J Rheum Dis.
2024 Apr;31(2):116-119. 10.4078/jrd.2023.0052.
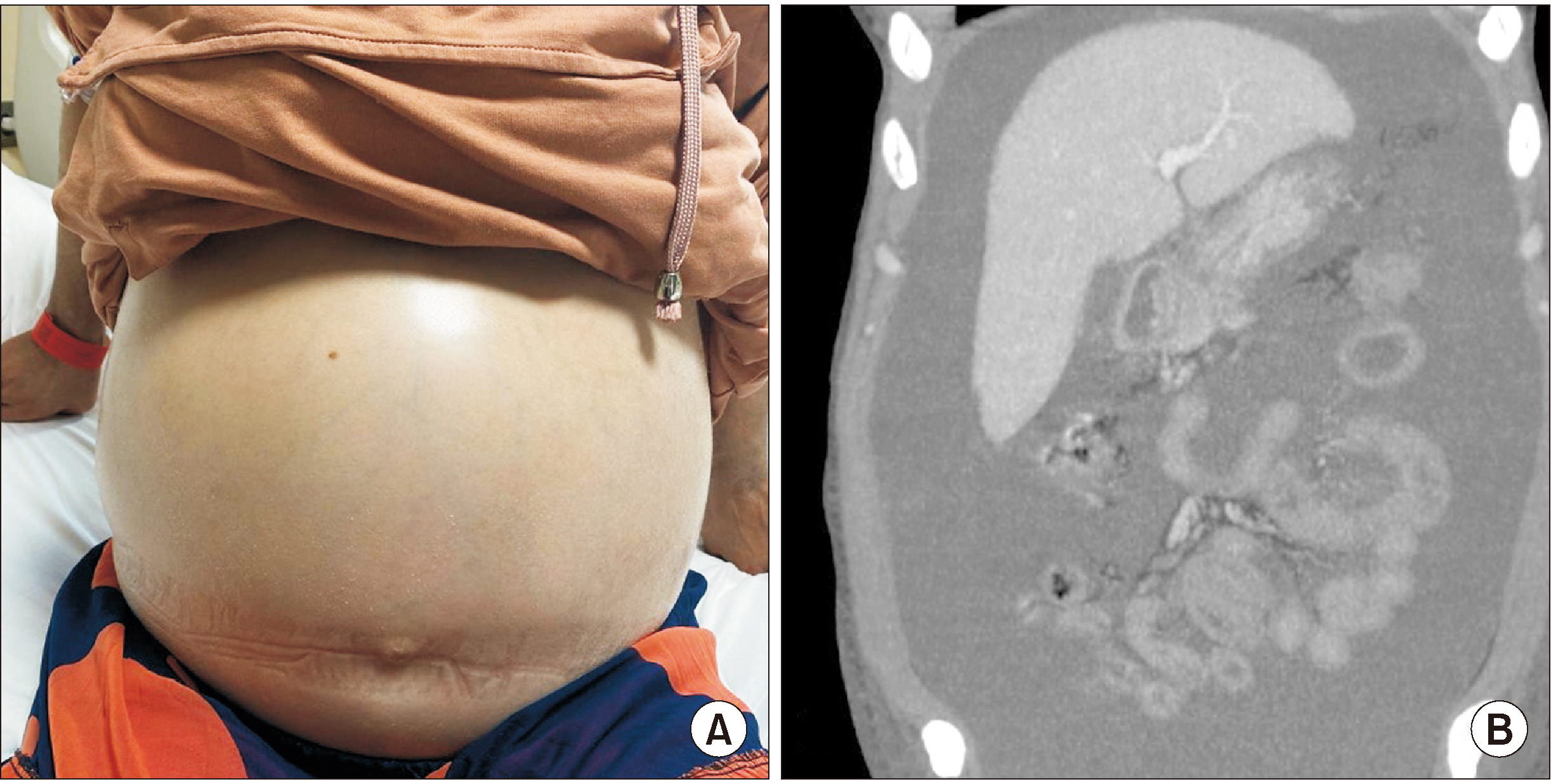
Lupus nephritis presenting with massive ascites and pleural effusion (pseudo-pseudo Meigs’ syndrome)
- Affiliations
-
- 1Department of Rheumatology, Başakşehir Çam and Sakura City Hospital, University of Health Sciences, Istanbul, Turkey
- 2Department of Internal Medicine, University of Health Sciences Bağcılar Education and Research Hospital, Istanbul, Turkey
- KMID: 2554360
- DOI: http://doi.org/10.4078/jrd.2023.0052
Abstract
- The triad of ascites, pleural effusion, and elevated cancer antigen-125 (CA-125) levels in the absence of ovarian malignancy in systemic lupus erythematosus patients is specifically named pseudo-pseudo Meigs’ syndrome (PPMS) or Tjalma syndrome. In this case we reported a 33 years female patient with pleural effusion lasting for 3 years and new onset progressive massive ascites and increased level of CA-125. After she was evaluated for an underlying benign and malign ovarian tumor or any other malignancies, serologic tests were requested with respect to progressive renal dysfunction, proteinuria, lymphopenia, anemia, and effusion. She was diagnosed with systemic lupus erythamatosus (SLE) and renal biopsy showed class-V lupus nephritis. Immunosuppressive treatment led to improvement in both SLE activity and components of PPMS, including massive ascites and pleural effusion and without the need of diuretics. Co-existence of unexplained CA-125 increase, pleural effusion, and ascites might be related to PPMS and detailed examination to exclude malignancy and early and effective treatment of SLE are the mainstay of management.
Figure
Reference
-
1. Tjalma WA. 2005; Ascites, pleural effusion, and CA 125 elevation in an SLE patient, either a Tjalma syndrome or, due to the migrated Filshie clips, a pseudo-Meigs syndrome. Gynecol Oncol. 97:288–91. DOI: 10.1016/j.ygyno.2004.12.022. PMID: 15790480.
Article2. Widra EA, Armstrong J. 1995; Pseudo-Meigs' syndrome and lupus. Int J Gynaecol Obstet. 49:193–4. DOI: 10.1016/0020-7292(95)02355-G. PMID: 7649329.
Article3. Meena DS, Kumar B, Gopalakrishnan M, Kachhwaha A, Kumar S, Sureka B, et al. 2021; Pseudo-pseudo Meigs' syndrome (PPMS) in chronic lupus peritonitis: a case report with review of literature. Mod Rheumatol Case Rep. 5:300–5. DOI: 10.1080/24725625.2021.1916160. PMID: 33970813.
Article4. Quintero-Muñoz E, Gómez Pineda MA, Araque Parra C, Vallejo Castillo CA, Ortega Marrugo V, Bonilla Jassir J, et al. 2021; Is there any relationship between massive ascites and elevated CA-125 in systemic lupus erythematosus? Case report and review of the literature. Mod Rheumatol Case Rep. 5:292–9. DOI: 10.1080/24725625.2021.1909213. PMID: 33783326.
Article5. Thaker DA, Stride PJ, Dettrick A. 2011; A pseudo case of atypical pseudo-Meigs syndrome. Indian J Cancer. 48:364–6. DOI: 10.4103/0019-509X.84914. PMID: 21921340.
Article6. Wiatrowska B, Krajci P, Berner A. 2000; [Pseudo-Meigs' syndrome]. Tidsskr Nor Laegeforen. 120:364–6. Norwegian.7. Bes C, Dağlı Ü, Memedoğlu P, Soy M. 2013; A rare form of SLE: pseudo-pseudo meigs syndrome and hydrocephalus. Rheumatol Int. 33:2175–6. DOI: 10.1007/s00296-012-2420-6. PMID: 22451030.
Article8. Bes C, Soy M. 2011; Pseudo-pseudo Meigs syndrome developed under the leflunomide therapy. Rheumatol Int. 31:521–3. DOI: 10.1007/s00296-009-1190-2. PMID: 19844717.
Article9. Chao YH, Chen HY. 2022; Rare cause of ascites and pleural effusion: the first case report and literature review of pseudo-pseudo Meig's syndrome in Taiwan. J Formos Med Assoc. 121:2633–8. DOI: 10.1016/j.jfma.2022.03.020. PMID: 35459608.
Article10. Torres Jiménez AR, Solís-Vallejo E, Céspedes-Cruz AI, Zeferino Cruz M, Rojas-Curiel EZ, Sánchez-Jara B. 2019; Tjalma syndrome (pseudo-pseudo Meigs') as initial manifestation of juvenile-onset systemic lupus erythematosus. Reumatol Clin (Engl Ed). 15:e41–3. DOI: 10.1016/j.reumae.2018.09.003.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Unilateral massive hydrothorax in a gynecologic patient with pseudo-Meigs' syndrome: A case report
- A Case of Pseudo-Meigs' Syndrome
- Pseudo-Meigs' syndrome associateed with pedunculated subserosal myoma and elevated CA-125 level
- A Case of Pseudo-Meigs' Syndrome
- A case report of Pseudo-Meigs' syndrome associated with ovarian serous cystadenocarcinoma