Clin Endosc.
2024 Mar;57(2):203-208. 10.5946/ce.2023.111.
Novel upper gastrointestinal bleeding sensor capsule: a first human feasibility and safety trial
- Affiliations
-
- 1Department of Gastroenterology and Hepatology, Institute for Clinical and Experimental Medicine, Prague, Czech Republic
- 2EnteraSense Limited, Galway, Ireland
- KMID: 2553757
- DOI: http://doi.org/10.5946/ce.2023.111
Abstract
- Background/Aims
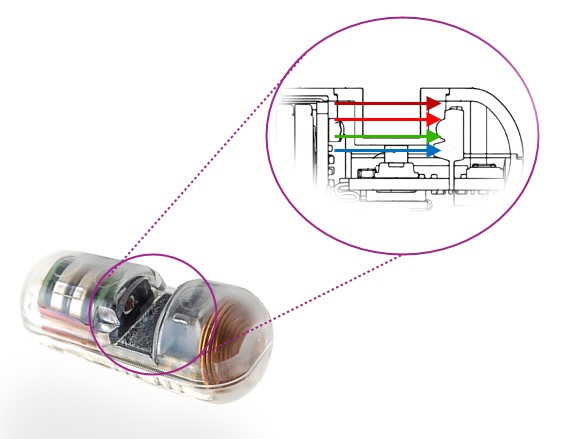
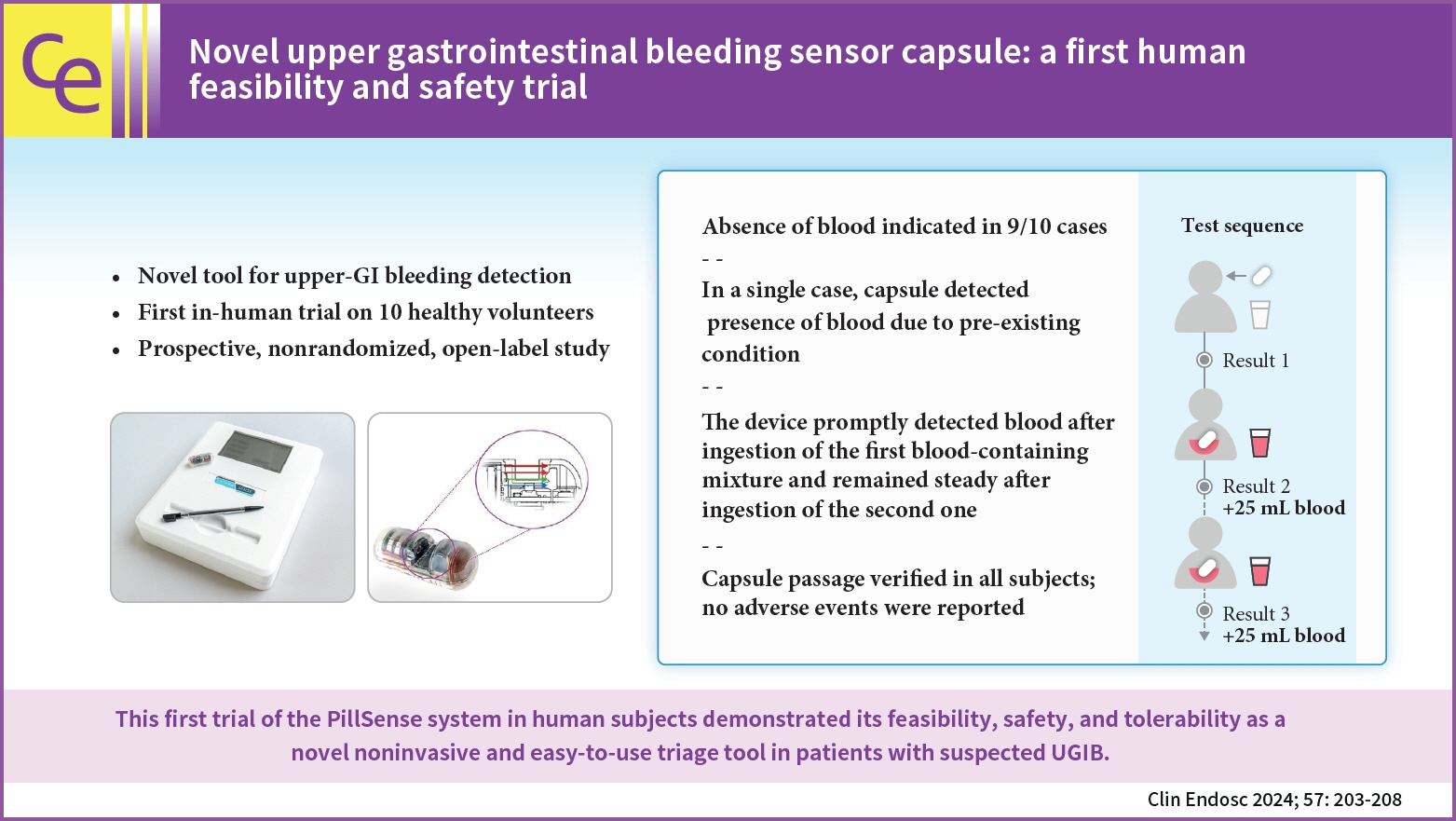
Upper gastrointestinal bleeding (UGIB) is the most common GI condition requiring hospitalization, and can be diagnosed by direct visualization. The present study aimed to evaluate the safety and feasibility of using the PillSense system (EnteraSense Ltd.), a novel diagnostic tool designed for the rapid in vivo detection of UGIB, in human volunteers.
Methods
In the present study, 10 volunteers swallowed a PillSense capsule, followed by 2 servings of an autologous blood preparation. Participants were monitored for capsule passage, overall tolerability of the procedure, and adverse events.
Results
The procedure was completed per the protocol established in the present study in 9/10 cases. In 9 of the subjects, after capsule ingestion, the device indicated the absence of blood with sensor output values of 1. After the ingestion of the first blood mixture, the sensor outputs of all devices increased from 2.8 to 4, indicating that each camera detected blood. The sensor output remained within that range after the ingestion of the second mixture; however, in one case, the baseline capsule signal was positive, because of a preexisting condition. The passage of the capsule was verified in all patients, and no adverse events were reported.
Conclusions
The first trial of the PillSense system in human subjects demonstrated the feasibility, safety, and tolerability of utilizing this product as a novel, noninvasive, and easy-to-use triage tool for the diagnosis of patients suspected of having UGIB.
Keyword
Figure
Reference
-
1. Peery AF, Crockett SD, Murphy CC, et al. Burden and cost of gastrointestinal, liver, and pancreatic diseases in the United States: update 2021. Gastroenterology. 2022; 162:621–644.2. Oakland K. Changing epidemiology and etiology of upper and lower gastrointestinal bleeding. Best Pract Res Clin Gastroenterol. 2019; 42-43:101610.3. Sung JJ, Laine L, Kuipers EJ, et al. Towards personalised management for non-variceal upper gastrointestinal bleeding. Gut. 2021; 70:818–824.4. Sengupta N. Integrating gastrointestinal bleeding risk scores into clinical practice. Am J Gastroenterol. 2019; 114:1699–1703.5. Blatchford O, Murray WR, Blatchford M. A risk score to predict need for treatment for upper-gastrointestinal haemorrhage. Lancet. 2000; 356:1318–1321.6. Saltzman JR, Tabak YP, Hyett BH, et al. A simple risk score accurately predicts in-hospital mortality, length of stay, and cost in acute upper GI bleeding. Gastrointest Endosc. 2011; 74:1215–1224.7. Rockall TA, Logan RF, Devlin HB, et al. Risk assessment after acute upper gastrointestinal haemorrhage. Gut. 1996; 38:316–321.8. Laine L, Barkun AN, Saltzman JR, et al. ACG Clinical guideline: upper gastrointestinal and ulcer bleeding. Am J Gastroenterol. 2021; 116:899–917.9. Gralnek IM, Stanley AJ, Morris AJ, et al. Endoscopic diagnosis and management of nonvariceal upper gastrointestinal hemorrhage (NVUGIH): European Society of Gastrointestinal Endoscopy (ESGE) guideline: update 2021. Endoscopy. 2021; 53:300–332.10. Barkun AN, Laine L, Leontiadis GI, et al. Management of nonvariceal upper gastrointestinal bleeding. Ann Intern Med. 2020; 172:573.11. Meltzer AC, Ward MJ, Gralnek IM, et al. The cost-effectiveness analysis of video capsule endoscopy compared to other strategies to manage acute upper gastrointestinal hemorrhage in the ED. Am J Emerg Med. 2014; 32:823–832.12. Rubin M, Hussain SA, Shalomov A, et al. Live view video capsule endoscopy enables risk stratification of patients with acute upper GI bleeding in the emergency room: a pilot study. Dig Dis Sci. 2011; 56:786–791.13. Papaefthymiou A, Koffas A, Laskaratos FM, et al. Upper gastrointestinal video capsule endoscopy: the state of the art. Clin Res Hepatol Gastroenterol. 2022; 46:101798.14. Schembre DB, Ely RE, Connolly JM, et al. Semiautomated Glasgow-Blatchford bleeding score helps direct bed placement for patients with upper gastrointestinal bleeding. BMJ Open Gastroenterol. 2020; 7:e000479.15. ASGE Standards of Practice Committee, Chandrasekhara V, Early DS, et al. Modifications in endoscopic practice for the elderly. Gastrointest Endosc. 2013; 78:1–7.16. Stolow E, Moreau C, Sayana H, et al. Management of non-variceal upper GI bleeding in the geriatric population: an update. Curr Gastroenterol Rep. 2021; 23:5.17. Ahmed A, Armstrong M, Robertson I, et al. Upper gastrointestinal bleeding in Scotland 2000-2010: improved outcomes but a significant weekend effect. World J Gastroenterol. 2015; 21:10890–10897.18. Gupta A, Agarwal R, Ananthakrishnan AN. “Weekend effect” in patients with upper gastrointestinal hemorrhage: a systematic review and meta-analysis. Am J Gastroenterol. 2018; 113:13–21.19. Forbes N, Chau M, Koury HF, et al. Development and validation of a patient-reported scale for tolerability of endoscopic procedures using conscious sedation. Gastrointest Endosc. 2021; 94:103–110.20. Wilcox CM, Alexander LN, Cotsonis G. A prospective characterization of upper gastrointestinal hemorrhage presenting with hematochezia. Am J Gastroenterol. 1997; 92:231–235.21. Al Hillan A, Curras-Martin D, Carson M, et al. Capsule endoscopy transit time to duodenum: relation to patient demographics. Cureus. 2020; 12:e6894.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Could a bleeding-sensor device be established as a new paradigm for detecting upper gastrointestinal bleeding before performing endoscopy?
- Chronic Bleeding due to Jejunal Gatrointestinal Stromal Tumor Diagnosed by Capsule Endoscopy
- Preclinical study of a novel ingestible bleeding sensor for upper gastrointestinal bleeding
- A Case of Small Bowel Polyp Bleeding Diagnosed by Capsule Endoscopy
- Endoscopic Management of Nonvariceal Upper Gastrointestinal Bleeding