Clin Endosc.
2024 Mar;57(2):209-216. 10.5946/ce.2023.022.
Endoscopic ultrasound-guided gastrojejunostomy with a direct technique without previous intestinal filling using a tubular fully covered self-expandable metallic stent
- Affiliations
-
- 1Department of Gastroenterology, Bezmialem Vakif University Medicine Faculty, Istanbul, Turkiye
- 2Department of Gastroenterology, Baskent University Istanbul Hospital, Baskent University Medicine Faculty, Istanbul, Turkiye
- 3Gastroenterology Clinic, Nevsehir Training and Education Hospital, Nevsehir, Turkiye
- KMID: 2553758
- DOI: http://doi.org/10.5946/ce.2023.022
Abstract
- Background/Aims
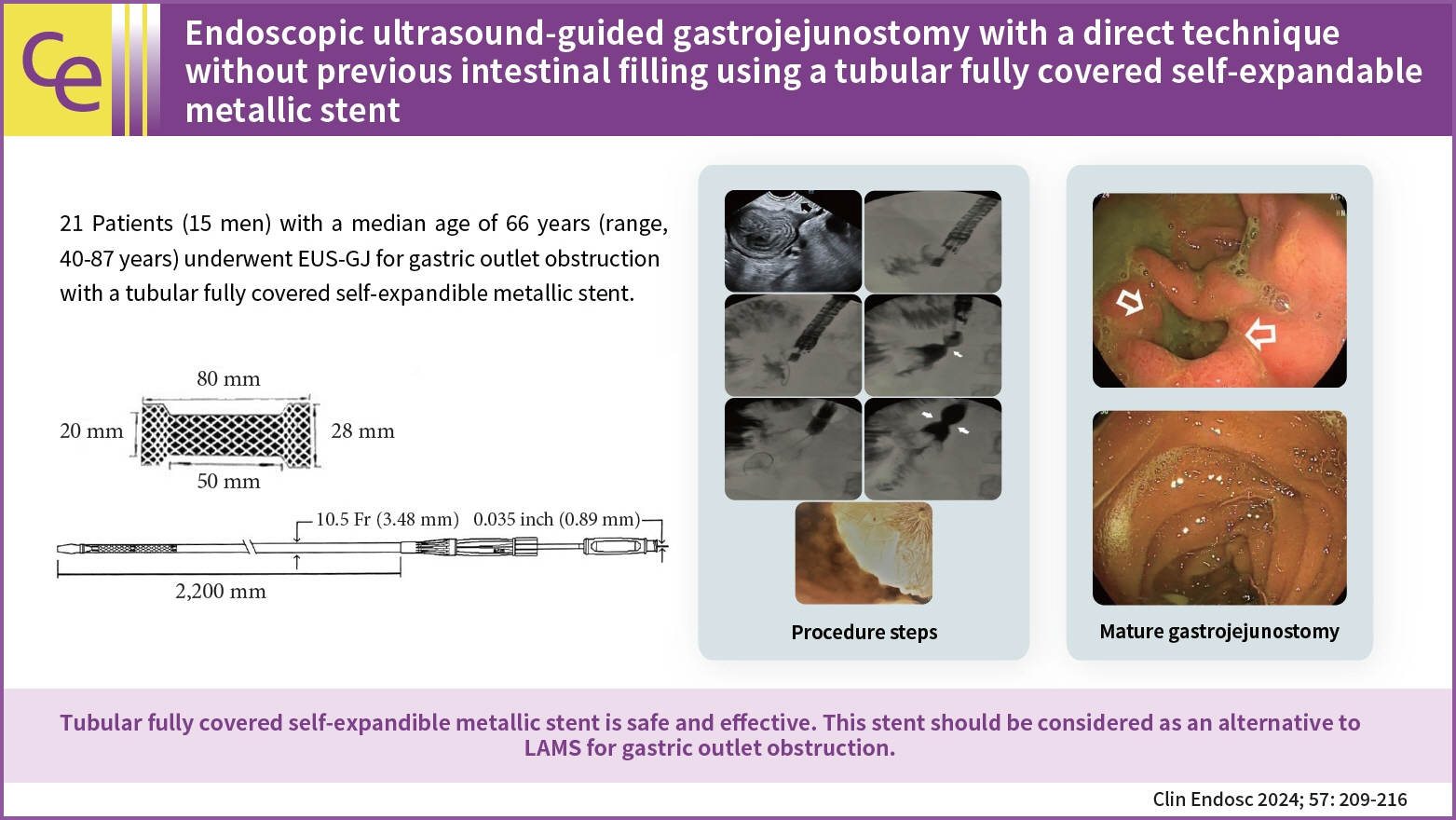
Endoscopic ultrasonography-guided gastrojejunostomy is a minimally invasive method for the management of gastric outlet obstruction. Conventionally, a lumen-apposing metal stent (LAMS) is used to create an anastomosis. However, LAMS is expensive and not widely available. In this report, we described a tubular fully covered self-expandable metallic stent (T-FCSEMS) for this purpose.
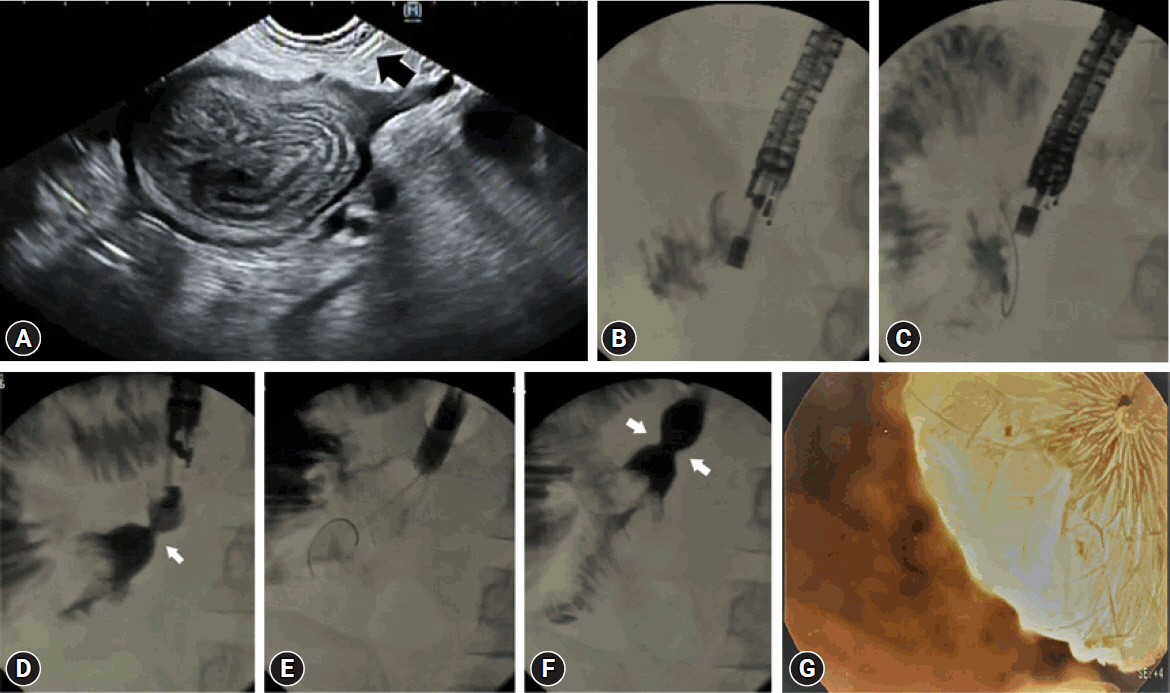
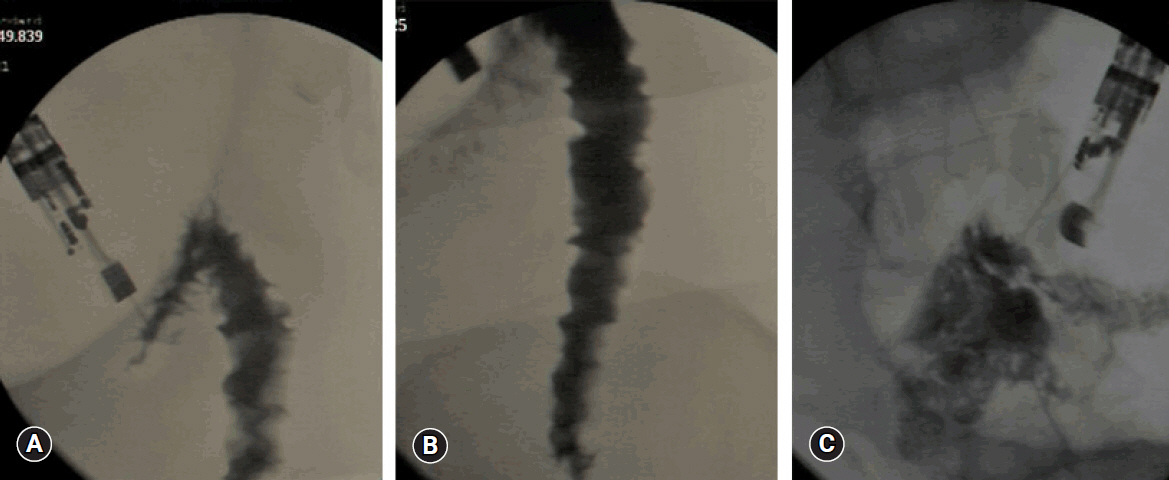
Methods
Twenty-one patients (15 men [71.4%]; median age, 66 years; range, 40–87 years) were included in this study. A total of 19 malignant (12 pancreatic, 6 gastric, and 1 metastatic rectal cancer) and 2 benign cases were observed. The proximal jejunum was punctured with a 19 G needle. The stomach and jejunum walls were dilated with a 6 F cystotome, and a 20×80 mm polytetrafluoroethylene T-FCSEMS (Hilzo) was deployed. Oral feeding was initiated after 12 to 18 hours and solid foods after 48 hours.
Results
The median procedure time was 33 minutes (range, 23–55 minutes). After two weeks, 19 patients tolerated oral feeding. In patients with malignancy, the median survival time was 118 days (range, 41–194 days). No serious complications or deaths occurred. All patients with malignancy tolerated oral food intake until they expired.
Conclusions
T-FCSEMS is safe and effective. This stent should be considered as an alternative to LAMS for gastric outlet obstruction.
Figure
Reference
-
1. Jeurnink SM, Steyerberg EW, van Hooft JE, et al. Surgical gastrojejunostomy or endoscopic stent placement for the palliation of malignant gastric outlet obstruction (SUSTENT study): a multicenter randomized trial. Gastrointest Endosc. 2010; 71:490–499.2. Del Piano M, Ballarè M, Montino F, et al. Endoscopy or surgery for malignant GI outlet obstruction? Gastrointest Endosc. 2005; 61:421–426.3. ASGE Standards of Practice Committee, Fukami N, Anderson MA, et al. The role of endoscopy in gastroduodenal obstruction and gastroparesis. Gastrointest Endosc. 2011; 74:13–21.4. Krishnamoorthi R, Bomman S, Benias P, et al. Efficacy and safety of endoscopic duodenal stent versus endoscopic or surgical gastrojejunostomy to treat malignant gastric outlet obstruction: systematic review and meta-analysis. Endosc Int Open. 2022; 10:E874–E897.5. Rimbas M, Larghi A, Costamagna G. Endoscopic ultrasound-guided gastroenterostomy: are we ready for prime time? Endosc Ultrasound. 2017; 6:235–240.6. Irani S, Baron TH, Itoi T, et al. Endoscopic gastroenterostomy: techniques and review. Curr Opin Gastroenterol. 2017; 33:320–329.7. Tonozuka R, Tsuchiya T, Mukai S, et al. Endoscopic ultrasonography-guided gastroenterostomy techniques for treatment of malignant gastric outlet obstruction. Clin Endosc. 2020; 53:510–518.8. Duan B, Guo J, Ge N, et al. Preliminary use of a double-flanged, fully covered, self-expandable, metal stent with cautery in endoscopic ultrasound-guided gastroenterostomy. Endoscopy. 2018; 50:E29–E31.9. Khashab MA, Kumbhari V, Grimm IS, et al. EUS-guided gastroenterostomy: the first U.S. clinical experience (with video). Gastrointest Endosc. 2015; 82:932–938.10. Chen YI, Kunda R, Storm AC, et al. EUS-guided gastroenterostomy: a multicenter study comparing the direct and balloon-assisted techniques. Gastrointest Endosc. 2018; 87:1215–1221.11. Ge PS, Young JY, Dong W, et al. EUS-guided gastroenterostomy versus enteral stent placement for palliation of malignant gastric outlet obstruction. Surg Endosc. 2019; 33:3404–3411.12. Iqbal U, Khara HS, Hu Y, et al. EUS-guided gastroenterostomy for the management of gastric outlet obstruction: a systematic review and meta-analysis. Endosc Ultrasound. 2020; 9:16–23.13. Kouanda A, Binmoeller K, Hamerski C, et al. Endoscopic ultrasound-guided gastroenterostomy versus open surgical gastrojejunostomy: clinical outcomes and cost effectiveness analysis. Surg Endosc. 2021; 35:7058–7067.14. Fan W, Tan S, Wang J, et al. Clinical outcomes of endoscopic ultrasound-guided gastroenterostomy for gastric outlet obstruction: a systematic review and meta-analysis. Minim Invasive Ther Allied Technol. 2022; 31:159–167.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Tubular fully covered self-expandable metallic stents for endoscopic ultrasound-guided gastrojejunostomy: moving forward or taking a step back?
- Advances in self-expandable metal stents for endoscopic ultrasound-guided interventions
- Follow-up computed tomography can prevent stent migration after endoscopic ultrasound-guided hepaticogastrostomy
- Successful Endoscopic Ultrasound-Guided Treatment of a Spontaneous Rupture of a Hemorrhagic Pancreatic Pseudocyst
- Refractory benign biliary stricture due to chronic pancreatitis in two patients treated using endoscopic ultrasound-guided choledochoduodenostomy fistula creation: case reports