Clin Endosc.
2024 Jan;57(1):122-127. 10.5946/ce.2022.149.
Refractory benign biliary stricture due to chronic pancreatitis in two patients treated using endoscopic ultrasound-guided choledochoduodenostomy fistula creation: case reports
- Affiliations
-
- 1Department of Gastroenterology, Aichi Cancer Center Hospital, Nagoya, Japan
- KMID: 2551201
- DOI: http://doi.org/10.5946/ce.2022.149
Abstract
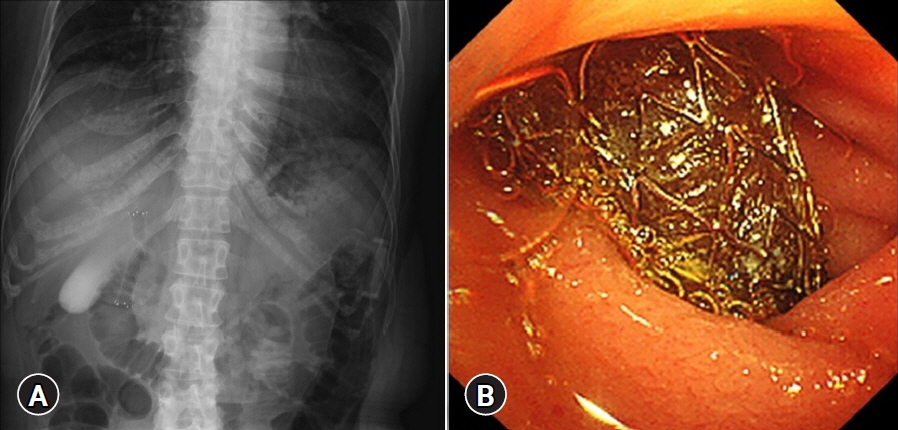
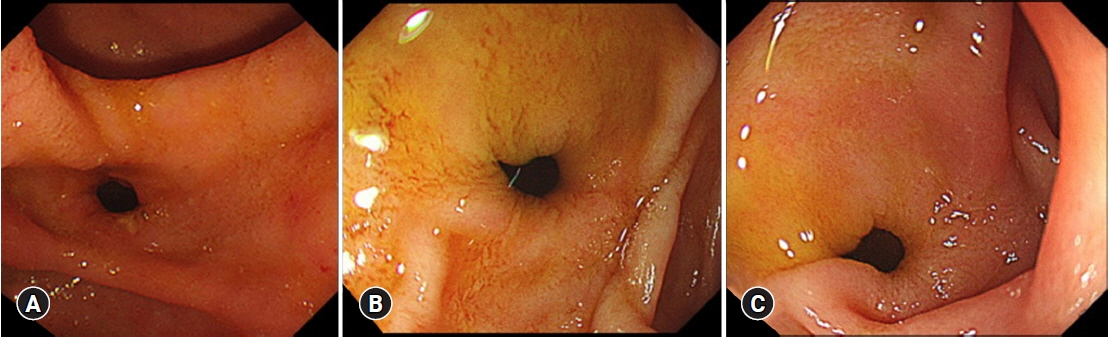
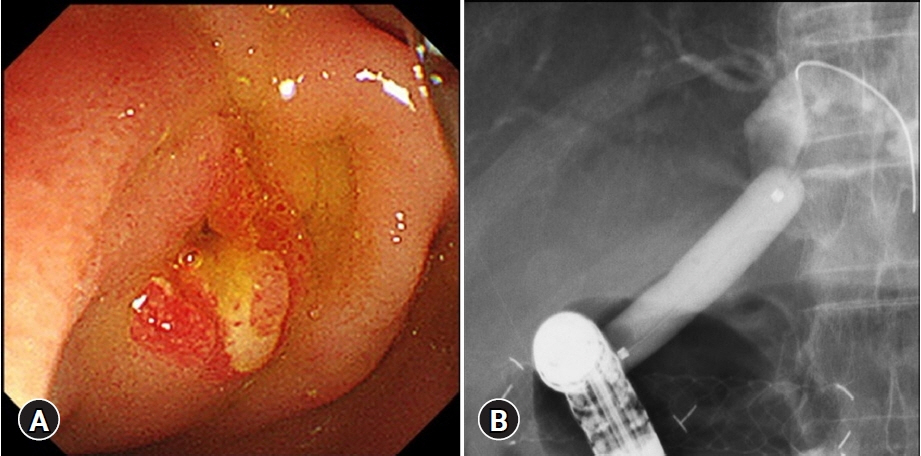
- Benign biliary stricture (BBS) is a complication of chronic pancreatitis (CP). Despite endoscopic biliary stenting, some patients do not respond to treatment, and they experience recurrent cholangitis. We report two cases of CP with refractory BBS treated using endoscopic ultrasound-guided choledochoduodenostomy (EUS-CDS) fistula creation. A 50-year-old woman and a 60-year-old man both presented with obstructive jaundice secondary to BBS due to alcoholic CP. They underwent repeated placement of a fully covered self-expandable metal stent for biliary strictures. However, the strictures persisted, causing repeated episodes of cholangitis. Therefore, an EUS-CDS was performed. The stents were eventually removed and the patients became stent-free. These fistulas have remained patent without cholangitis for more than 2.5 years. Fistula creation using EUS-CDS is an effective treatment option for BBS.
Keyword
Figure
Reference
-
1. Abdallah AA, Krige JE, Bornman PC. Biliary tract obstruction in chronic pancreatitis. HPB (Oxford). 2007; 9:421–428.2. Wong MY, Saxena P, Kaffes AJ. Benign biliary strictures: a systematic review on endoscopic treatment options. Diagnostics (Basel). 2020; 10:221.3. Dumonceau JM, Delhaye M, Tringali A, et al. Endoscopic treatment of chronic pancreatitis: European Society of Gastrointestinal Endoscopy (ESGE) guideline: updated August 2018. Endoscopy. 2019; 51:179–193.4. Ramchandani M, Lakhtakia S, Costamagna G, et al. Fully covered self-expanding metal stent vs multiple plastic stents to treat benign biliary strictures secondary to chronic pancreatitis: a multicenter randomized trial. Gastroenterology. 2021; 161:185–195.5. Ma MX, Jayasekeran V, Chong AK. Benign biliary strictures: prevalence, impact, and management strategies. Clin Exp Gastroenterol. 2019; 12:83–92.6. Lakhtakia S, Reddy N, Dolak W, et al. Long-term outcomes after temporary placement of a self-expanding fully covered metal stent for benign biliary strictures secondary to chronic pancreatitis. Gastrointest Endosc. 2020; 91:361–369.7. Artifon EL, Visconti TA, Brunaldi VO. Choledochoduodenostomy: outcomes and limitations. Endosc Ultrasound. 2019; 8(Suppl 1):S72–S78.8. Pawa R, Pleasant T, Tom C, et al. Endoscopic ultrasound-guided biliary drainage: are we there yet? World J Gastrointest Endosc. 2021; 13:302–318.9. Hara K, Yamao K, Hijioka S, et al. Prospective clinical study of endoscopic ultrasound-guided choledochoduodenostomy with direct metallic stent placement using a forward-viewing echoendoscope. Endoscopy. 2013; 45:392–396.10. Kuraoka N, Hara K, Okuno N, et al. Outcomes of EUS-guided choledochoduodenostomy as primary drainage for distal biliary obstruction with covered self-expandable metallic stents. Endosc Int Open. 2020; 8:E861–E868.11. Ogura T, Itoi T. Technical tips and recent development of endoscopic ultrasound-guided choledochoduodenostomy. DEN Open. 2021; 1:e8.12. Paik WH, Lee TH, Park DH, et al. EUS-guided biliary drainage versus ERCP for the primary palliation of malignant biliary obstruction: a multicenter randomized clinical trial. Am J Gastroenterol. 2018; 113:987–997.13. Matsumoto S, Hara K, Mizuno N, et al. Risk factor analysis for adverse events and stent dysfunction of endoscopic ultrasound-guided choledochoduodenostomy. Dig Endosc. 2020; 32:957–966.14. Iwai T, Kida M, Yamauchi H, et al. Long-lasting patent fistula after EUS-guided choledochoduodenostomy in a patient with refractory benign biliary stricture. VideoGIE. 2018; 3:193–195.15. Akiyama D, Hamada T, Nakai Y, et al. Placement of multiple metal stents for malignant intrahepatic biliary obstruction via an endoscopic ultrasound-guided choledochoduodenostomy fistula. Arab J Gastroenterol. 2015; 16:145–147.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic Management of Pancreatobiliary Stricture in Chronic Pancreatitis
- Recent development of endoscopic ultrasound-guided biliary drainage
- An unusual stent migration after endoscopic ultrasound-guided choledochoduodenostomy
- Fracture of Self-Expandable Metal Stent during Endoscopic Removal in Benign Biliary Stricture
- Endoscopic Ultrasound-Guided Hepaticogastrostomy: Technical Review and Tips to Prevent Adverse Events