment Therapy for clinical outpatients with depressive symptoms. CBT in Kor. 2023; 23:177–200.
Article21. Miralles I, Granell C, Díaz-Sanahuja L, van Woensel W, BretónLópez J, Mira A, et al. Smartphone apps for the treatment of mental disorders: Systematic review. JMIR mHealth and uHealth. 2020; 4:1–28.
Article22. Kim H, Choi H, Han SM. The Internet-based CBT. Seoul: Hakjisa;2020.23. Kuhn E, McGee-Vincent P. Using mobile Apps in mental health practice. In : Reger GM, editor. Technology and mental health: a clinician’s guide to improving outcomes. UK: Routledge/Taylor & Francis Group;2021. p. 56–74.24. Wrzus C, Neubauer AB. Ecological Momentary Assessment: a Meta-Analysis on Designs, Samples, and Compliance Across Research Fields. Assessment. 2023; 30:825–846.
Article25. Kwon S, Firth J, Joshi D, Torous J. Accessibility and availability of smartphone apps for schizophrenia. Schizophrenia. 2022; 1:1–15.
Article26. Oh E, Gang M. Effect of Digital Health Interventions on Psychotic Symptoms among Persons with Severe Mental Illness in Community: A Systematic Review and Meta-Analysis. J Kor Acad Nurs. 2023; 53:69–86.
Article27. Fulford D, Schupbach E, Gard DE, Mueser KT, Mow J. Do cognitive impairments limit treatment gains in a standalone digital intervention for psychosis? A test of the digital divide. Schizophr Res Cogn. 2022; 100244:1–6.
Article28. Nassir Ghaemi S, Sverdlov O, Van Dam J, Campellone T, Gerwien R. A Smartphone-Based Intervention as an Adjunct to Standardof-Care Treatment for Schizophrenia: Randomized Controlled Trial. JMIR Form Res. 2022; 3:1–16.
Article29. Gumley AI, Bradstreet S, Ainsworth J, Allan S, Alvarez-Jimenez M, Birchwood M, et al. Digital smartphone intervention to recognise and manage early warning signs in schizophrenia to prevent relapse: the EMPOWER feasibility cluster RCT. Health Technol Assess (Rockv). 2022; 27:1–173.
Article30. Weintraub MJ, Ichinose MC, Zinberg J, Done M, Morgan-Fleming GM, Wilkerson CA, et al. App-enhanced transdiagnostic CBT for adolescents with mood or psychotic spectrum disorders. J Affect Disord. 2022; 311:319–326.
Article31. Ben-Zeev D, Chander A, Tauscher J, Buck B, Nepal S, Campbell A, et al. A smartphone intervention for people with serious mental illness: Fully remote randomized controlled trial of CORE. J Med Internet Res. 2021; 11:1–16.
Article32. Dabit S, Quraishi S, Jordan J, Biagianti B. Improving social functioning in people with schizophrenia-spectrum disorders via mobile experimental interventions: Results from the CLIMB pilot trial. Schizophr Res Cogn. 2021; 100211:1–10.
Article33. Garety P, Ward T, Emsley R, Greenwood K, Freeman D, Fowler D, et al. Effects of SlowMo, a Blended Digital Therapy Targeting Reasoning, on Paranoia among People with Psychosis: A Randomized Clinical Trial. JAMA Psychiatry. 2021; 78:714–725.
Article34. Haesebaert F, El Oussoul S, Pavard A, Fabre D, Cellard C, Magaud L, et al. PLAN-e-PSY, a mobile application to improve case management and patient’s functioning in first episode psychosis: Protocol for an open-label, multicentre, superiority, randomised controlled trial. BMJ Open. 2021; 9:1–11.
Article35. Kidd SA, Feldcamp L, Adler A, Kaleis L, Wang W, Vichnevetski K, et al. Feasibility and outcomes of a multi-function mobile health approach for the schizophrenia spectrum: APP4Independence (A4I). PLoS One. 2019; 7:1–17.
Article36. Steare T, Giorgalli M, Free K, Harju-Seppänen J, Akther S, Eskinazi M, et al. A qualitative study of stakeholder views on the use of a digital app for supported self-management in early intervention services for psychosis. BMC Psychiatry. 2021; 311:1–12.
Article37. Krzystanek M, Krysta K, Borkowski M, Przybyło J, Pałasz A, et al. The effect of smartphone-based cognitive training on the functional/cognitive markers of schizophrenia: a one-year randomized study. J Clin Med. 2020; 9:1–12.
Article38. Cullen BA, Rodriguez K, Eaton WW, Mojtabai R, Von Mach T, Ybarra ML. Clinical outcomes from the texting for relapse prevention (T4RP) in schizophrenia and schizoaffective disorder study. Psychiatry Res. 2020; 113346:1–13.
Article39. Hanssen E, Balvert S, Borkelmans K, van Os J, Delespaul P, et al. An ecological momentary intervention incorporating personalised feedback to improve symptoms and social functioning in schizophrenia spectrum disorders. Psychiatry Res. 2020; 112695:1–8.
Article40. Hui CLM, Lam BST, Wong AKH, Tao TJ, Ho ECN, Suen YN, et al. ReMind, a smartphone application for psychotic relapse prediction: a longitudinal study protocol. Early Interv Psychiatry. 2021; 15:1659–1666.
Article41. Lewis S, Ainsworth J, Sanders C, Stockton-Powdrell C, Machin M, Whelan P, et al. Smartphone-enhanced symptom management in psychosis: Open, randomized controlled trial. J Med Internet Res. 2020; 8:1–11.
Article42. Traber-Walker N, Gerstenberg M, Metzler S, Joris MR, Karr M, Studer N, et al. Evaluation of the combined treatment approach “robin”(Standardized Manual and Smartphone App) for adolescents at clinical high risk for psychosis. Front Psychiatry. 2019; 384:1–11.43. Bell IH, Rossell SL, Farhall J, Hayward M, Lim MH, FieldingSmith SF, et al. Pilot randomised controlled trial of a brief copingfocused intervention for hearing voices blended with smartphonebased ecological momentary assessment and intervention (SAVVy): Feasibility, acceptability and preliminary clinical outcomes. Schizophr Res. 2020; 216:479–487.
Article44. Vaessen T, Steinhart H, Batink T, Klippel A, Van Nierop M, Reininghaus U, et al. ACT in daily life in early psychosis: an ecological momentary intervention approach. Psychosis. 2019; 11:93–104.
Article45. Nicholson J, Wright SM, Carlisle AM. Pre-post, mixed-methods feasibility study of the WorkingWell mobile support tool for individuals with serious mental illness in the USA: a pilot study protocol. BMJ Open. 2018; 2:1–9.
Article46. Terp M, Jørgensen R, Laursen BS, Mainz J, Bjørnes CD. A smartphone app to foster power in the everyday management of living with schizophrenia: Qualitative analysis of young adults’ perspectives. JMIR Ment Health;2018.47. Biagianti B, Hidalgo-Mazzei D, Meyer N. Developing digital interventions for people living with serious mental illness: Perspectives from three mHealth studies. Evid Based Ment Health. 2017; 20:98–101.
Article48. Garety P, Ward T, Emsley R, Greenwood K, Freeman D, Fowler D, et al. Digitally supported CBT to reduce paranoia and improve reasoning for people with schizophrenia-spectrum psychosis: the SlowMo RCT. Efficacy and Mech Eval. 2021; 8:1–90.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Development and Evaluation of a Self-management Mobile App for Adults with Osteoarthritis
- Effects of Structured Group Acceptance and Commitment Therapy for Psychological Acceptance and Recovery Among Inpatients With Psychotic Disorder: A Pilot Study
- Acceptance and Commitment Therapy for Psychosis
- Importance of Early Detection in Early Psychosis
- Effectiveness of a mobile app-based individualized non-pharmacological intervention on behavioral and psychological symptoms of dementia in community-dwelling older adults: Study protocol for a randomized control trial