J Korean Med Sci.
2024 Apr;39(14):e132. 10.3346/jkms.2024.39.e132.
Antimicrobial Use and CarbapenemResistant Enterobacterales in Korea: A Nationwide Case-Control Study With Propensity Score Matching
- Affiliations
-
- 1Division of Infectious Diseases, Department of Internal Medicine, Kyungpook National University Hospital, Kyungpook National University School of Medicine, Daegu, Korea
- KMID: 2554585
- DOI: http://doi.org/10.3346/jkms.2024.39.e132
Abstract
- Background
Nationwide research on the association between carbapenem-resistant Enterobacterales (CREs) and antibiotic use is limited.
Methods
This nested case-control study analyzed Korean National Health Insurance claims data from April 2017 to April 2019. Based on the occurrence of CRE, hospitalized patients aged ≥ 18 years were classified into CRE (cases) and control groups. Propensity scores based on age, sex, modified Charlson comorbidity score, insurance type, long-term care facility, intensive care unit stay, and acquisition of vancomycin-resistant Enterococci were used to match the case and control groups (1:3).
Results
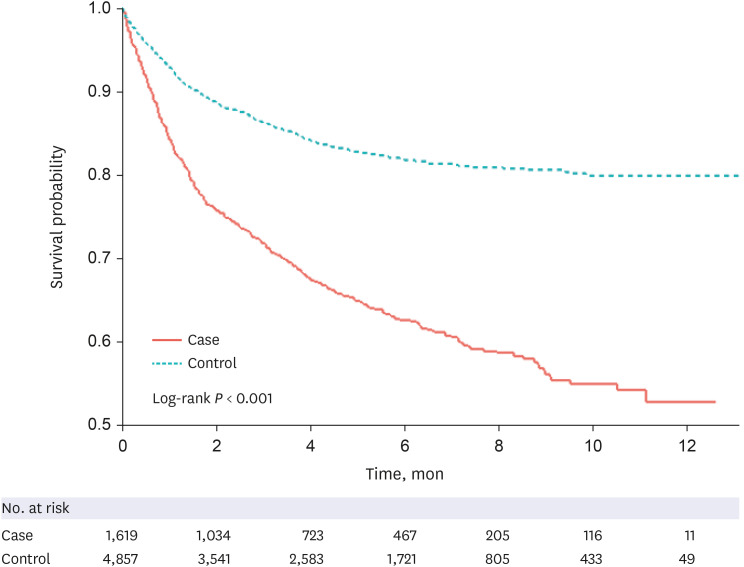
After matching, the study included 6,476 participants (1,619 cases and 4,857 controls). Multivariable logistic regression analysis revealed that the utilization of broad-spectrum antibiotics, such as piperacillin/tazobactam (adjusted odds ratio [aOR], 2.178; 95% confidence interval [CI], 1.829–2.594), third/fourth generation cephalosporins (aOR, 1.764; 95% CI, 1.514–2.056), and carbapenems (aOR, 1.775; 95% CI, 1.454–2.165), as well as the presence of comorbidities (diabetes [aOR, 1.237; 95% CI, 1.061–1.443], hemiplegia or paraplegia [aOR, 1.370; 95% CI, 1.119–1.679], kidney disease [aOR, 1.312; 95% CI, 1.105–1.559], and liver disease [aOR, 1.431; 95% CI, 1.073–1.908]), were significantly associated with the development of CRE. Additionally, the CRE group had higher mortality (8.33 vs. 3.32 incidence rate per 100 personmonths, P < 0.001) and a total cost of healthcare utilization per person-month (15,325,491 ± 23,587,378 vs. 5,263,373 ± 14,070,118 KRW, P < 0.001) than the control group.
Conclusion
The utilization of broad-spectrum antibiotics and the presence of comorbidities are associated with increasing development of CRE. This study emphasizes the importance of antimicrobial stewardship in reducing broad-spectrum antibiotic use and CRE disease burden in Korea.
Figure
Reference
-
1. Logan LK, Weinstein RA. The epidemiology of carbapenem-resistant Enterobacteriaceae: the impact and evolution of a global menace. J Infect Dis. 2017; 215(suppl_1):S28–S36. PMID: 28375512.2. Kang JS, Yi J, Ko MK, Lee SO, Lee JE, Kim KH. Prevalence and risk factors of carbapenem-resistant Enterobacteriaceae acquisition in an emergency intensive care unit in a tertiary hospital in Korea: a case-control study. J Korean Med Sci. 2019; 34(18):e140. PMID: 31074254.3. Korea Disease Control and Prevention Agency. Infectious Disease Portal. Updated 2021. Accessed February 20, 2023. https://www.kdca.go.kr/npt/biz/npp/ist/bass/bassDissStatsMain.do .4. Korea Center for Disease Control and Prevention. Guidelines for control of patients with carbapenemase producing carbapenem-resistant Enterobacteriaceae. Updated 2012. Accessed January 25, 2024. https://www.kdca.go.kr/board/board.es?mid=a20507020000&bid=0019 .5. Lim J, Sim J, Lee H, Hyun J, Lee S, Park S. Characteristics of carbapenem-resistant Enterobacteriaceae (CRE) in Korea, 2022. Public Health Wkly Rep. 2024; 17(4):115–127.6. Potter RF, D’Souza AW, Dantas G. The rapid spread of carbapenem-resistant Enterobacteriaceae. Drug Resist Updat. 2016; 29:30–46. PMID: 27912842.7. Lee HJ, Choi JK, Cho SY, Kim SH, Park SH, Choi SM, et al. Carbapenem-resistant Enterobacteriaceae: prevalence and risk factors in a single community-based hospital in Korea. Infect Chemother. 2016; 48(3):166–173. PMID: 27659436.8. Kim YA, Park YS. Epidemiology and treatment of antimicrobial resistant gram-negative bacteria in Korea. Korean J Intern Med. 2018; 33(2):247–255. PMID: 29506343.9. Park DA, Lee NR, Park JJ, Son SK, Paek KR, Moon SY. A comparative clinical study on the efficacy of carbapenem and alternative antibiotics in the treatment of bacteremia and urinary tract infections caused by ESBL-producing Enterobacteriaceae. Res Reprod. 2016; 1(2):1–210.10. Office of Prime Minister in South Korea. National action plan on antimicrobial resistance (2016-2020). Updated 2016. Accessed February 20, 2023. https://www.who.int/publications/m/item/republic-of-korea-national-action-plan-on-antimicrobial-resistance-(2016-2020) .11. Tamma PD, Goodman KE, Harris AD, Tekle T, Roberts A, Taiwo A, et al. Comparing the outcomes of patients with carbapenemase-producing and non-carbapenemase-producing carbapenem-resistant Enterobacteriaceae bacteremia. Clin Infect Dis. 2017; 64(3):257–264. PMID: 28013264.12. Lee CS, Doi Y. Therapy of infections due to carbapenem-resistant gram-negative pathogens. Infect Chemother. 2014; 46(3):149–164. PMID: 25298904.13. Rubin DB. Using propensity scores to help design observational studies: application to the tobacco litigation. Health Serv Outcomes Res Methodol. 2001; 2(3):169–188.14. World Health Organization. Definition and general considerations of defined daily dose (DDD). Updated 2018. Accessed October 3, 2021. https://www.whocc.no/ddd/definition_and_general_considera/ .15. Sharland M, Gandra S, Huttner B, Moja L, Pulcini C, Zeng M, et al. Encouraging AWaRe-ness and discouraging inappropriate antibiotic use-the new 2019 Essential Medicines List becomes a global antibiotic stewardship tool. Lancet Infect Dis. 2019; 19(12):1278–1280. PMID: 31782385.16. Sundararajan V, Henderson T, Perry C, Muggivan A, Quan H, Ghali WA. New ICD-10 version of the Charlson comorbidity index predicted in-hospital mortality. J Clin Epidemiol. 2004; 57(12):1288–1294. PMID: 15617955.17. Han YH, Bae MJ, Hur YR, Hwang K. Prevalence and risk factors for carbapenem-resistant Enterobacteriaceae colonization in patients with stroke. Brain Neurorehabil. 2019; 12(2):e16.18. Torres-Gonzalez P, Cervera-Hernandez ME, Niembro-Ortega MD, Leal-Vega F, Cruz-Hervert LP, García-García L, et al. Factors associated to prevalence and incidence of carbapenem-resistant Enterobacteriaceae fecal carriage: a cohort study in a Mexican tertiary care hospital. PLoS One. 2015; 10(10):e0139883. PMID: 26431402.19. Swaminathan M, Sharma S, Poliansky Blash S, Patel G, Banach DB, Phillips M, et al. Prevalence and risk factors for acquisition of carbapenem-resistant Enterobacteriaceae in the setting of endemicity. Infect Control Hosp Epidemiol. 2013; 34(8):809–817. PMID: 23838221.20. Yang P, Chen Y, Jiang S, Shen P, Lu X, Xiao Y. Association between antibiotic consumption and the rate of carbapenem-resistant Gram-negative bacteria from China based on 153 tertiary hospitals data in 2014. Antimicrob Resist Infect Control. 2018; 7(1):137. PMID: 30479750.21. Chotiprasitsakul D, Srichatrapimuk S, Kirdlarp S, Pyden AD, Santanirand P. Epidemiology of carbapenem-resistant Enterobacteriaceae: a 5-year experience at a tertiary care hospital. Infect Drug Resist. 2019; 12:461–468. PMID: 30863128.22. Moghnieh R, Abdallah D, Jadayel M, Zorkot W, El Masri H, Dib MJ, et al. Epidemiology, risk factors, and prediction score of carbapenem resistance among inpatients colonized or infected with 3rd generation cephalosporin resistant Enterobacterales . Sci Rep. 2021; 11(1):14757. PMID: 34285312.23. Ling ML, Tee YM, Tan SG, Amin IM, How KB, Tan KY, et al. Risk factors for acquisition of carbapenem resistant Enterobacteriaceae in an acute tertiary care hospital in Singapore. Antimicrob Resist Infect Control. 2015; 4(1):26. PMID: 26106476.24. Song JY, Jeong IS. Development of a risk prediction model of carbapenem-resistant Enterobacteriaceae colonization among patients in intensive care units. Am J Infect Control. 2018; 46(11):1240–1244. PMID: 29884578.25. Jeon MH, Choi SH, Kwak YG, Chung JW, Lee SO, Jeong JY, et al. Risk factors for the acquisition of carbapenem-resistant Escherichia coli among hospitalized patients. Diagn Microbiol Infect Dis. 2008; 62(4):402–406. PMID: 18993012.26. Jiao Y, Qin Y, Liu J, Li Q, Dong Y, Shang Y, et al. Risk factors for carbapenem-resistant Klebsiella pneumoniae infection/colonization and predictors of mortality: a retrospective study. Pathog Glob Health. 2015; 109(2):68–74. PMID: 25707874.27. Ahn JY, Song JE, Kim MH, Choi H, Kim JK, Ann HW, et al. Risk factors for the acquisition of carbapenem-resistant Escherichia coli at a tertiary care center in South Korea: a matched case-control study. Am J Infect Control. 2014; 42(6):621–625. PMID: 24837112.28. Teo J, Cai Y, Tang S, Lee W, Tan TY, Tan TT, et al. Risk factors, molecular epidemiology and outcomes of ertapenem-resistant, carbapenem-susceptible Enterobacteriaceae: a case-case-control study. PLoS One. 2012; 7(3):e34254. PMID: 22461908.29. Pérez-Galera S, Bravo-Ferrer JM, Paniagua M, Kostyanev T, de Kraker ME, Feifel J, et al. Risk factors for infections caused by carbapenem-resistant Enterobacterales: an international matched case-control-control study (EURECA). EClinicalMedicine. 2023; 57:101871. PMID: 36895801.30. Gao Y, Chen M, Cai M, Liu K, Wang Y, Zhou C, et al. An analysis of risk factors for carbapenem-resistant Enterobacteriaceae infection. J Glob Antimicrob Resist. 2022; 30:191–198. PMID: 35429666.31. Asai N, Sakanashi D, Suematsu H, Kato H, Hagihara M, Nishiyama N, et al. The epidemiology and risk factor of carbapenem-resistant Enterobacteriaceae colonization and infections: case control study in a single institute in Japan. J Infect Chemother. 2018; 24(7):505–509. PMID: 29548627.32. Salomão MC, Guimarães T, Duailibi DF, Perondi MB, Letaif LS, Montal AC, et al. Carbapenem-resistant Enterobacteriaceae in patients admitted to the emergency department: prevalence, risk factors, and acquisition rate. J Hosp Infect. 2017; 97(3):241–246. PMID: 28826688.33. Bhargava A, Hayakawa K, Silverman E, Haider S, Alluri KC, Datla S, et al. Risk factors for colonization due to carbapenem-resistant Enterobacteriaceae among patients exposed to long-term acute care and acute care facilities. Infect Control Hosp Epidemiol. 2014; 35(4):398–405. PMID: 24602945.34. Bar-Yoseph H, Cohen N, Korytny A, Andrawus ER, Even Dar R, Geffen Y, et al. Risk factors for mortality among carbapenem-resistant Enterobacteriaceae carriers with focus on immunosuppression. J Infect. 2019; 78(2):101–105. PMID: 30312647.35. Brown AL, van Kamp I. WHO environmental noise guidelines for the European region: a systematic review of transport noise interventions and their impacts on health. Int J Environ Res Public Health. 2017; 14(8):873. PMID: 28771220.36. Sheu CC, Chang YT, Lin SY, Chen YH, Hsueh PR. Infections caused by carbapenem-resistant Enterobacteriaceae: an update on therapeutic options. Front Microbiol. 2019; 10:80. PMID: 30761114.37. Zhou R, Fang X, Zhang J, Zheng X, Shangguan S, Chen S, et al. Impact of carbapenem resistance on mortality in patients infected with Enterobacteriaceae: a systematic review and meta-analysis. BMJ Open. 2021; 11(12):e054971.38. Tangsawad W, Kositamongkol C, Chongtrakool P, Phisalprapa P, Jitmuang A. The burden of carbapenem-resistant Enterobacterales infection in a large Thai tertiary care hospital. Front Pharmacol. 2022; 13:972900. PMID: 36120317.39. Chen HY, Jean SS, Lee YL, Lu MC, Ko WC, Liu PY, et al. Carbapenem-resistant Enterobacterales in long-term care facilities: a global and narrative review. Front Cell Infect Microbiol. 2021; 11:601968. PMID: 33968793.40. Kim J. Strategies to Enhance the Use of National Health Insurance Claims Database in Generating Health Statistics. Seoul, Korea: Health Insurance Review and Assessment Services;2005.41. Park B, Sung J, Park K, Seo S, Kim S. Strategies to Improve the Validity of Diagnostic Codes of National Health Insurance Claims Data. Seoul, Korea: Health Insurance Review and Assessment Services;2002.42. Carrara E, Conti M, Meschiari M, Mussini C. The role of antimicrobial stewardship in preventing KPC-producing Klebsiella pneumoniae . J Antimicrob Chemother. 2021; 76(Suppl 1):i12–i18. PMID: 33534879.43. Cipko K, Cuenca J, Wales E, Harris J, Bond S, Newton P, et al. Implementation of an antimicrobial stewardship programme and reduction in carbapenemase-producing Enterobacterales in an Australian local health district. JAC Antimicrob Resist. 2020; 2(3):dlaa041. PMID: 34223004.44. Barros A, Monroy H, Bergo P, Beck E, David L, Rigatto MH. Antimicrobial stewardship programme associated with earlier prescription of in vitro susceptible therapy and lower 14-day mortality in patients with carbapenem-resistant Enterobacterales bacteraemia: a cohort study. J Glob Antimicrob Resist. 2022; 28:130–135. PMID: 34933141.45. Aiesh BM, Nazzal MA, Abdelhaq AI, Abutaha SA, Zyoud SH, Sabateen A. Impact of an antibiotic stewardship program on antibiotic utilization, bacterial susceptibilities, and cost of antibiotics. Sci Rep. 2023; 13(1):5040. PMID: 36977796.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Applications of propensity score matching: a case series of articles published in Annals of Coloproctology
- Propensity Score Matching: A Conceptual Review for Radiology Researchers
- An introduction to propensity score matching methods
- The impact of patient sex on survival after unintentional trauma in Korea: a retrospective, observational, case-control study
- Improving Causal Inference in Observational Studies: Propensity Score Matching