J Korean Med Sci.
2024 Feb;39(6):e60. 10.3346/jkms.2024.39.e60.
Effects of Transport to Trauma Centers on Survival Outcomes Among Severe Trauma Patients in Korea: Nationwide Age-Stratified Analysis
- Affiliations
-
- 1Department of Emergency Medicine, Seoul National University College of Medicine, Seoul, Korea
- 2Department of Emergency Medicine, Seoul National University Hospital, Seoul, Korea
- 3Department of Emergency Medicine, Seoul Metropolitan Government-Seoul National University Hospital Boramae Medical Center, Seoul, Korea
- 4Laboratory of Emergency Medical Services, Seoul National University Hospital Biomedical Research Institute, Seoul, Korea
- KMID: 2553307
- DOI: http://doi.org/10.3346/jkms.2024.39.e60
Abstract
- Background
Previous studies showed that the prognosis for severe trauma patients is better after transport to trauma centers compared to non-trauma centers. However, the benefit from transport to trauma centers may differ according to age group. The aim of this study was to compare the effects of transport to trauma centers on survival outcomes in different age groups among severe trauma patients in Korea.
Methods
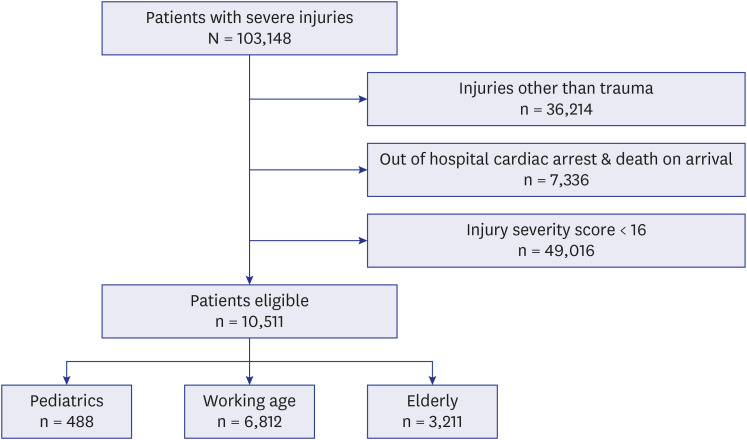
Cross-sectional study using Korean national emergency medical service (EMS) based severe trauma registry in 2018–2019 was conducted. EMS-treated trauma patients whose injury severity score was above or equal to 16, and who were not out-of-hospital cardiac arrest or death on arrival were included. Patients were classified into 3 groups: pediatrics (age < 19), working age (age 19–65), and elderly (age > 65). The primary outcome was in-hospital mortality. Multivariable logistic regression analysis was conducted to evaluate the effect of trauma center transport on outcome after adjusting of age, sex, comorbidity, mechanism of injury, Revised Trauma Score, and Injury Severity Score. All analysis was stratified according to the age group, and subgroup analysis for traumatic brain injury was also conducted.
Results
Overall, total of 10,511 patients were included in the study, and the number of patients in each age group were 488 in pediatrics, 6,812 in working age, and 3,211 in elderly, respectively. The adjusted odds ratio (95% confidence interval [CI]) of trauma center transport on in-hospital mortality from were 0.76 (95% CI, 0.43–1.32) in pediatrics, 0.78 (95% CI, 0.68–0.90) in working age, 0.71(95% CI, 0.60–0.85) in elderly, respectively. In subgroup analysis of traumatic brain injury, the benefit from trauma center transport was observed only in elderly group.
Conclusion
We found out trauma centers showed better clinical outcomes for adult and elderly groups, excluding the pediatric group than non-trauma centers. Further research is warranted to evaluate and develop the response system for pediatric severe trauma patients in Korea.
Keyword
Figure
Reference
-
1. Rossiter ND. “Trauma-the forgotten pandemic?”. Int Orthop. 2022; 46(1):3–11. PMID: 34519840.2. Minei JP, Schmicker RH, Kerby JD, Stiell IG, Schreiber MA, Bulger E, et al. Severe traumatic injury: regional variation in incidence and outcome. Ann Surg. 2010; 252(1):149–157. PMID: 20531005.3. MacKenzie EJ, Weir S, Rivara FP, Jurkovich GJ, Nathens AB, Wang W, et al. The value of trauma center care. J Trauma. 2010; 69(1):1–10. PMID: 20622572.4. MacKenzie EJ, Rivara FP, Jurkovich GJ, Nathens AB, Frey KP, Egleston BL, et al. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006; 354(4):366–378. PMID: 16436768.5. Nathens AB, Jurkovich GJ, Maier RV, Grossman DC, MacKenzie EJ, Moore M, et al. Relationship between trauma center volume and outcomes. JAMA. 2001; 285(9):1164–1171. PMID: 11231745.6. DuBose JJ, Browder T, Inaba K, Teixeira PG, Chan LS, Demetriades D. Effect of trauma center designation on outcome in patients with severe traumatic brain injury. Arch Surg. 2008; 143(12):1213–1217. PMID: 19075174.7. Gabbe BJ, Biostat GD, Lecky FE, Bouamra O, Woodford M, Jenks T, et al. The effect of an organized trauma system on mortality in major trauma involving serious head injury: a comparison of the United kingdom and Victoria, Australia. Ann Surg. 2011; 253(1):138–143. PMID: 21233612.8. Takahashi Y, Sato S, Yamashita K, Matsumoto N, Nozaki Y, Hirao T, et al. Effects of a trauma center on early mortality after trauma in a regional city in Japan: a population-based study. Trauma Surg Acute Care Open. 2019; 4(1):e000291. PMID: 31245618.9. George RL, McGwin G Jr, Windham ST, Melton SM, Metzger J, Chaudry IH, et al. Age-related gender differential in outcome after blunt or penetrating trauma. Shock. 2003; 19(1):28–32. PMID: 12558140.10. Harbrecht BG, Peitzman AB, Rivera L, Heil B, Croce M, Morris JA Jr, et al. Contribution of age and gender to outcome of blunt splenic injury in adults: multicenter study of the eastern association for the surgery of trauma. J Trauma. 2001; 51(5):887–895. PMID: 11706335.11. Wesson DE. Pediatric trauma centers: coming of age. Tex Heart Inst J. 2012; 39(6):871–873. PMID: 23304041.12. Webman RB, Carter EA, Mittal S, Wang J, Sathya C, Nathens AB, et al. Association between trauma center type and mortality among injured adolescent patients. JAMA Pediatr. 2016; 170(8):780–786. PMID: 27368110.13. Potoka DA, Schall LC, Gardner MJ, Stafford PW, Peitzman AB, Ford HR. Impact of pediatric trauma centers on mortality in a statewide system. J Trauma. 2000; 49(2):237–245. PMID: 10963534.14. Potoka DA, Schall LC, Ford HR. Improved functional outcome for severely injured children treated at pediatric trauma centers. J Trauma. 2001; 51(5):824–832. PMID: 11706326.15. Jarman MP, Jin G, Weissman JS, Ash AS, Tjia J, Salim A, et al. Association of trauma center designation with postdischarge survival among older adults with injuries. JAMA Netw Open. 2022; 5(3):e222448. PMID: 35294541.16. Bonne S, Schuerer DJ. Trauma in the older adult: epidemiology and evolving geriatric trauma principles. Clin Geriatr Med. 2013; 29(1):137–150. PMID: 23177604.17. Pracht EE, Tepas JJ 3rd, Langland-Orban B, Simpson L, Pieper P, Flint LM. Do pediatric patients with trauma in Florida have reduced mortality rates when treated in designated trauma centers? J Pediatr Surg. 2008; 43(1):212–221. PMID: 18206485.18. Pracht EE, Langland-Orban B, Flint L. Survival advantage for elderly trauma patients treated in a designated trauma center. J Trauma. 2011; 71(1):69–77. PMID: 21818016.19. Moore L, Turgeon AF, Sirois MJ, Lavoie A. Trauma centre outcome performance: a comparison of young adults and geriatric patients in an inclusive trauma system. Injury. 2012; 43(9):1580–1585. PMID: 21382620.20. Park DJ, Park CY, Cho HM, Lee KH, Han HS. Current status and future prospects of trauma centers in Korea. J Korean Med Assoc. 2017; 60(7):530–532.21. Choi KK, Jang MJ, Lee MA, Lee GJ, Yoo B, Park Y, et al. The suitability of the CdC field triage for Korean trauma care. J Trauma Inj. 2020; 33(1):13–17.22. Park JH, Song KJ, Shin SD, Hong KJ, Ro YS, Jeong J, et al. Epidemiology and outcomes of severe injury patients: nationwide community-based study in Korea. Injury. 2022; 53(6):1935–1946. PMID: 35369987.23. van Walraven C, Austin PC, Jennings A, Quan H, Forster AJ. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care. 2009; 47(6):626–633. PMID: 19433995.24. Thompson HJ, Dikmen S, Temkin N. Prevalence of comorbidity and its association with traumatic brain injury and outcomes in older adults. Res Gerontol Nurs. 2012; 5(1):17–24. PMID: 22165997.25. Menendez ME, Ring D. A comparison of the Charlson and Elixhauser comorbidity measures to predict inpatient mortality after proximal humerus fracture. J Orthop Trauma. 2015; 29(11):488–493. PMID: 26165266.26. Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998; 36(1):8–27. PMID: 9431328.27. Champion HR, Sacco WJ, Copes WS. Injury severity scoring again. J Trauma. 1995; 38(1):94–95. PMID: 7745669.28. Zaloshnja E, Miller T, Langlois JA, Selassie AW. Prevalence of long-term disability from traumatic brain injury in the civilian population of the United States, 2005. J Head Trauma Rehabil. 2008; 23(6):394–400. PMID: 19033832.29. Maas AI, Menon DK, Adelson PD, Andelic N, Bell MJ, Belli A, et al. Traumatic brain injury: integrated approaches to improve prevention, clinical care, and research. Lancet Neurol. 2017; 16(12):987–1048. PMID: 29122524.30. Jung K, Kwon J, Huh Y, Moon J, Hwang K, Cho HM, et al. National trauma system establishment based on implementation of regional trauma centers improves outcomes of trauma care: a follow-up observational study in South Korea. PLOS Glob Public Health. 2022; 2(1):e0000162. PMID: 36962235.31. Hwang K, Kwon J, Cho J, Heo Y, Lee JC, Jung K. Implementation of trauma center and massive transfusion protocol improves outcomes for major trauma patients: a study at a single institution in Korea. World J Surg. 2018; 42(7):2067–2075. PMID: 29290073.32. Kim JS, Jeong SW, Ahn HJ, Hwang HJ, Kyoung KH, Kwon SC, et al. Effects of trauma center establishment on the clinical characteristics and outcomes of patients with traumatic brain injury: a retrospective analysis from a single trauma center in Korea. J Korean Neurosurg Soc. 2019; 62(2):232–242. PMID: 30840979.33. Rhodes M, Smith S, Boorse D. Pediatric trauma patients in an ‘adult’ trauma center. J Trauma. 1993; 35(3):384–392. PMID: 8371296.34. Knudson MM, McGrath J. Improving outcomes in pediatric trauma care: essential characteristics of the trauma center. J Trauma. 2007; 63(6):Suppl. S140–S142. PMID: 18091206.35. James SL, Theadom A, Ellenbogen RG, Bannick MS, Montjoy-Venning W, Lucchesi LR, et al. Global, regional, and national burden of traumatic brain injury and spinal cord injury, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019; 18(1):56–87. PMID: 30497965.36. Park Y, Lee GJ, Lee MA, Choi KK, Gwak J, Hyun SY, et al. Major causes of preventable death in trauma patients. J Trauma Inj. 2021; 34(4):225–232.37. Kang MS, Kim HS. Characteristics and trends of traumatic injuries in children visiting emergency departments in South Korea: a retrospective serial cross-sectional study using both nationwide-sample and single-institutional data. PLoS One. 2019; 14(8):e0220798. PMID: 31398222.38. Giza CC, Mink RB, Madikians A. Pediatric traumatic brain injury: not just little adults. Curr Opin Crit Care. 2007; 13(2):143–152. PMID: 17327734.39. Kochanek PM, Tasker RC, Carney N, Totten AM, Adelson PD, Selden NR, et al. Guidelines for the management of pediatric severe traumatic brain injury: update of the brain trauma foundation guidelines, executive summary. Neurosurgery. 2019; 84(6):1169–1178. PMID: 30822776.40. Cosentino CM, Barthel MJ, Reynolds M. The impact of level 1 pediatric trauma center designation on demographics and financial reimbursement. J Pediatr Surg. 1991; 26(3):306–309. PMID: 2030476.41. Hunt EA, Heine M, Hohenhaus SM, Luo X, Frush KS. Simulated pediatric trauma team management: assessment of an educational intervention. Pediatr Emerg Care. 2007; 23(11):796–804. PMID: 18007210.42. Eichelberger MR, Gotschall CS, Sacco WJ, Bowman LM, Mangubat EA, Lowenstein AD. A comparison of the trauma score, the revised trauma score, and the pediatric trauma score. Ann Emerg Med. 1989; 18(10):1053–1058. PMID: 2802280.43. Bankole S, Asuncion A, Ross S, Aghai Z, Nollah L, Echols H, et al. First responder performance in pediatric trauma: a comparison with an adult cohort. Pediatr Crit Care Med. 2011; 12(4):e166–e170. PMID: 20729789.44. Keller MS, Vane DW. Management of pediatric blunt splenic injury: comparison of pediatric and adult trauma surgeons. J Pediatr Surg. 1995; 30(2):221–224. PMID: 7738742.45. Butler EK, Groner JI, Vavilala MS, Bulger EM, Rivara FP. Surgeon choice in management of pediatric abdominal trauma. J Pediatr Surg. 2021; 56(1):146–152. PMID: 33139031.46. Kwon J, Lee M, Moon J, Huh Y, Song S, Kim S, et al. National follow-up survey of preventable trauma death rate in Korea. J Korean Med Sci. 2022; 37(50):e349. PMID: 36573386.47. Kaya E, Ozguc H, Tokyay R, Yunuk O. Financial burden of trauma care on a university hospital in a developing country. J Trauma. 1999; 47(3):572–575. PMID: 10498318.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Proposal for stabilization of regional trauma centers in Korea
- Comparison of Outcomes at Trauma Centers versus Non-Trauma Centers for Severe Traumatic Brain Injury
- Reduced Mortality by Physician-Staffed HEMS Dispatch for Adult Blunt Trauma Patients in Korea
- Reduced Mortality in Severely Injured Patients Using Hospital-based Helicopter Emergency Medical Services in Interhospital Transport
- Survey of Recognition of Trauma and Trauma Care System