Anat Cell Biol.
2024 Mar;57(1):31-44. 10.5115/acb.23.148.
Exploring the variations of the pancreatic ductal system: a systematic review and metaanalysis of observational studies
- Affiliations
-
- 1Department of Anatomy, All India Institute of Medical Sciences, Patna, India
- 2Department of Anatomy, ESIC Medical College & Hospital, Patna, India
- 3JSS Medical College, JSS Academy of Higher Education and Research, Mysore, India
- 4All India Institute of Medical Sciences, Bathinda, 5 All India Institute of Medical Sciences, Gorakhpur, India
- 5Tulane University School of Medicine, New Orleans, LA, USA
- KMID: 2554239
- DOI: http://doi.org/10.5115/acb.23.148
Abstract
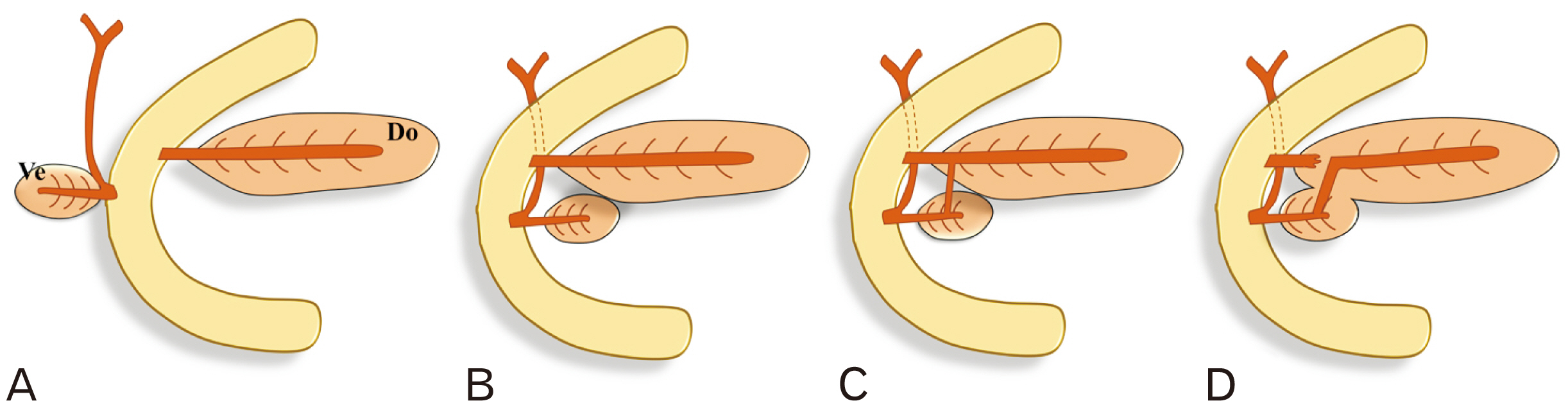
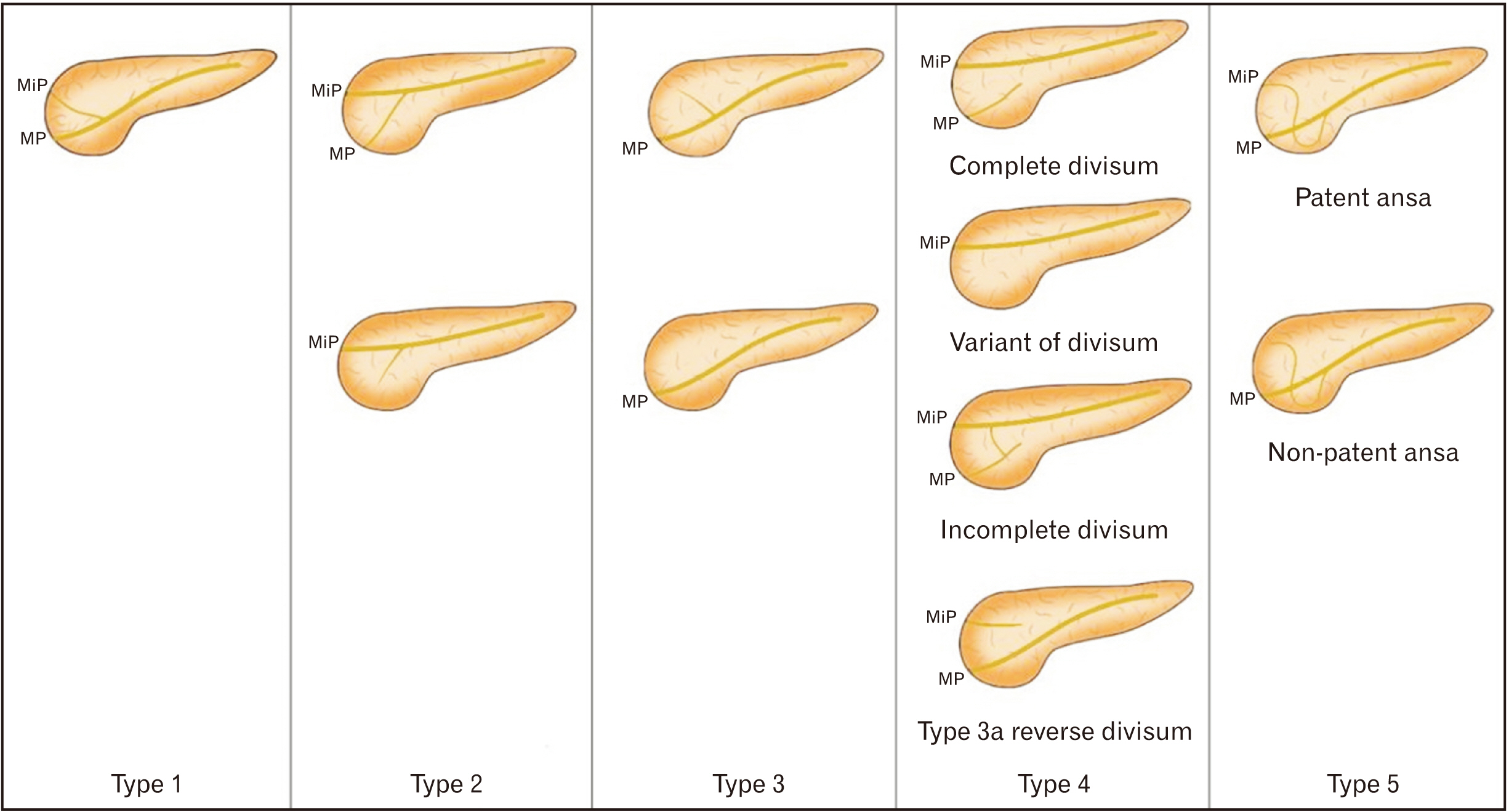
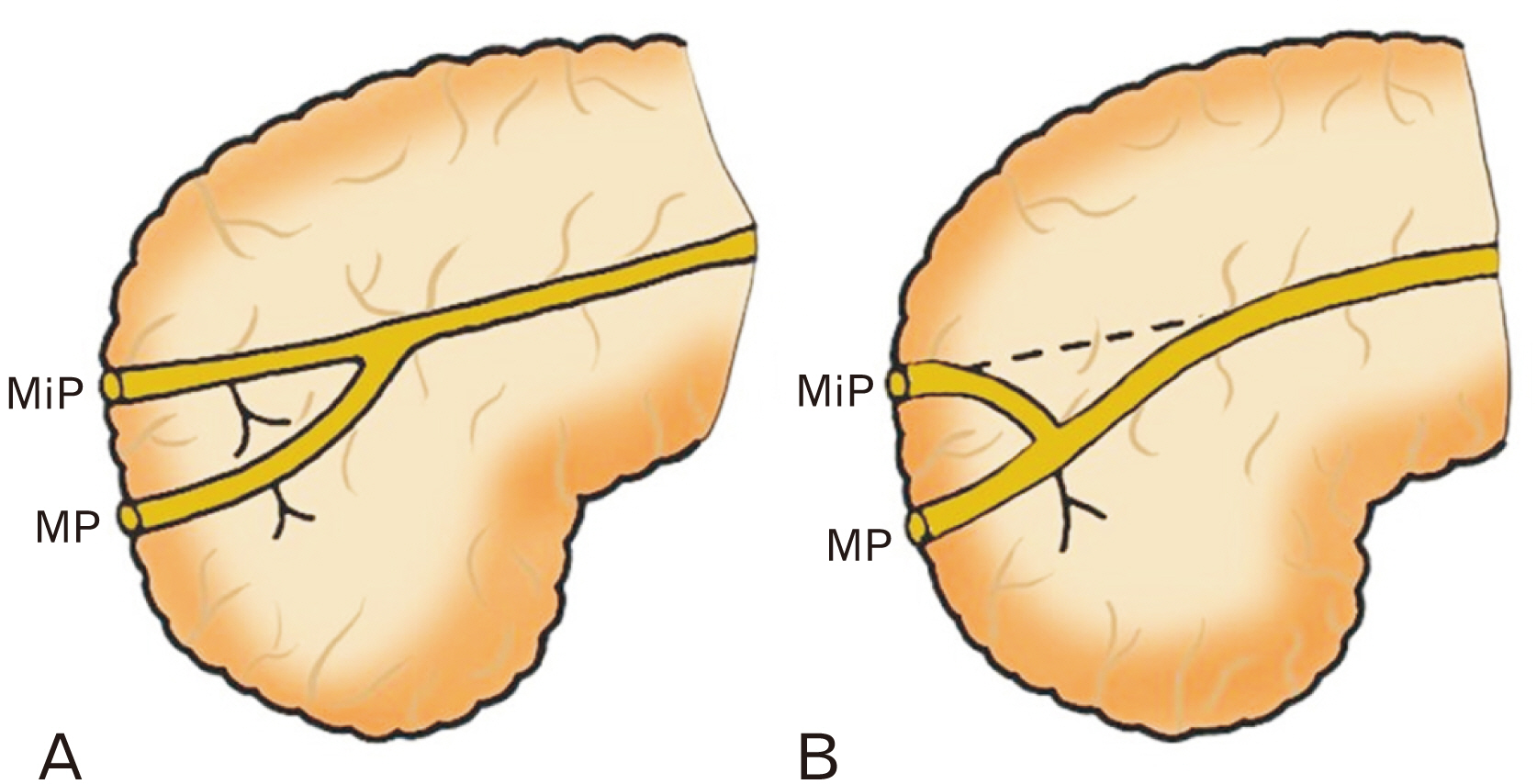
- The exocrine part of the pancreas has a duct system called the pancreatic ductal system (PDS). Its mechanism of development is complex, and any reorganization during early embryogenesis can give rise to anatomical variants. The aim of this study is to collect, classify, and analyze published evidence on the importance of anatomical variants of the PDS, addressing gaps in our understanding of such variations. The MEDLINE, Web of Science, Embase, and Google Scholar databases were searched to identify publications relevant to this review. R studio with meta-package was used for data extraction, risk of bias estimation, and statistical analysis. A total of 64 studies out of 1,778 proved suitable for this review and metanalysis. The meta-analysis computed the prevalence of normal variants of the PDS (92% of 10,514 subjects). Type 3 variants and “descending” subtypes of the main pancreatic duct (MPD) predominated in the pooled samples. The mean lengths of the MPD and accessory pancreatic duct (APD) were 16.53 cm and 3.36 cm, respectively. The mean diameters of the MPD at the head and the APD were 3.43 mm and 1.69 mm, respectively. The APD was present in only 41% of samples, and the long type predominated. The pancreatic ductal anatomy is highly variable, and the incorrect identification of variants may be challenging for surgeons during ductal anastomosis with gut, failure to which may often cause ductal obstruction or pseudocysts formation.
Keyword
Figure
Reference
-
References
1. Anand BS, Vij JC, Mac HS, Chowdhury V, Kumar A. 1989; Effect of aging on the pancreatic ducts: a study based on endoscopic retrograde pancreatography. Gastrointest Endosc. 35:210–3. DOI: 10.1016/S0016-5107(89)72760-7. PMID: 2759399.
Article2. Arora A, Piplani M, Kapoor S, Bhatia B, Singh R, Verma P, Piplani S. 2011; A research study of santorini duct. J Clin Diagn Res. 5:1510–3.3. Abdelkareem H, Ali R, Jibrini M, Nazzal Z, Maree M, Hamaida J, Demyati K. 2019; A study of the anatomic variations of the pancreatico-biliary system in Palestine: a national study. Int Surg J. 6:1020–8. DOI: 10.18203/2349-2902.isj20191066.
Article4. Covantsev S, Chicu C, Mazuruc N, Belic O. 2022; Pancreatic ductal anatomy: more than meets the eye. Surg Radiol Anat. 44:1231–8. DOI: 10.1007/s00276-022-03002-w. PMID: 35986117.
Article5. Renzulli M, Pagano N, Golfieri R. 2020; Pancreas divisum inversus. Clin Anat. 33:646–52. DOI: 10.1002/ca.23475. PMID: 31576611.
Article6. Jagielski M, Smoczyński M, Adrych K. 2018; The anatomical variations of pancreatic duct in the patients with pancreatic diseases. Eur J Transl Clin Med. 1:63–6. DOI: 10.31373/ejtcm/92069.
Article7. Dimitriou I, Katsourakis A, Nikolaidou E, Noussios G. 2018; The main anatomical variations of the pancreatic duct system: review of the literature and its importance in surgical practice. J Clin Med Res. 10:370–5. DOI: 10.14740/jocmr3344w. PMID: 29581798. PMCID: PMC5862083.
Article8. Dugic A, Nikolic S, Mühldorfer S, Bulajic M, Pozzi Mucelli R, Tsolakis AV, Löhr JM, Vujasinovic M. 2020; Clinical importance of main pancreatic duct variants and possible correlation with pancreatic diseases. Scand J Gastroenterol. 55:517–27. DOI: 10.1080/00365521.2020.1760345. PMID: 32393143.
Article9. Adibelli ZH, Adatepe M, Isayeva L, Esen OS, Yildirim M. 2017; Pancreas divisum: a risk factor for pancreaticobiliary tumors - an analysis of 1628 MR cholangiography examinations. Diagn Interv Imaging. 98:141–7. DOI: 10.1016/j.diii.2016.08.004. PMID: 27616039.10. Methley AM, Campbell S, Chew-Graham C, McNally R, Cheraghi-Sohi S. 2014; PICO, PICOS and SPIDER: a comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Serv Res. 14:579. DOI: 10.1186/s12913-014-0579-0. PMID: 25413154. PMCID: PMC4310146.
Article11. Bülow R, Simon P, Thiel R, Thamm P, Messner P, Lerch MM, Mayerle J, Völzke H, Hosten N, Kühn JP. 2014; Anatomic variants of the pancreatic duct and their clinical relevance: an MR-guided study in the general population. Eur Radiol. 24:3142–9. DOI: 10.1007/s00330-014-3359-7. PMID: 25120204.
Article12. Türkvatan A, Erden A, Türkoğlu MA, Yener Ö. 2013; Congenital variants and anomalies of the pancreas and pancreatic duct: imaging by magnetic resonance cholangiopancreaticography and multidetector computed tomography. Korean J Radiol. 14:905–13. DOI: 10.3348/kjr.2013.14.6.905. PMID: 24265565. PMCID: PMC3835637.
Article13. Kamisawa T. 2004; Clinical significance of the minor duodenal papilla and accessory pancreatic duct. J Gastroenterol. 39:605–15. DOI: 10.1007/s00535-004-1390-1. PMID: 15293129.
Article14. Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa Hospital Research Institute;2011.15. De Filippo M, Calabrese M, Quinto S, Rastelli A, Bertellini A, Martora R, Sverzellati N, Corradi D, Vitale M, Crialesi G, Sarli L, Roncoroni L, Garlaschi G, Zompatori M. 2008; Congenital anomalies and variations of the bile and pancreatic ducts: magnetic resonance cholangiopancreatography findings, epidemiology and clinical significance. Radiol Med. 113:841–59. DOI: 10.1007/s11547-008-0298-x. PMID: 18592141.
Article16. Bang S, Suh JH, Park BK, Park SW, Song SY, Chung JB. 2006; The relationship of anatomic variation of pancreatic ductal system and pancreaticobiliary diseases. Yonsei Med J. 47:243–8. DOI: 10.3349/ymj.2006.47.2.243. PMID: 16642555. PMCID: PMC2687635.
Article17. Kamisawa T, Takuma K, Tabata T, Egawa N. 2010; Clinical implications of accessory pancreatic duct. World J Gastroenterol. 16:4499–503. DOI: 10.3748/wjg.v16.i36.4499. PMID: 20857518. PMCID: PMC2945479.
Article18. Shahriah S, Nurunnabi ASM, Johora F, Siddiqua D, Ara S. 2014; Cadaveric study of the anatomical variations of the accessory pancreatic duct. J Bangladesh Soc Physiol. 9:83–8. DOI: 10.3329/jbsp.v9i2.22802.
Article19. Kim HJ, Kim MH, Lee SK, Seo DW, Kim YT, Lee DK, Song SY, Roe IH, Kim JH, Chung JB, Kim CD, Shim CS, Yoon YB, Yang US, Kang JK, Min YI. 2002; Normal structure, variations, and anomalies of the pancreaticobiliary ducts of Koreans: a nationwide cooperative prospective study. Gastrointest Endosc. 55:889–96. DOI: 10.1067/mge.2002.124635. PMID: 12024146.
Article20. Oracz G, Oralewska B, Pertkiewics J, Teisseyre M, Ryzko J, Socha J. 2006; Chronic pancreatitis associated with anatomic anomalies of pancreatic duct in children. J Pediatr Gastroenterol Nutr. 42:E58. DOI: 10.1002/j.1536-4801.2006.tb01738.x.
Article21. Uomo G, Manes G, D'Anna L, Laccetti M, Di Gaeta S, Rabitti PG. 1995; Fusion and duplication variants of pancreatic duct system. Clinical and pancreatographic evaluation. Int J Pancreatol. 17:23–8. DOI: 10.1007/BF02788355. PMID: 8568331.22. Prasanna LC, Rajagopal KV, Thomas HR, Bhat KM. 2015; Accessory pancreatic duct patterns and their clinical implications. J Clin Diagn Res. 9:AC05–7. DOI: 10.7860/JCDR/2015/11539.5660. PMID: 25954609. PMCID: PMC4413057.
Article23. Prasad M, Rout S, Putta T, Kurien RT, Chowdhury SD, Eapen A, Hepsy YS, Rabi S. 2019; Anatomical patterns of the pancreatic ductal system - a cadaveric and magnetic resonance cholangiopancreatography study. J Morphol Sci. 36:279–85. DOI: 10.1055/s-0039-1698371.
Article24. Koshariya M, Behram S, Singour JP, Tiwari S, Khare V. 2019; Anomalous anatomical variation in extrahepatic biliary tree and pancreas and its related vessels: a cadaveric study. Int Surg J. 6:3111–6. DOI: 10.18203/2349-2902.isj20193658.
Article25. Gonoi W, Akai H, Hagiwara K, Akahane M, Hayashi N, Maeda E, Yoshikawa T, Kiryu S, Tada M, Uno K, Okura N, Koike K, Ohtomo K. 2013; Santorinicele without pancreas divisum pathophysiology: initial clinical and radiographic investigations. BMC Gastroenterol. 13:62. DOI: 10.1186/1471-230X-13-62. PMID: 23570616. PMCID: PMC3637151.
Article26. Darnis E, Cronier P, Mercier P, Moreau P, Pillet J, Boyer J. 1984; A radio-anatomical study in vivo on pancreatic ducts. Anat Clin. 6:109–16. DOI: 10.1007/BF01773162. PMID: 6497998.27. Schmitt F, Maignan A, Ploteau S, Hamel A, Lagier S, Blin Y, Rogez JM, Le Borgne J. 2010; New anatomical data on the drainage patterns of the uncinate process of the pancreas. Surg Radiol Anat. 32:777–81. DOI: 10.1007/s00276-010-0680-y. PMID: 20490492.
Article28. Smanio T. 1969; Proposed nomenclature and classification of the human pancreatic ducts and duodenal papillae. Study based on 200 post mortems. Int Surg. 52:125–41. PMID: 5793091.29. Dawson W, Langman J. 1961; An anatomical-radiological study on the pancreatic duct pattern in man. Anat Rec. 139:59–68. DOI: 10.1002/ar.1091390109. PMID: 14025604.
Article30. Berman LG, Prior JT, Abramow SM, Ziegler DD. 1960; A study of the pancreatic duct system in man by the use of vinyl acetate casts of postmortem preparations. Surg Gynecol Obstet. 110:391–403. PMID: 13799593.31. Ishaque I, Ilyas A, Khan O, Kazmi QH, Ladak AH, Rafay A. 2020; Role of magnetic resonance cholangiopancreatography (MRCP) in learning anatomical variations in pancreatic duct. J Pak Med Assoc. 70:472–6. DOI: 10.5455/JPMA.15767. PMID: 32207428.
Article32. Johansson K, Mustonen H, Seppänen H, Lehtimäki TE. 2022; Anatomical pancreatic variants in intraductal papillary mucinous neoplasm patients: a cross-sectional study. BMC Gastroenterol. 22:394. DOI: 10.1186/s12876-022-02465-w. PMID: 35989322. PMCID: PMC9394057.
Article33. Malathi K, Kishan Reddy C. 2019; The study of anatomy of main pancreatic duct and its variations. Perspect Med Res. 7:31–7.34. Shu J, Zhang XM, Zeng N. 2006; Normal pancreatic duct: evaluation with MR cholangiopancreatography. Chin J Med Imaging Technol. 4:2004–6.35. Kasugai T, Kuno N, Kobayashi S, Hattori K. 1972; Endoscopic pancreatocholangiography. I. The normal endoscopic pancreatocholangiogram. Gastroenterology. 63:217–26. DOI: 10.1016/S0016-5085(19)33306-2. PMID: 5048325.36. Kreel L, Sandin B. 1973; Changes in pancreatic morphology associated with aging. Gut. 14:962–70. DOI: 10.1136/gut.14.12.962. PMID: 4785285. PMCID: PMC1412863.
Article37. Kang JK, Chung JB, Moon YM, Choi HJ. 1989; The normal endoscopic pancreatogram in Koreans. Korean J Intern Med. 4:74–9. DOI: 10.3904/kjim.1989.4.1.74. PMID: 2487408. PMCID: PMC4534962.
Article38. Vinay Kumar N, Lokanadham S. 2019; A study on incidence of accessory pancreatic duct and its clinical importance. Maedica (Bucur). 14:22–5. DOI: 10.26574/maedica.2019.14.1.22. PMID: 31123508. PMCID: PMC6511670.39. Hayashi TY, Gonoi W, Yoshikawa T, Hayashi N, Ohtomo K. 2016; Ansa pancreatica as a predisposing factor for recurrent acute pancreatitis. World J Gastroenterol. 22:8940–8. DOI: 10.3748/wjg.v22.i40.8940. PMID: 27833385. PMCID: PMC5083799.
Article40. Govindraj N, Shabna C. 2017; Variations in the duct system of pancreas: a cadaveric study. Int J Anat Res. 5:4136–43. DOI: 10.16965/ijar.2017.269.
Article41. Liessi F, Manfredi R, Liessi G, Mucelli RP. Anatomical variants of the pancreatic ducts. ECR;2010. https://dx.doi.org/10.1594/ecr2010/C-0174. DOI: 10.1594/ecr2010/C-0174.42. Varley PF, Rohrmann CA Jr, Silvis SE, Vennes JA. 1976; The normal endoscopic pancreatogram. Radiology. 118:295–300. DOI: 10.1148/118.2.295. PMID: 1250961.
Article43. Classen M, Hellwig H, Rösch W. 1973; Anatomy of the pancreatic duct a duodenoscopic-radiological study. Endoscopy. 5:14–7. DOI: 10.1055/s-0028-1098203.
Article44. Cotton P. 1974; The normal endoscopic pancreatogram. Endoscopy. 6:65–70. DOI: 10.1055/s-0028-1098599. PMID: 1250961.
Article45. Seifert E, Wagner HH, Otto P. 1973; Value and indication of endoscopic pancreato-cholangiography. Gastroenterol Jpn. 8:205–12. DOI: 10.1007/BF02779900.
Article46. Okuda K, Someya N, Goto A, Kunisaki T, Emura T, Yasumoto M, Shimokawa Y. 1973; Endoscopic pancreato-cholangiography. A preliminary report on technique and diagnostic significance. Am J Roentgenol Radium Ther Nucl Med. 117:437–45. DOI: 10.2214/ajr.117.2.437. PMID: 4346685.47. Sivak MV Jr, Sullivan BH Jr. 1976; Endoscopic retrograde pancreatography: analysis of the normal pancreatogram. Am J Dig Dis. 21:263–9. DOI: 10.1007/BF01095900. PMID: 1266843.48. Ara S, Shahriah S, Begum S. 2011; The length of main pancreatic duct in Bangladeshi cadaver at different age groups. Mymensingh Med J. 20:298–302. PMID: 21522104.49. Kochhar R, Goenka MK, Nagi B, Aggarwal R, Singh K. 1996; Normal pancreatic duct morphology in a north Indian population. Trop Gastroenterol. 17:223–5. PMID: 9094863.50. Sahni D, Jit I, Harjeet . 2001; Gross anatomy of the pancreatic ducts in north Indians. Trop Gastroenterol. 22:197–201. PMID: 11963324.51. Fatima T. 2010; Anatomical variants of pancreatic duct system in human cadavers. J Fatima Jinnah Med Univ. 4:110–7.52. Wilasrusmee C, Pongchairerks P. 1999; Pancreaticobiliary ductal anatomy in Thai people. J Hepatobiliary Pancreat Surg. 6:79–85. DOI: 10.1007/s005340050087. PMID: 10436241.
Article53. Pina L. 2016; Does the accessory pancreatic duct have any protective role in acute biliary pancreatitis? Anatomical findings from cadaver dissections. MOJ Anat Physiol. 2:180. DOI: 10.15406/mojap.2016.02.00071.54. Hastier P, Buckley MJ, Dumas R, Kuhdorf H, Staccini P, Demarquay JF, Caroli-Bosc FX, Delmont JP. 1998; A study of the effect of age on pancreatic duct morphology. Gastrointest Endosc. 48:53–7. DOI: 10.1016/S0016-5107(98)70129-4. PMID: 9684665.
Article55. Akochi S, Ugwu A, Otuh I. 2018; Sonographic measurement of common bile duct diameter in apparently healthy adults in Abakaliki metropolis. Int J Sci Appl Res. 5:1–8.56. Karak PK, Vashisht S, Tandon RK, Berry M. 1991; Normal endoscopic pancreatogram in an Indian referral hospital. Indian J Med Res. 94:426–9. PMID: 1774094.57. Hadidi A. 1983; Pancreatic duct diameter: sonographic measurement in normal subjects. J Clin Ultrasound. 11:17–22. DOI: 10.1002/jcu.1870110105. PMID: 6403583.
Article58. Millbourn E. 1960; Calibre and appearance of the pancreatic ducts and relevant clinical problems. A roentgenographic and anatomical study. Acta Chir Scand. 118:286–303. PMID: 14422445.59. Trapnell JE, Howard JM. 1966; Transduodenal pancreatography: an improved technique. Surgery. 60:1112–9. PMID: 5928106.60. Hand BH. 1963; An anatomical study of the choledochoduodenal area. Br J Surg. 50:486–94. DOI: 10.1002/bjs.18005022303. PMID: 13952484.
Article61. Ogoshi K, Niwa M, Hara Y, Nebel OT. 1973; Endoscopic pancreatocholangiography in the evaluation of pancreatic and biliary disease. Gastroenterology. 64:210–6. DOI: 10.1016/S0016-5085(73)80031-9. PMID: 4686330.
Article62. Birnstingl M. 1959; A study of pancreatography. Br J Surg. 47:128–39. DOI: 10.1002/bjs.18004720203. PMID: 13800918.
Article63. MacCarty RL, Stephens DH, Brown AL Jr, Carlson HC. 1975; Retrograde pancreatography in autopsy specimens. Am J Roentgenol Radium Ther Nucl Med. 123:359–66. DOI: 10.2214/ajr.123.2.359. PMID: 1115312.
Article64. Toda J, Ueno E, Takada Y, Okawa T. 1998; Demonstration of normal bile duct and pancreatic duct with MR cholangiopancreatography. Nihon Rinsho. 56:2830–5. Japanese. PMID: 9847605.65. Aubé C, Hentati N, Tanguy JY, Fournier HD, Papon X, Lebigot J, Mercier P. 2003; Radio-anatomic study of the pancreatic duct by MR cholangiopancreatography. Surg Radiol Anat. 25:64–9. DOI: 10.1007/s00276-002-0082-x. PMID: 12647024.
Article66. Mchonde GJ, Gesase AP. 2014; Termination pattern of the main and accessory pancreatic ducts among Tanzanians. Anat J Afr. 3:223–7.67. Jirasiritham J, Wilasrusmee C, Poprom N, Larbcharoensub N. 2016; Pancreaticobiliary ductal anatomy in the normal population. Asian Pac J Cancer Prev. 17:4363–5. DOI: 10.1016/j.pan.2017.07.034. PMID: 27797245.68. Gosavi V, Gaikwad P. 1980; The duct system of the human pancreatic gland. J Anat Soc India. 29:142–6.69. Cremer M, Toussaint J, Hermanus A, Deltenre M, De Tceuf J, Engelholm L. 1976; Primary chronic pancreatitis. A classification based on endoscopic pancreatography. Acta Gastroenter Belg. 39:522–46. In French. PMID: 1023728.70. Malathi K, Chitra R. 2022; The study of anatomy of accessory pancreatic duct and its variations. Eur J Mol Clin Med. 9:6270–9.71. Nealon WH, Walser E. 2002; Main pancreatic ductal anatomy can direct choice of modality for treating pancreatic pseudocysts (surgery versus percutaneous drainage). Ann Surg. 235:751–8. DOI: 10.1097/00000658-200206000-00001. PMID: 12035030. PMCID: PMC1422503.
Article72. Covantev S. 2018; Pancreas divisum: a reemerging risk factor for pancreatic diseases. Rom J Intern Med. 56:233–42. DOI: 10.2478/rjim-2018-0022. PMID: 30521477.
Article73. de Jong DM, Stassen PM, Poley JW, Fockens P, Timmer R, Voermans RP, Verdonk RC, Bruno MJ, de Jonge PJF. 2021; Clinical outcome of endoscopic therapy in patients with symptomatic pancreas divisum: a Dutch cohort study. Endosc Int Open. 9:E1164–70. DOI: 10.1055/a-1460-7899. PMID: 34222643. PMCID: PMC8216775.
Article74. Testoni PA. 2007; Endoscopic pancreatic duct stent placement for inflammatory pancreatic diseases. World J Gastroenterol. 13:5971–8. DOI: 10.3748/wjg.v13.45.5971. PMID: 18023085. PMCID: PMC4250876.
Article75. Elbanna KY, Jang HJ, Kim TK. 2020; Imaging diagnosis and staging of pancreatic ductal adenocarcinoma: a comprehensive review. Insights Imaging. 11:58. DOI: 10.1186/s13244-020-00861-y. PMID: 32335790. PMCID: PMC7183518.
Article76. Nealon WH, Walser E. 2003; Duct drainage alone is sufficient in the operative management of pancreatic pseudocyst in patients with chronic pancreatitis. Ann Surg. 237:614–20. discussion 620–2. DOI: 10.1097/01.SLA.0000064360.14269.EF. PMID: 12724627. PMCID: PMC1514521.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pathological Classification of Panaeatic Cancer and Precancerous Casion
- Two Cases of Anomalous Termination of the Common Bile Duct and the Pancreatic Duct into the Duodenal Bulb
- Anatomical Variations and Morphological Diversities of the Pancreatic Ductal System: Clinical and ERCP evaluation
- The Relationship of Anatomic Variation of Pancreatic Ductal System and Pancreaticobiliary Diseases
- A Serous Cystic Neoplasm of the Pancreas with Synchronous Pancreatic Ductal Adenocarcinoma