J Korean Diabetes.
2024 Mar;25(1):16-25. 10.4093/jkd.2024.25.1.16.
Chronic Kidney Disease and SGLT2 Inhibitors
- Affiliations
-
- 1Division of Nephrology, Department of Internal Medicine, Yeouido St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2554117
- DOI: http://doi.org/10.4093/jkd.2024.25.1.16
Abstract
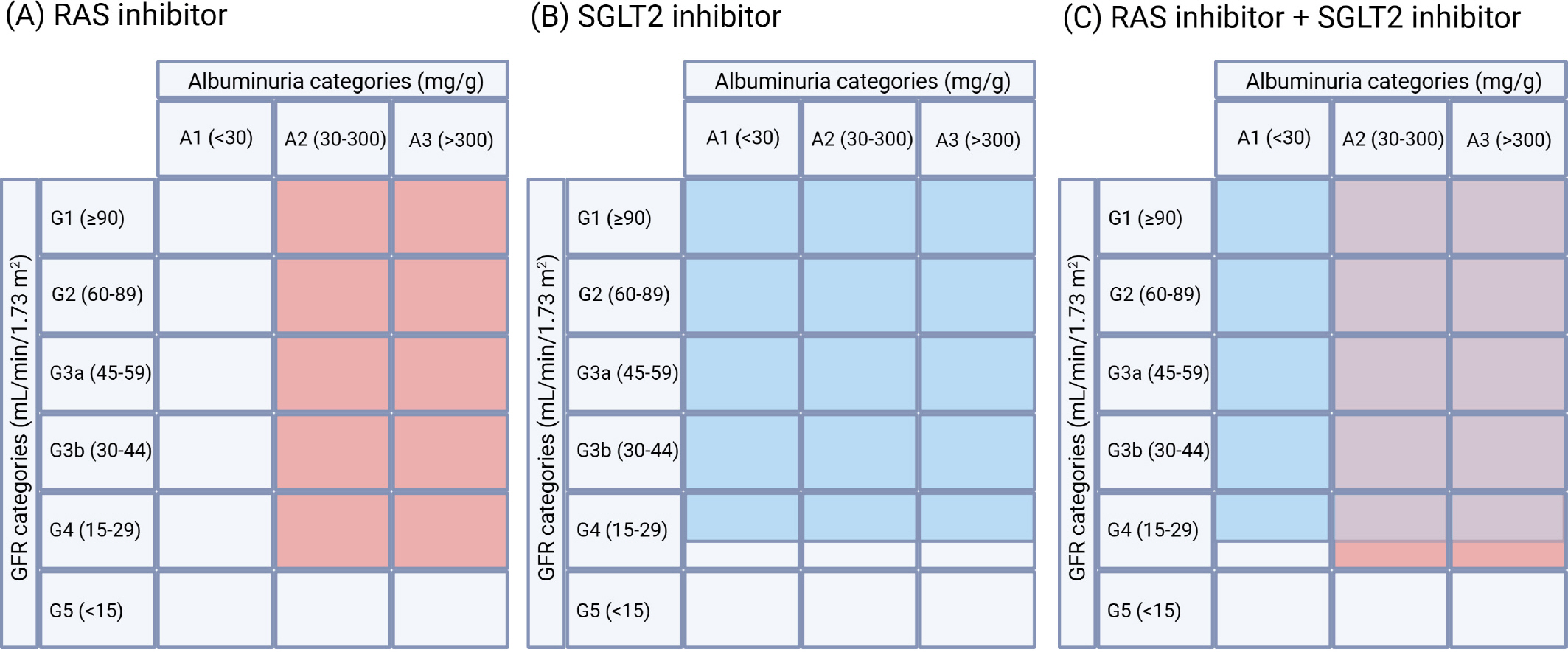
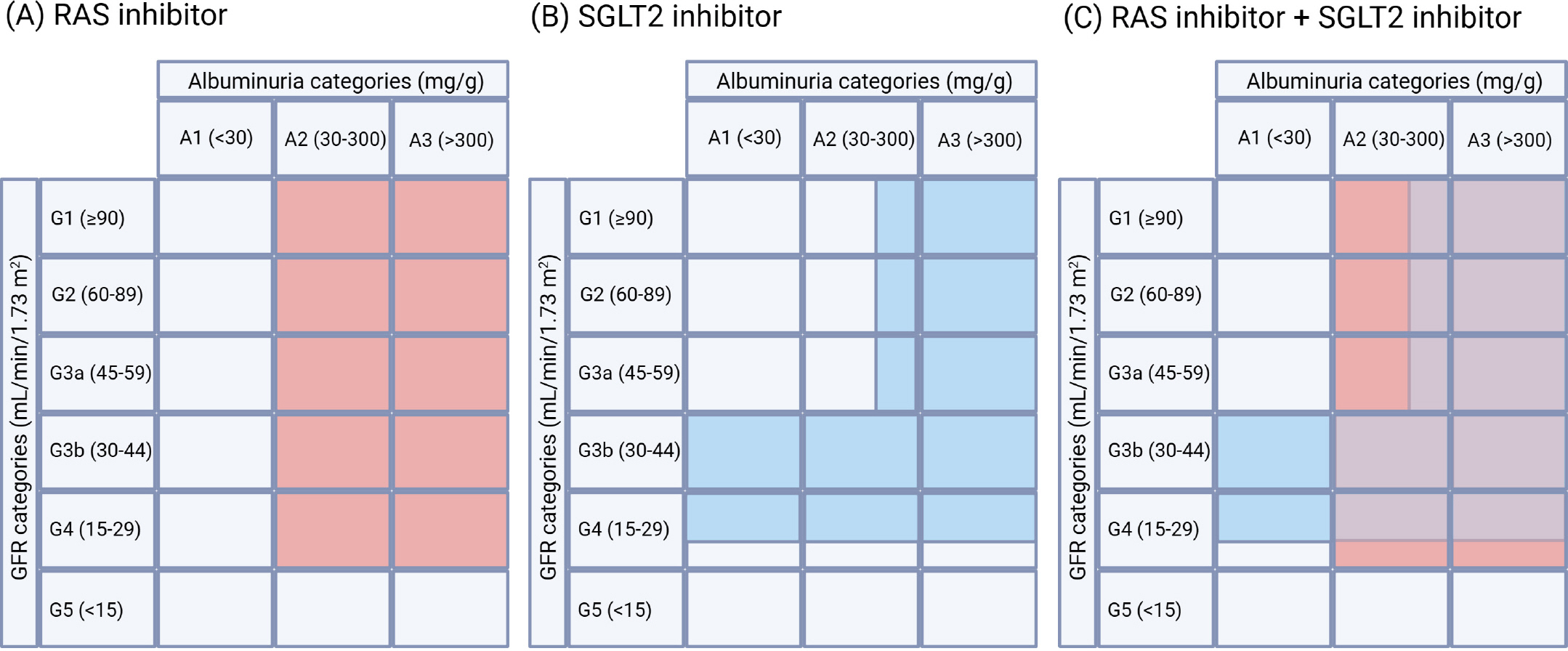
- Sodium glucose cotransporter 2 (SGLT2) inhibitors were initially developed to enhance glycemic control in diabetic patients, but they have emerged as a promising treatment for individuals with chronic kidney disease (CKD) regardless of diabetic status. A collaborative meta-analysis of large-scale SGLT2 inhibitor trials has provided compelling evidence supporting recommendations for the use of these agents in CKD patients, regardless of their primary kidney disease diagnosis or whether they have diabetes. Notably, the kidney-protective benefits of SGLT2 inhibitors have been observed across various stages of CKD, including advanced stage 4 CKD, and across all levels of albuminuria. Given the robust evidence highlighting the benefits of SGLT2 inhibitors across a broad spectrum of CKD patients, these agents should be considered foundational therapy for CKD, in order to mitigate the progression to kidney failure and its associated complications. Although the beneficial effects of SGLT2 inhibitors may not be immediately apparent, they are expected to grow over time, potentially altering the prognosis for numerous CKD patients.
Figure
Reference
-
1.Kovesdy CP. Epidemiology of chronic kidney disease: an update 2022. Kidney Int Suppl (2011). 2022. 12:7–11.
Article2.Murphy D., McCulloch CE., Lin F., Banerjee T., Bragg-Gresham JL., Eberhardt MS., Centers for Disease Control and Prevention Chronic Kidney Disease Surveil-lance Team, et al. Trends in prevalence of chronic kidney disease in the United States. Ann Intern Med. 2016. 165:473–81.
Article3.Aitken GR., Roderick PJ., Fraser S., Mindell JS., O’ Dono-ghue D., Day J, et al. Change in prevalence of chronic kidney disease in England over time: comparison of nationally representative cross-sectional surveys from 2003 to 2010. BMJ Open. 2014. 4:e005480.
Article4.Yoon SY., Park HW., Kim HJ., Kronbichler A., Koyanagi A., Smith L, et al. National trends in the prevalence of chronic kidney disease among Korean adults, 2007-2020. Sci Rep. 2023. 13:5831.
Article5.Kang HT., Lee J., Linton JA., Park BJ., Lee YJ. Trends in the prevalence of chronic kidney disease in Korean adults: the Korean National Health and Nutrition Examination Sur-vey from 1998 to 2009. Nephrol Dial Transplant. 2013. 28:927–36.
Article6.Hsu RK., Powe NR. Recent trends in the prevalence of chronic kidney disease: not the same old song. Curr Opin Nephrol Hypertens. 2017. 26:187–96.7.Hallan SI., Øvrehus MA., Romundstad S., Rifkin D., Lang-hammer A., Stevens PE, et al. Long-term trends in the prevalence of chronic kidney disease and the influence of cardiovascular risk factors in Norway. Kidney Int. 2016. 90:665–73.8.Formentini I., Bobadilla M., Haefliger C., Hartmann G., Loghman-Adham M., Mizrahi J, et al. Current drug de-velopment challenges in chronic kidney disease (CKD)- identification of individualized determinants of renal progression and premature cardiovascular disease (CVD). Nephrol Dial Transplant. 2012. 27(Suppl 3):iii81–8.9.Breyer MD., Susztak K. Developing treatments for chronic kidney disease in the 21st century. Semin Nephrol. 2016. 36:436–47.
Article10.Kim KM., Jeong SA., Ban TH., Hong YA., Hwang SD., Choi SR, et al. Status and trends in epidemiologic characteristics of diabetic end-stage renal disease: an analysis of the 2021 Korean Renal Data System. Kidney Res Clin Pract. 2024. 43:20–32.
Article11.Hong YA., Ban TH., Kang CY., Hwang SD., Choi SR., Lee H, et al. Trends in epidemiologic characteristics of end-stage renal disease from 2019 Korean Renal Data System (KORDS). Kidney Res Clin Pract. 2021. 40:52–61.
Article12.Keener AB. SGLT2 inhibitors breathe life into kidney-disease care. Nature. 2023. 615:S2–4.
Article13.Koh ES., Kim GH., Chung S. Intrarenal mechanisms of sodium-glucose cotransporter-2 inhibitors on tubulo-glomerular feedback and natriuresis. Endocrinol Metab (Seoul). 2023. 38:359–72.
Article14.Mark PB., Sattar N. Implementation, not hesitation, for SGLT2 inhibition as foundational therapy for chronic kidney disease. Lancet. 2022. 400:1745–7.
Article15.Nuffield Department of Population Health Renal Studies Group; SGLT2 inhibitor Meta-Analysis Cardio-Renal Trialists’ Consortium. Impact of diabetes on the effects of sodium glucose co-transporter-2 inhibitors on kidney outcomes: collaborative meta-analysis of large placebo-con-trolled trials. Lancet. 2022. 400:1788–801.16.Zinman B., Wanner C., Lachin JM., Fitchett D., Bluhmki E., Hantel S., EMPA-REG OUTCOME Investigators, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015. 373:2117–28.
Article17.Herrington WG., Staplin N., Wanner C., Green JB., Hauske SJ., Emberson JR, et al. Empagliflozin in patients with chronic kidney disease. N Engl J Med. 2023. 388:117–27.
Article18.Perkovic V., Jardine MJ., Neal B., Bompoint S., Heerspink HJL., Charytan DM., CREDENCE Trial Investigators, et al. Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. N Engl J Med. 2019. 380:2295–306.
Article19.Bhatt DL., Szarek M., Pitt B., Cannon CP., Leiter LA., Mc-Guire DK., SCORED Investigators, et al. Sotagliflozin in patients with diabetes and chronic kidney disease. N Engl J Med. 2021. 384:129–39.
Article20.Heerspink HJL., Stefánsson BV., Correa-Rotter R., Chertow GM., Greene T., Hou FF., DAPA-CKD Trial Com-mittees and Investigators, et al. Dapagliflozin in patients with chronic kidney disease. N Engl J Med. 2020. 383:1436–46.
Article21.Neuen BL., Young T., Heerspink HJL., Neal B., Perkovic V., Billot L, et al. SGLT2 inhibitors for the prevention of kidney failure in patients with type 2 diabetes: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2019. 7:845–54.
Article22.Mark PB., Sarafidis P., Ekart R., Ferro CJ., Balafa O., Fernan-dez-Fernandez B, et al. SGLT2i for evidence-based car-diorenal protection in diabetic and nondiabetic chronic kidney disease: a comprehensive review by EURECA-m and ERBP working groups of ERA. Nephrol Dial Transplant. 2023. 38:2444–55.
Article23.Kidney Disease: Improving Global Outcomes (KDIGO) Diabetes Work Group. KDIGO 2022 clinical practice guideline for diabetes management in chronic kidney disease. Kidney Int. 2022. 102:S1–127.24.Chung S. Synopsis of the Korean Society of Nephrology 2023 practical recommendations for the management of diabetic kidney disease. Korean J Med. 2023. 98:270–82.
Article25.Kidney Disease: Improving Global Outcomes (KDIGO) Blood Pressure Work Group. KDIGO 2021 clinical practice guideline for the management of blood pressure in chronic kidney disease. Kidney Int. 2021. 99:S1–87.26.Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2024 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int. 2024. 105:S117–314.27.Lv J., Guo L., Wang R., Chen J. Efficacy and safety of so-dium-glucose cotransporter-2 inhibitors in nondiabetic patients with chronic kidney disease: a review of recent evidence. Kidney Dis (Basel). 2023. 9:326–41.
Article28.Georgianos PI., Agarwal R. Hypertension in chronic kidney disease-treatment standard 2023. Nephrol Dial Transplant. 2023. 38:2694–703.
Article29.Georgianos PI., Agarwal R. Ambulatory blood pressure reduction with SGLT-2 inhibitors: dose-response meta-analysis and comparative evaluation with low-dose hydro-chlorothiazide. Diabetes Care. 2019. 42:693–700.
Article30.Hao Z., Sun Y., Wen Y., Cui L., Li G., Liu Y. Effects and mechanisms of dapagliflozin treatment on ambulatory blood pressure in diabetic patients with hypertension. Med Sci Monit. 2020. 26:e925987.
Article31.Neuen BL., Oshima M., Agarwal R., Arnott C., Cherney DZ., Edwards R, et al. Sodium-glucose cotransporter 2 inhibitors and risk of hyperkalemia in people with type 2 diabetes: a meta-analysis of individual participant data from randomized, controlled trials. Circulation. 2022. 145:1460–70.
Article32.FitzGerald JD., Dalbeth N., Mikuls T., Brignardello-Peters-en R., Guyatt G., Abeles AM, et al. 2020 American college of rheumatology guideline for the management of gout. Arthritis Care Res (Hoboken). 2020. 72:744–60.
Article33.Iwata Y., Notsu S., Kawamura Y., Mitani W., Tamai S., Morimoto M, et al. The effect of dapagliflozin on uric acid excretion and serum uric acid level in advanced CKD. Sci Rep. 2023. 13:4849.
Article34.Inker LA., Grams ME., Levey AS., Coresh J., Cirillo M., Col-lins JF., CKD Prognosis Consortium, et al. Relationship of estimated GFR and albuminuria to concurrent laboratory abnormalities: an individual participant data meta-analy-sis in a global consortium. Am J Kidney Dis. 2019. 73:206–17.35.Wiviott SD., Raz I., Bonaca MP., Mosenzon O., Kato ET., Cahn A., DECLARE– TIMI 58 Investigators, et al. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2019. 380:347–57.
Article36.McMurray JJV., Solomon SD., Inzucchi SE., Køber L., Kosi-borod MN., Martinez FA., DAPA-HF Trial Commit-tees and Investigators, et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med. 2019. 381:1995–2008.37.Santulli G., Varzideh F., Forzano I., Wilson S., Salemme L., de Donato A, et al. Functional and clinical importance of SGLT2-inhibitors in frailty: from the kidney to the heart. Hypertension. 2023. 80:1800–9.
Article38.Rossing P., Caramori ML., Chan JCN., Heerspink HJL., Hurst C., Khunti K, et al. Executive summary of the KDIGO 2022 clinical practice guideline for diabetes management in chronic kidney disease: an update based on rapid-ly emerging new evidence. Kidney Int. 2022. 102:990–9.39.Morales J., Dagogo-Jack S., Fonseca V., Neumiller JJ., Rosas SE. Perspectives on chronic kidney disease with type 2 diabetes and risk management: practical viewpoints and a paradigm shift using a pillar approach. Clin Diabetes. 2023. 41:553–66.
Article40.Kearney J., Gnudi L. The pillars for renal disease treatment in patients with type 2 diabetes. Pharmaceutics. 2023. 15:1343.
Article41.Agarwal R., Filippatos G., Pitt B., Anker SD., Rossing P., Joseph A., FIDELIO-DKD and FIGARO-DKD investigators, et al. Cardiovascular and kidney outcomes with finerenone in patients with type 2 diabetes and chronic kidney disease: the FIDELITY pooled analysis. Eur Heart J. 2022. 43:474–84.
Article42.Gragnano F., De Sio V., Calabrò P. FLOW trial stopped ear-ly due to evidence of renal protection with semaglutide. Eur Heart J Cardiovasc Pharmacother. 2024. 10:7–9.
Article43.Meraz-Muñoz AY., Weinstein J., Wald R. eGFR decline after SGLT2 inhibitor initiation: the tortoise and the hare reimagined. Kidney360. 2021. 2:1042–7.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- SGLT2 Inhibitors and Diabetes: Where Does It Come from and Where Does It Go?
- Sodium-Glucose Cotransporter 2 Inhibitors for Chronic Kidney Disease: A Comprehensive Review
- Renoprotective Mechanism of Sodium-Glucose Cotransporter 2 Inhibitors: Focusing on Renal Hemodynamics
- Use of dapagliflozin in patients with advanced diabetic kidney disease
- Intrarenal Mechanisms of Sodium-Glucose Cotransporter-2 Inhibitors on Tubuloglomerular Feedback and Natriuresis