J Korean Med Sci.
2024 Mar;39(9):e88. 10.3346/jkms.2024.39.e88.
Risk of Cerebral Aneurysm Rupture After Liver Transplantation: Development and Validation of a Hemorrhagic Stroke Scoring Model
- Affiliations
-
- 1Department of Neurosurgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 2Division of Hepatobiliary Surgery and Liver Transplantation, Department of Surgery, Asan Medical Centre, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2553337
- DOI: http://doi.org/10.3346/jkms.2024.39.e88
Abstract
- Background
Liver transplantation (LT) patients appear to be more prone to neurological events compared to individuals undergoing other types of solid-organ transplantation. The aims of the present study were to analyze the prevalence of unruptured intracranial aneurysms (UIAs) in patients undergoing liver transplantation (LT) and to examine the perioperative occurrence of subarachnoid hemorrhage (SAH). Also, it intended to systematically identify the risk factors of SAH and hemorrhagic stroke (HS) within a year after LT and to develop a scoring system which involves distinct clinical features of LT patients.
Methods
Patients who underwent LT from January 2012 to March 2022 were analyzed. All included patients underwent neurovascular imaging within 6 months before LT. We conducted an analysis of prevalence and radiological features of UIA and SAH. The clinical factors that may have an impact on HS within one year of LT were also reviewed.
Results
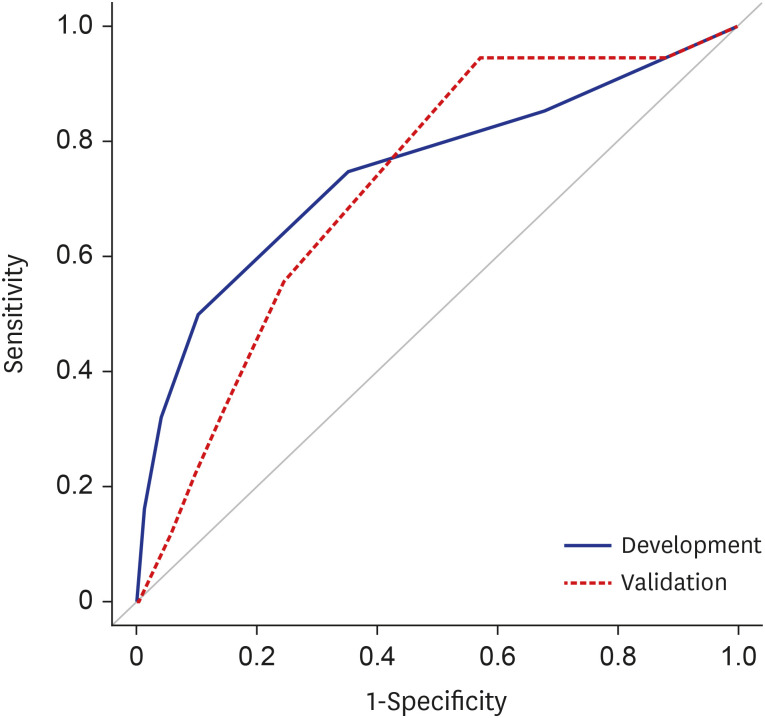
Total of 3,487 patients were enrolled in our study after applying inclusion and exclusion criteria. The prevalence of UIA was 5.4%. The incidence of SAH and HS within one year following LT was 0.5% and 1.6%, respectively. We developed a scoring system based on multivariable analysis to predict the HS within 1-year after LT. The variables were a poor admission mental status, the diagnosis of UIA, serum ammonia levels, and Model for End-stage Liver Disease (MELD) scores. Our model showed good discrimination among the development (C index, 0.727; 95% confidence interval [CI], 0.635–0.820) and validation (C index, 0.719; 95% CI, 0.598–0.801) cohorts.
Conclusion
The incidence of UIA and SAH was very low in LT patients. A poor admission mental status, diagnosis of UIA, serum ammonia levels, and MELD scores were significantly associated with the risk of HS within one year after LT. Our scoring system showed a good discrimination to predict the HS in LT patients.
Keyword
Figure
Reference
-
1. Oliveira CP, Stefano JT, Alvares-da-Silva MR. Cardiovascular risk, atherosclerosis and metabolic syndrome after liver transplantation: a mini review. Expert Rev Gastroenterol Hepatol. 2013; 7(4):361–364. PMID: 23639094.2. Ahn C, Koo TY, Jeong JC, Kim M, Yang J, Lee J, et al. Initial report of the Korean Organ Transplant Registry: the first report of national kidney transplantation data. Transplant Proc. 2014; 46(2):425–430. PMID: 24655980.3. Wang JH, Skeans MA, Israni AK. Current status of kidney transplant outcomes: dying to survive. Adv Chronic Kidney Dis. 2016; 23(5):281–286. PMID: 27742381.4. Vizzini G, Asaro M, Miraglia R, Gruttadauria S, Filì D, D’Antoni A, et al. Changing picture of central nervous system complications in liver transplant recipients. Liver Transpl. 2011; 17(11):1279–1285. PMID: 21770016.5. Saner FH, Sotiropoulos GC, Gu Y, Paul A, Radtke A, Gensicke J, et al. Severe neurological events following liver transplantation. Arch Med Res. 2007; 38(1):75–79. PMID: 17174727.6. Kim BS, Lee SG, Hwang S, Park KM, Kim KH, Ahn CS, et al. Neurologic complications in adult living donor liver transplant recipients. Clin Transplant. 2007; 21(4):544–547. PMID: 17645717.7. Bronster DJ, Emre S, Boccagni P, Sheiner PA, Schwartz ME, Miller CM. Central nervous system complications in liver transplant recipients--incidence, timing, and long-term follow-up. Clin Transplant. 2000; 14(1):1–7. PMID: 10693627.8. Senzolo M, Ferronato C, Burra P. Neurologic complications after solid organ transplantation. Transpl Int. 2009; 22(3):269–278. PMID: 19076332.9. Kumar SS, Mashour GA, Picton P. Neurologic considerations and complications related to liver transplantation. Anesthesiology. 2018; 128(5):1008–1014. PMID: 29498949.10. Thompson BG, Brown RD Jr, Amin-Hanjani S, Broderick JP, Cockroft KM, Connolly ES Jr, et al. Guidelines for the management of patients with unruptured intracranial aneurysms: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2015; 46(8):2368–2400. PMID: 26089327.11. Mesquita GL, Yokoyama AP, de Souza CM, Kutner JM, de Almeida MD, Vaz CO, et al. Role of microvesicles as markers of inflammation and adverse clinical outcomes in orthotopic liver transplantation. J Liver Transpl. 2023; 9:100138.12. Chalouhi N, Ali MS, Jabbour PM, Tjoumakaris SI, Gonzalez LF, Rosenwasser RH, et al. Biology of intracranial aneurysms: role of inflammation. J Cereb Blood Flow Metab. 2012; 32(9):1659–1676. PMID: 22781330.13. Moreno R, Berenguer M. Post-liver transplantation medical complications. Ann Hepatol. 2006; 5(2):77–85. PMID: 16807513.14. Parikh NS, Navi BB, Schneider Y, Jesudian A, Kamel H. Association between cirrhosis and stroke in a nationally representative cohort. JAMA Neurol. 2017; 74(8):927–932. PMID: 28586894.15. Parikh NS, Merkler AE, Jesudian A, Kamel H. Association between cirrhosis and aneurysmal subarachnoid hemorrhage. Ann Clin Transl Neurol. 2018; 6(1):27–32. PMID: 30656181.16. Cebral JR, Mut F, Weir J, Putman CM. Association of hemodynamic characteristics and cerebral aneurysm rupture. AJNR Am J Neuroradiol. 2011; 32(2):264–270. PMID: 21051508.17. Weiss N, Thabut D. Neurological complications occurring after liver transplantation: role of risk factors, hepatic encephalopathy, and acute (on chronic) brain injury. Liver Transpl. 2019; 25(3):469–487. PMID: 30697911.18. UCAS Japan Investigators. Morita A, Kirino T, Hashi K, Aoki N, Fukuhara S, et al. The natural course of unruptured cerebral aneurysms in a Japanese cohort. N Engl J Med. 2012; 366(26):2474–2482. PMID: 22738097.19. Greving JP, Wermer MJ, Brown RD Jr, Morita A, Juvela S, Yonekura M, et al. Development of the PHASES score for prediction of risk of rupture of intracranial aneurysms: a pooled analysis of six prospective cohort studies. Lancet Neurol. 2014; 13(1):59–66. PMID: 24290159.20. Frontera JA, Claassen J, Schmidt JM, Wartenberg KE, Temes R, Connolly ES Jr, et al. Prediction of symptomatic vasospasm after subarachnoid hemorrhage: the modified fisher scale. Neurosurgery. 2006; 59(1):21–27. PMID: 16823296.21. Chung Y, Lee S, Park JC, Ahn JS, Moon EJ, Park JW, et al. Prevalence of cerebrovascular diseases that can cause hemorrhagic stroke in liver transplantation recipients: a 6-year comparative study with 24,681 healthy adults. Neurol Sci. 2021; 42(7):2753–2761. PMID: 33125597.22. Hoh BL, Ko NU, Amin-Hanjani S, Chou SH, Cruz-Flores S, Dangayach NS, et al. 2023 Guideline for the management of patients with aneurysmal subarachnoid hemorrhage: a guideline from the American Heart Association/American Stroke Association. Stroke. 2023; 54(7):e314–e370. PMID: 37212182.23. Greenberg SM, Ziai WC, Cordonnier C, Dowlatshahi D, Francis B, Goldstein JN, et al. 2022 Guideline for the management of patients with spontaneous intracerebral hemorrhage: a guideline from the American Heart Association/American Stroke Association. Stroke. 2022; 53(7):e282–e361. PMID: 35579034.24. Kim T, Lee H, Ahn S, Kwon OK, Bang JS, Hwang G, et al. Incidence and risk factors of intracranial aneurysm: a national cohort study in Korea. Int J Stroke. 2016; 11(8):917–927. PMID: 27422699.25. Kwon HM, Jun IG, Kim KS, Moon YJ, Huh IY, Lee J, et al. Rupture risk of intracranial aneurysm and prediction of hemorrhagic stroke after liver transplant. Brain Sci. 2021; 11(4):445. PMID: 33807191.26. Targher G, Bertolini L, Scala L, Zoppini G, Zenari L, Falezza G. Non-alcoholic hepatic steatosis and its relation to increased plasma biomarkers of inflammation and endothelial dysfunction in non-diabetic men. Role of visceral adipose tissue. Diabet Med. 2005; 22(10):1354–1358. PMID: 16176196.27. Raevens S, Coulon S, Van Steenkiste C, Colman R, Verhelst X, Van Vlierberghe H, et al. Role of angiogenic factors/cell adhesion markers in serum of cirrhotic patients with hepatopulmonary syndrome. Liver Int. 2015; 35(5):1499–1507. PMID: 24766195.28. Kim T, Kwon OK, Bang JS, Lee H, Kim JE, Kang HS, et al. Epidemiology of ruptured brain arteriovenous malformation: a national cohort study in Korea. J Neurosurg. 2018; 130:1965–1970.29. Gondar R, El Rahal A, Kulcsár Z, Schaller K, Momjian S. Spontaneous appearance of de novo intracranial arteriovenous malformation in hepatic cirrhosis. Neurochirurgie. 2019; 65(6):393–396. PMID: 31605684.30. Shimoda Y, Kuroda S, Kashiwazaki D, Asano T, Yamashita K, Taniguchi M, et al. Spontaneous disappearance of intracranial arteriovenous malformation after living-donor liver transplantation: a case report. No Shinkei Geka. 2011; 39(6):589–594. PMID: 21628738.31. Kim YD, Song D, Heo JH, Kim SU, Kim BK, Park JY, et al. Relationship between cerebral microbleeds and liver stiffness determined by transient elastography. PLoS One. 2015; 10(9):e0139227. PMID: 26421848.32. Kang Y, Elia E. Anesthesia management of liver transplantation. Doria C, editor. Contemporary Liver Transplantation. Cham, Switzerland: Springer Nature;2017. p. 143–187.33. Kim YW, Neal D, Hoh BL. Cerebral aneurysms in pregnancy and delivery: pregnancy and delivery do not increase the risk of aneurysm rupture. Neurosurgery. 2013; 72(2):143–149. PMID: 23147786.34. Salonen Ros H, Lichtenstein P, Bellocco R, Petersson G, Cnattingius S. Increased risks of circulatory diseases in late pregnancy and puerperium. Epidemiology. 2001; 12(4):456–460. PMID: 11416782.35. Zhang Y, Li L, Jia L, Chong W, Hai Y, Lunsford LD, et al. Association of chronic liver disease and mortality in patients with aneurysmal subarachnoid hemorrhage. Stroke. 2021; 52(10):e614–e617. PMID: 34281381.36. Lagman C, Nagasawa DT, Sheppard JP, Jacky Chen CH, Nguyen T, Prashant GN, et al. End-stage liver disease in patients with intracranial hemorrhage is associated with increased mortality: a cohort study. World Neurosurg. 2018; 113:e320–e327. PMID: 29452322.37. Prelipcean CC, Fierbinteanu-Braticevici C, Drug VL, Lăcătuşu C, Mihai B, Mihai C. Liver cirrhosis--procoagulant stasis. Rev Med Chir Soc Med Nat Iasi. 2011; 115(3):678–685. PMID: 22046771.38. Strauss GI, Hansen BA, Herzog T, Larsen FS. Cerebral autoregulation in patients with end-stage liver disease. Eur J Gastroenterol Hepatol. 2000; 12(7):767–771. PMID: 10929904.39. Djiambou-Nganjeu H. Hepatic encephalopathy in liver cirrhosis. J Transl Int Med. 2017; 5(1):64–67. PMID: 28680841.40. Koch DG, Speiser JL, Durkalski V, Fontana RJ, Davern T, McGuire B, et al. The natural history of severe acute liver injury. Am J Gastroenterol. 2017; 112(9):1389–1396. PMID: 28440304.41. Pan C, Xu LJ, Zhou R, Zhou W, Huang JR. Multivariate analysis of hepatic encephalopathy occurrence in patients with liver failure. Chung Hua Kan Tsang Ping Tsa Chih. 2012; 20(6):434–437. PMID: 23044200.42. Kamath PS, Wiesner RH, Malinchoc M, Kremers W, Therneau TM, Kosberg CL, et al. A model to predict survival in patients with end-stage liver disease. Hepatology. 2001; 33(2):464–470. PMID: 11172350.43. Shalimar , Sheikh MF, Mookerjee RP, Agarwal B, Acharya SK, Jalan R. Prognostic role of ammonia in patients with cirrhosis. Hepatology. 2019; 70(3):982–994. PMID: 30703853.44. Back A, Tupper KY, Bai T, Chiranand P, Goldenberg FD, Frank JI, et al. Ammonia-induced brain swelling and neurotoxicity in an organotypic slice model. Neurol Res. 2011; 33(10):1100–1108. PMID: 22196764.45. Byoun HS, Huh W, Oh CW, Bang JS, Hwang G, Kwon OK. Natural history of unruptured intracranial aneurysms: a retrospective single center analysis. J Korean Neurosurg Soc. 2016; 59(1):11–16. PMID: 26885281.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ruptured Intracranial Dermoid Cyst Associated with Rupture of Cerebral Aneurysm
- Simultaneous Onset of Ischemic and Hemorrhagic Stroke Due To Intracranial Artery Dissection
- Traumatic Rupture of Middle Cerebral Artery Aneurysm
- A new risk-scoring model for predicting 30-day mortality after repair of abdominal aortic aneurysms in the era of endovascular procedures
- New Pathophysiological Considerations on Cerebral Aneurysms