Anat Cell Biol.
2024 Mar;57(1):25-30. 10.5115/acb.23.275.
A novel histologic description of the fibrous networks in the lid-cheek junction and infraorbital region
- Affiliations
-
- 1Division in Anatomy and Developmental Biology, Department of Oral Biology, Human Identification Research Institute, BK21 FOUR Project, Yonsei University College of Dentistry, Seoul, Korea
- 2Maylin Clinic, Seoul, Korea
- 3Yonsei Severance Dental Clinic, Seoul, Korea
- 4Department of Anatomy, College of Medicine, Konkuk University, Chungju, Korea
- 5Department of Anatomy, Chungbuk National University, Cheongju, Korea
- 6Department of Plastic and Reconstructive Surgery, Royal Free Hospital, London, UK
- KMID: 2554238
- DOI: http://doi.org/10.5115/acb.23.275
Abstract
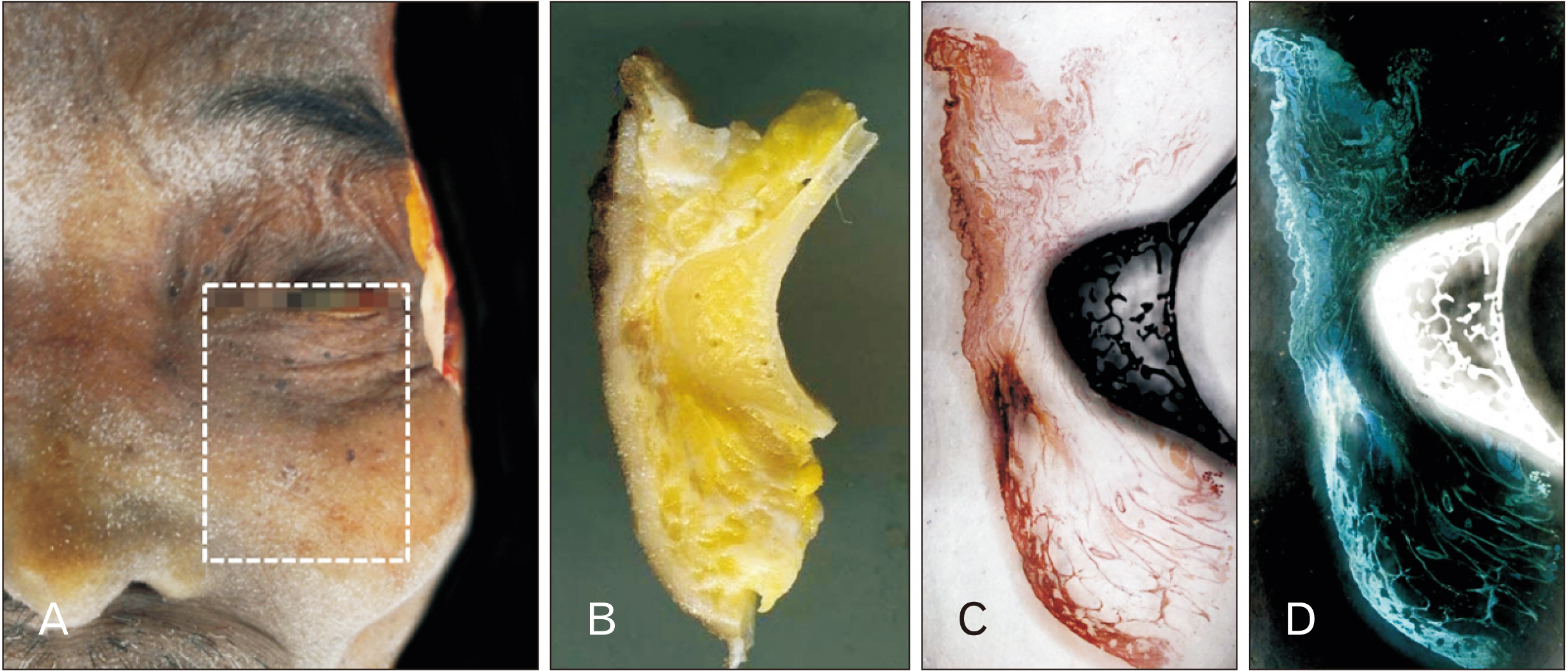
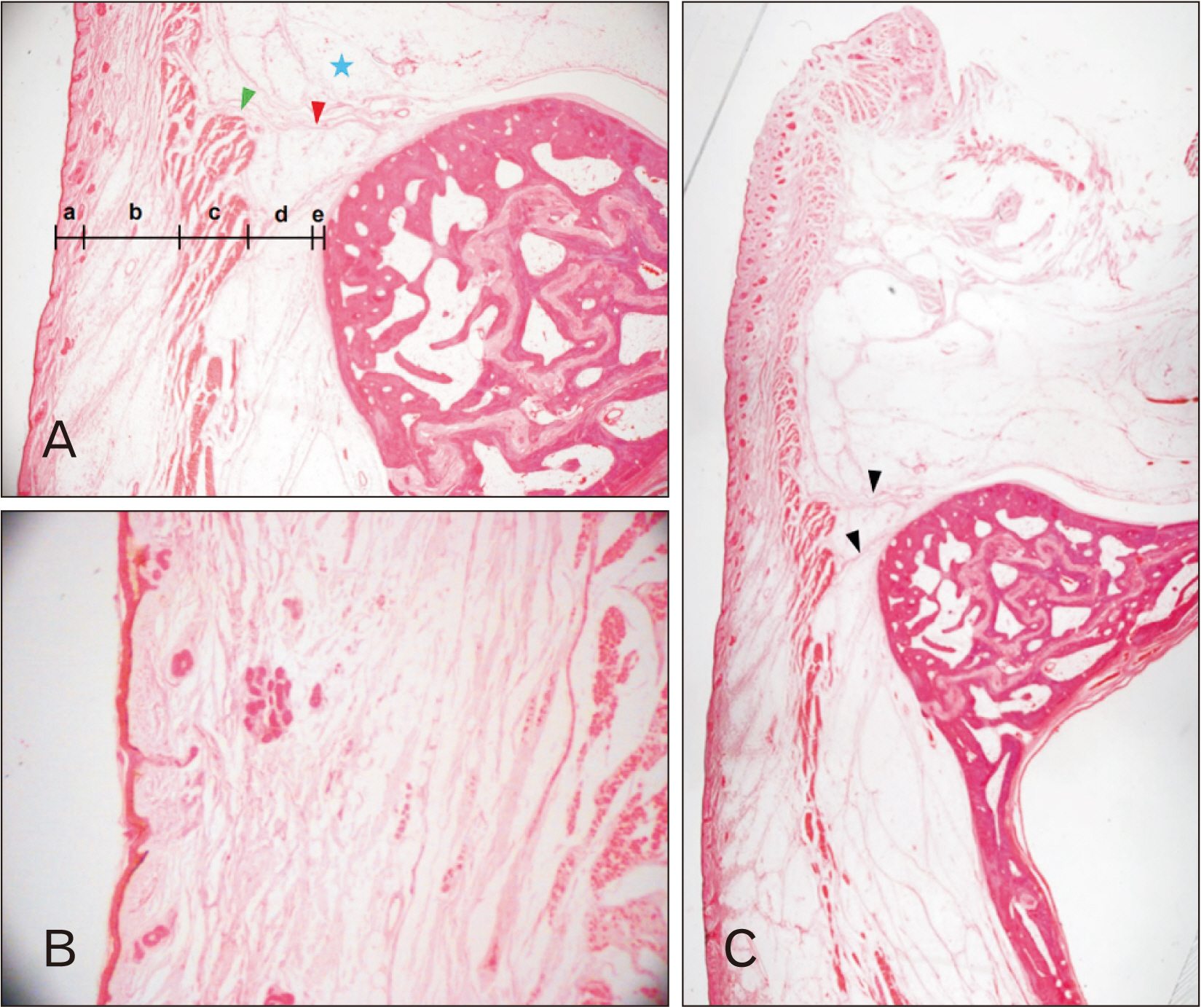
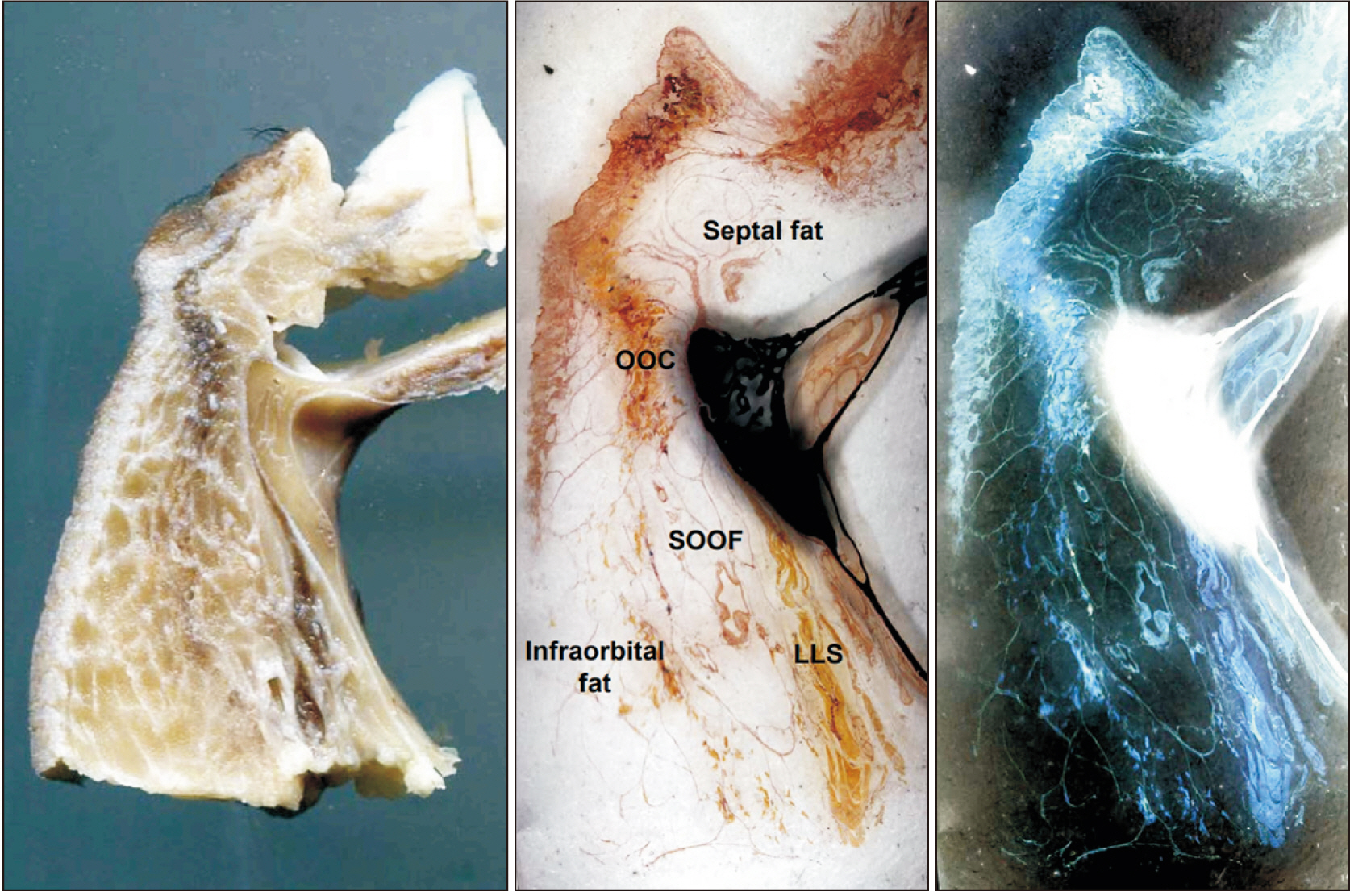
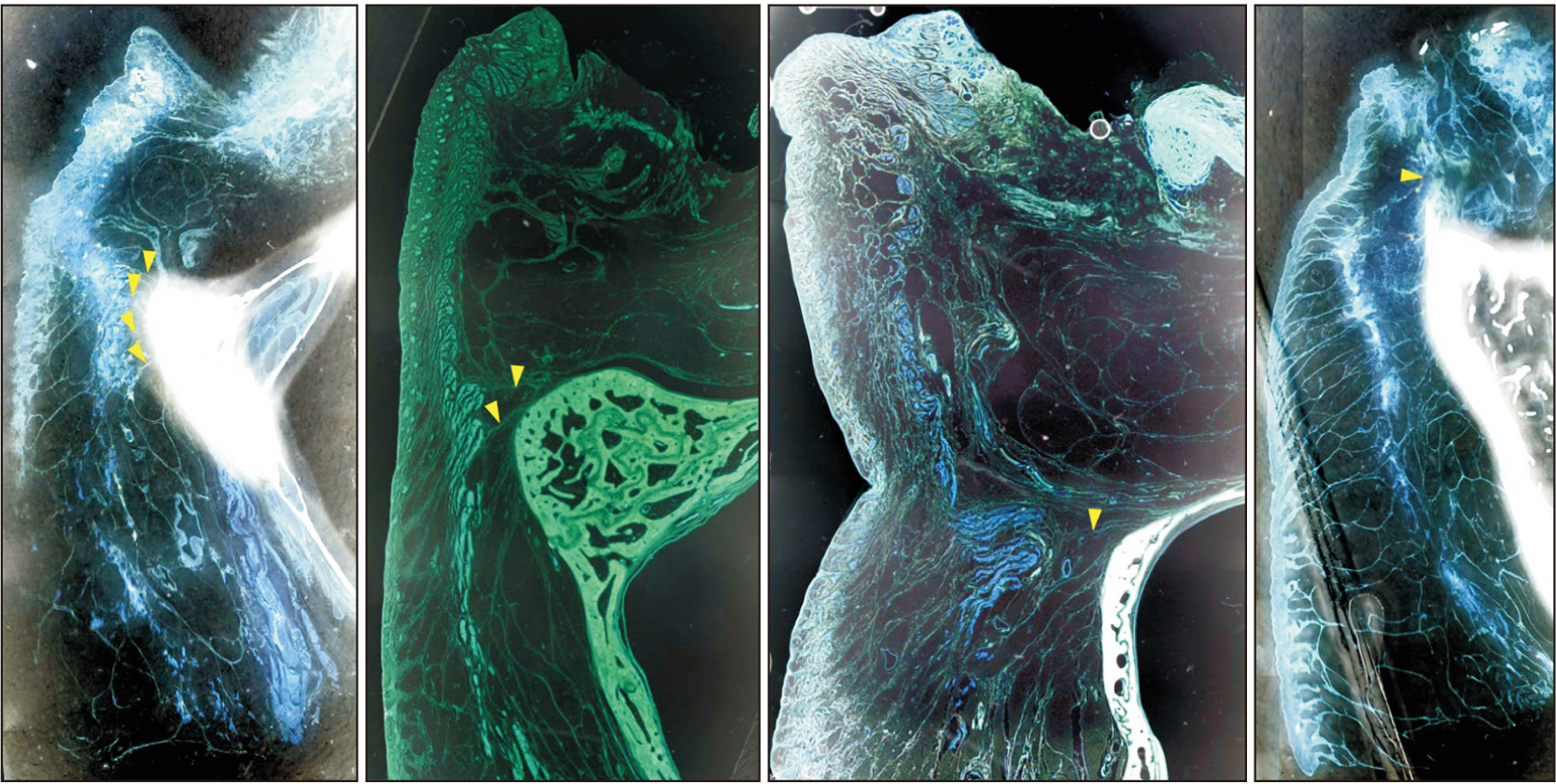
- The aim of this study was to identify the anatomical feature of retaining ligament and fat compartment on the lower eyelid and infraorbital region using a histological method, and to investigate clear definitions for them which could be used generally in the clinical area. Eighteen specimens from eight fresh Korean cadavers were stained with Masson trichrome or hematoxylin and eosin. The ligamentous and fascial fibrous tissue were clearly identified. The ligamentous fibrous tissue which traversed in the superficial and deep fat layer was skin ligament and orbicularis retaining ligament (ORL). The fascial fibrous tissue enclosed the orbicularis oculi muscle (OOc) and circumferencial adipose tissue. Based on the ligamentous and fascial structure, three fat compartments, septal, suborbicularis oculi and infraorbital fat compartment, could be identified. The OOc attached to orbital rim and dermis by ORL and skin ligament, and the muscle fascicle and fat fascicle provided the connection point to the ORL and skin ligament as enclosing all muscle and fat tissue. The combination of the force made by the skin ligament in the lower eyelid and ORL may decide the level and form of the infraorbital grooves.
Figure
Reference
-
References
1. Haddock NT, Saadeh PB, Boutros S, Thorne CH. 2009; The tear trough and lid/cheek junction: anatomy and implications for surgical correction. Plast Reconstr Surg. 123:1332–40. DOI: 10.1097/PRS.0b013e31819f2b36. PMID: 19337101.
Article2. Stuzin JM, Baker TJ, Gordon HL. 1992; The relationship of the superficial and deep facial fascias: relevance to rhytidectomy and aging. Plast Reconstr Surg. 89:441–9. discussion 450–1. DOI: 10.1097/00006534-199203000-00008.3. Wong CH, Hsieh MKH, Mendelson B. 2012; The tear trough ligament: anatomical basis for the tear trough deformity. Plast Reconstr Surg. 129:1392–402. DOI: 10.1097/PRS.0b013e31824ecd77. PMID: 22634656.4. Furnas DW. 1989; The retaining ligaments of the cheek. Plast Reconstr Surg. 83:11–6. DOI: 10.1097/00006534-198901000-00003. PMID: 2909050.
Article5. Nash LG, Phillips MN, Nicholson H, Barnett R, Zhang M. 2004; Skin ligaments: regional distribution and variation in morphology. Clin Anat. 17:287–93. DOI: 10.1002/ca.10203. PMID: 15108331.6. Lambros V. 2007; Observations on periorbital and midface aging. Plast Reconstr Surg. 120:1367–76. DOI: 10.1097/01.prs.0000279348.09156.c3. PMID: 17898614.
Article7. Moss CJ, Mendelson BC, Taylor GI. 2000; Surgical anatomy of the ligamentous attachments in the temple and periorbital regions. Plast Reconstr Surg. 105:1475–90. discussion 1491–8. DOI: 10.1097/00006534-200004000-00034.
Article8. Donofrio LM. 2000; Fat distribution: a morphologic study of the aging face. Dermatol Surg. 26:1107–12. DOI: 10.1046/j.1524-4725.2000.00270.x. PMID: 11134986.
Article9. Rohrich RJ, Pessa JE. 2008; The retaining system of the face: histologic evaluation of the septal boundaries of the subcutaneous fat compartments. Plast Reconstr Surg. 121:1804–9. DOI: 10.1097/PRS.0b013e31816c3c1a. PMID: 18454006.
Article10. Ghavami A, Pessa JE, Janis J, Khosla R, Reece EM, Rohrich RJ. 2008; The orbicularis retaining ligament of the medial orbit: closing the circle. Plast Reconstr Surg. 121:994–1001. DOI: 10.1097/01.prs.0000299941.62645.4e. PMID: 18317148.
Article11. Hwang K, Nam YS, Kim DJ, Han SH. 2008; Surgical anatomy of retaining ligaments in the periorbital area. J Craniofac Surg. 19:800–4. DOI: 10.1097/SCS.0b013e31816b6c5e. PMID: 18520402.
Article12. Byrd HS, Burt JD. 2002; Achieving aesthetic balance in the brow, eyelids, and midface. Plast Reconstr Surg. 110:926–33. discussion 934–9. DOI: 10.1097/01.PRS.0000019877.41086.EB.
Article13. Mendelson BC, Muzaffar AR, Adams WP Jr. 2002; Surgical anatomy of the midcheek and malar mounds. Plast Reconstr Surg. 110:885–96. discussion 897–911. DOI: 10.1097/01.PRS.0000019706.34235.E5.
Article14. Muzaffar AR, Mendelson BC, Adams WP Jr. 2002; Surgical anatomy of the ligamentous attachments of the lower lid and lateral canthus. Plast Reconstr Surg. 110:873–84. discussion 897–911. DOI: 10.1097/00006534-200209010-00025. PMID: 12172154.
Article15. Yang C, Zhang P, Xing X. 2013; Tear trough and palpebromalar groove in young versus elderly adults: a sectional anatomy study. Plast Reconstr Surg. 132:796–808. DOI: 10.1097/PRS.0b0133182a0539e. PMID: 24076672.16. Kim HJ, Seo K.K, Lee HK, Kim J. Clinical anatomy of the face for filler and botulinum toxin injection. Springer;2016. DOI: 10.1007/978-981-10-0240-3.17. Standring S, Gray H. Gray's anatomy: the anatomical basis of clinical practice. 40th ed. Churchill Livingstone/Elsevier;2008.18. Davison SP, Iorio ML, Oh C. 2015; Transconjunctival lower lid blepharoplasty with and without fat repositioning. Clin Plast Surg. 42:51–6. Erratum in: Clin Plast Surg 2017;44:xv. DOI: 10.1016/j.cps.2014.09.001. PMID: 25440740.
Article19. Furnas DW. 1981; The orbicularis oculi muscle. Management in blepharoplasty. Clin Plast Surg. 8:687–715. DOI: 10.1016/S0094-1298(20)30398-9. PMID: 7338003.
Article20. Mendelson BC. 2013; Anatomic study of the retaining ligaments of the face and applications for facial rejuvenation. Aesthetic Plast Surg. 37:513–5. DOI: 10.1007/s00266-013-0066-8. PMID: 23494030. PMCID: PMC3657075.
Article21. Nassif PS. 2005; Lower blepharoplasty: transconjunctival fat repositioning. Facial Plast Surg Clin North Am. 13:553–9. viDOI: 10.1016/j.fsc.2005.06.006. PMID: 16253842.
Article22. Zarem HA, Resnick JI. 1991; Expanded applications for transconjunctival lower lid blepharoplasty. Plast Reconstr Surg. 88:215–20. discussion 221DOI: 10.1097/00006534-199108000-00006.
Article23. Rohrich RJ, Ghavami A, Mojallal A. 2011; The five-step lower blepharoplasty: blending the eyelid-cheek junction. Plast Reconstr Surg. 128:775–83. DOI: 10.1097/PRS.0b013e3182121618. PMID: 21278622.24. Yoo DB, Peng GL, Massry GG. 2013; Transconjunctival lower blepharoplasty with fat repositioning: a retrospective comparison of transposing fat to the subperiosteal vs supraperiosteal planes. JAMA Facial Plast Surg. 15:176–81. DOI: 10.1001/jamafacial.2013.749. PMID: 23471339.
Article