J Rheum Dis.
2024 Apr;31(2):125-129. 10.4078/jrd.2023.0027.
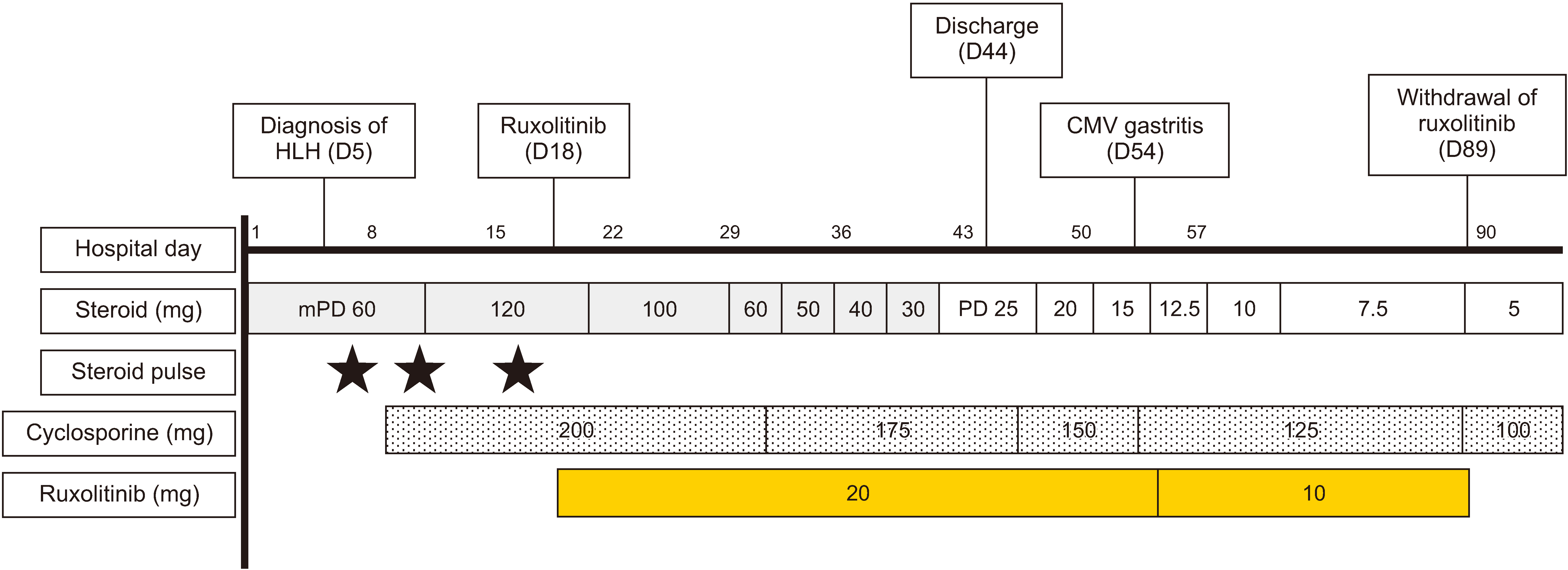
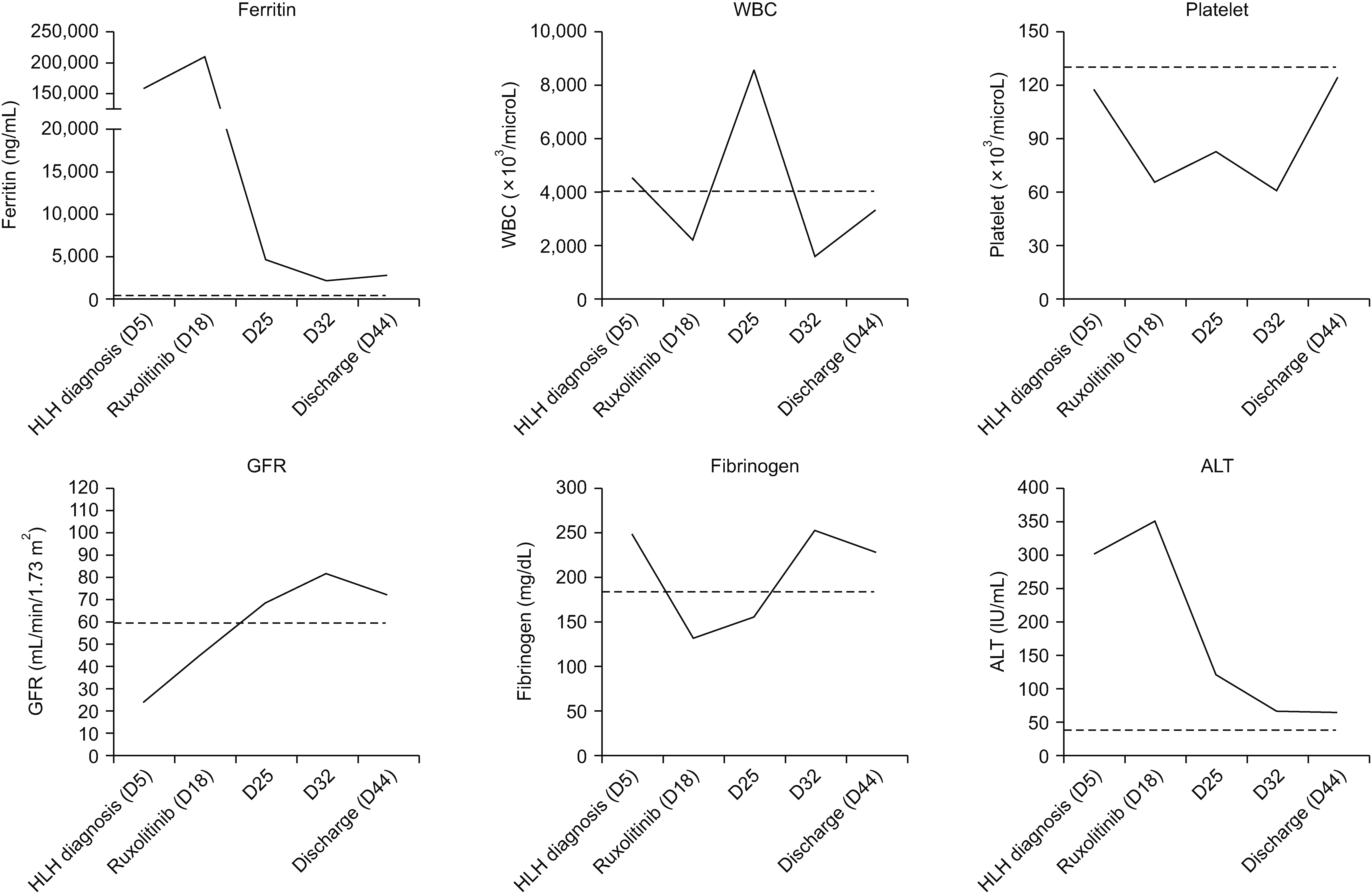
Successful treatment of hemophagocytic lymphohistiocytosis in a patient with systemic lupus erythematosus with ruxolitinib: a case report
- Affiliations
-
- 1Division of Rheumatology, Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea
- 2Division of Rheumatology, Department of Internal Medicine, Hallym University Dongtan Sacred Heart Hospital, Hwaseong, Korea
- KMID: 2554362
- DOI: http://doi.org/10.4078/jrd.2023.0027
Abstract
- Hemophagocytic lymphohistiocytosis (HLH) is a rare, life-threatening hematological disorder characterized by uncontrolled activation of CD8+ T and natural killer cells, leading to a cytokine storm and severe organ dysfunction. Although secondary HLH related to autoimmune diseases usually demonstrates a good treatment response to immunosuppressive therapy for underlying conditions, there is no consensus regarding the treatment in case of unresponsiveness to the treatment. Herein, we present a case of HLH that was unresponsive to high-dose glucocorticoid and cyclosporine treatment in a patient with newly diagnosed systemic lupus erythematosus. The patient’s clinical features and laboratory abnormalities rapidly improved with ruxolitinib, an oral Janus kinase 1 and 2 (JAK1/2) inhibitor. This result suggests that blocking JAK-STAT pathway may be a potential treatment option in patients with refractory HLH secondary to autoimmune diseases.
Figure
Reference
-
1. Morimoto A, Nakazawa Y, Ishii E. 2016; Hemophagocytic lymphohistiocytosis: pathogenesis, diagnosis, and management. Pediatr Int. 58:817–25. DOI: 10.1111/ped.13064. PMID: 27289085.
Article2. Carter SJ, Tattersall RS, Ramanan AV. 2019; Macrophage activation syndrome in adults: recent advances in pathophysiology, diagnosis and treatment. Rheumatology (Oxford). 58:5–17. DOI: 10.1093/rheumatology/key006. PMID: 29481673.
Article3. Henter JI, Horne A, Aricó M, Egeler RM, Filipovich AH, Imashuku S, et al. 2007; HLH-2004: diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer. 48:124–31. DOI: 10.1002/pbc.21039. PMID: 16937360.
Article4. Grom AA, Horne A, De Benedetti F. 2016; Macrophage activation syndrome in the era of biologic therapy. Nat Rev Rheumatol. 12:259–68. DOI: 10.1038/nrrheum.2015.179. PMID: 27009539. PMCID: PMC5851441.
Article5. Ahmed A, Merrill SA, Alsawah F, Bockenstedt P, Campagnaro E, Devata S, et al. 2019; Ruxolitinib in adult patients with secondary haemophagocytic lymphohistiocytosis: an open-label, single-centre, pilot trial. Lancet Haematol. 6:e630–7. DOI: 10.1016/S2352-3026(19)30156-5. PMID: 31537486.
Article6. Das R, Guan P, Sprague L, Verbist K, Tedrick P, An QA, et al. 2016; Janus kinase inhibition lessens inflammation and ameliorates disease in murine models of hemophagocytic lymphohistiocytosis. Blood. 127:1666–75. DOI: 10.1182/blood-2015-12-684399. PMID: 26825707. PMCID: PMC4817310.
Article7. Henter JI, Tondini C, Pritchard J. 2004; Histiocyte disorders. Crit Rev Oncol Hematol. 50:157–74. DOI: 10.1016/j.critrevonc.2004.01.002. PMID: 15157664.
Article8. Janka GE, Schneider EM. 2004; Modern management of children with haemophagocytic lymphohistiocytosis. Br J Haematol. 124:4–14. DOI: 10.1046/j.1365-2141.2003.04726.x. PMID: 14675403.
Article9. Fardet L, Galicier L, Lambotte O, Marzac C, Aumont C, Chahwan D, et al. 2014; Development and validation of the HScore, a score for the diagnosis of reactive hemophagocytic syndrome. Arthritis Rheumatol. 66:2613–20. DOI: 10.1002/art.38690. PMID: 24782338.
Article10. Gavand PE, Serio I, Arnaud L, Costedoat-Chalumeau N, Carvelli J, Dossier A, et al. 2017; Clinical spectrum and therapeutic management of systemic lupus erythematosus-associated macrophage activation syndrome: a study of 103 episodes in 89 adult patients. Autoimmun Rev. 16:743–9. DOI: 10.1016/j.autrev.2017.05.010. PMID: 28483541.
Article11. Nam SH, Ahn SM, Oh JS, Hong S, Lee CK, Yoo B, et al. 2022; Macrophage activation syndrome in rheumatic disease: clinical characteristics and prognosis of 20 adult patients. PLoS One. 17:e0267715. DOI: 10.1371/journal.pone.0267715. PMID: 35522672. PMCID: PMC9075640.
Article12. Wafa A, Hicham H, Naoufal R, Hajar K, Rachid R, Souad B, et al. 2022; Clinical spectrum and therapeutic management of systemic lupus erythematosus-associated macrophage activation syndrome: a study of 20 Moroccan adult patients. Clin Rheumatol. 41:2021–33. DOI: 10.1007/s10067-022-06055-9. PMID: 35179662.
Article13. Wang J, Wang Y, Wu L, Wang X, Jin Z, Gao Z, et al. 2020; Ruxolitinib for refractory/relapsed hemophagocytic lymphohistiocytosis. Haematologica. 105:e210–2. DOI: 10.3324/haematol.2019.222471. PMID: 31515353. PMCID: PMC7193462.
Article14. Rumi E, Sant'Antonio E, Cavalloni C, Comolli G, Ferretti VV, Cassaniti I, et al. 2020; Impaired virus-specific T cell responses in patients with myeloproliferative neoplasms treated with ruxolitinib. Hematol Oncol. 38:554–9. DOI: 10.1002/hon.2769. PMID: 32583904.
Article15. Abedin S, McKenna E, Chhabra S, Pasquini M, Shah NN, Jerkins J, et al. 2019; Efficacy, toxicity, and infectious complications in ruxolitinib-treated patients with corticosteroid-refractory graft-versus-host disease after hematopoietic cell transplantation. Biol Blood Marrow Transplant. 25:1689–94. DOI: 10.1016/j.bbmt.2019.04.003. PMID: 30965140.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Hemophagocytic Lymphohistiocytosis in a Child with Systemic Lupus Erythematosus
- A Case of Systemic Lupus Erythematosus-Associated Hemophagocytic Lymphohistiocytosis Treated Successfully with an Etoposide Infusion
- Three Cases of Secondary Hemophagocytic Lymphohistiocytosis Associated with Systemic Erythematosus Lupus
- A Case of Subcutaneous Panniculitic T-cell Lymphoma-like Lesion Occurring in a Patient with Systemic Lupus Erythematosus
- Refractory Macrophage Activation Syndrome in a Patient with Systemic Lupus Erythematosus Treated with Tocilizumab