Child Kidney Dis.
2024 Feb;28(1):44-50. 10.3339/ckd.24.004.
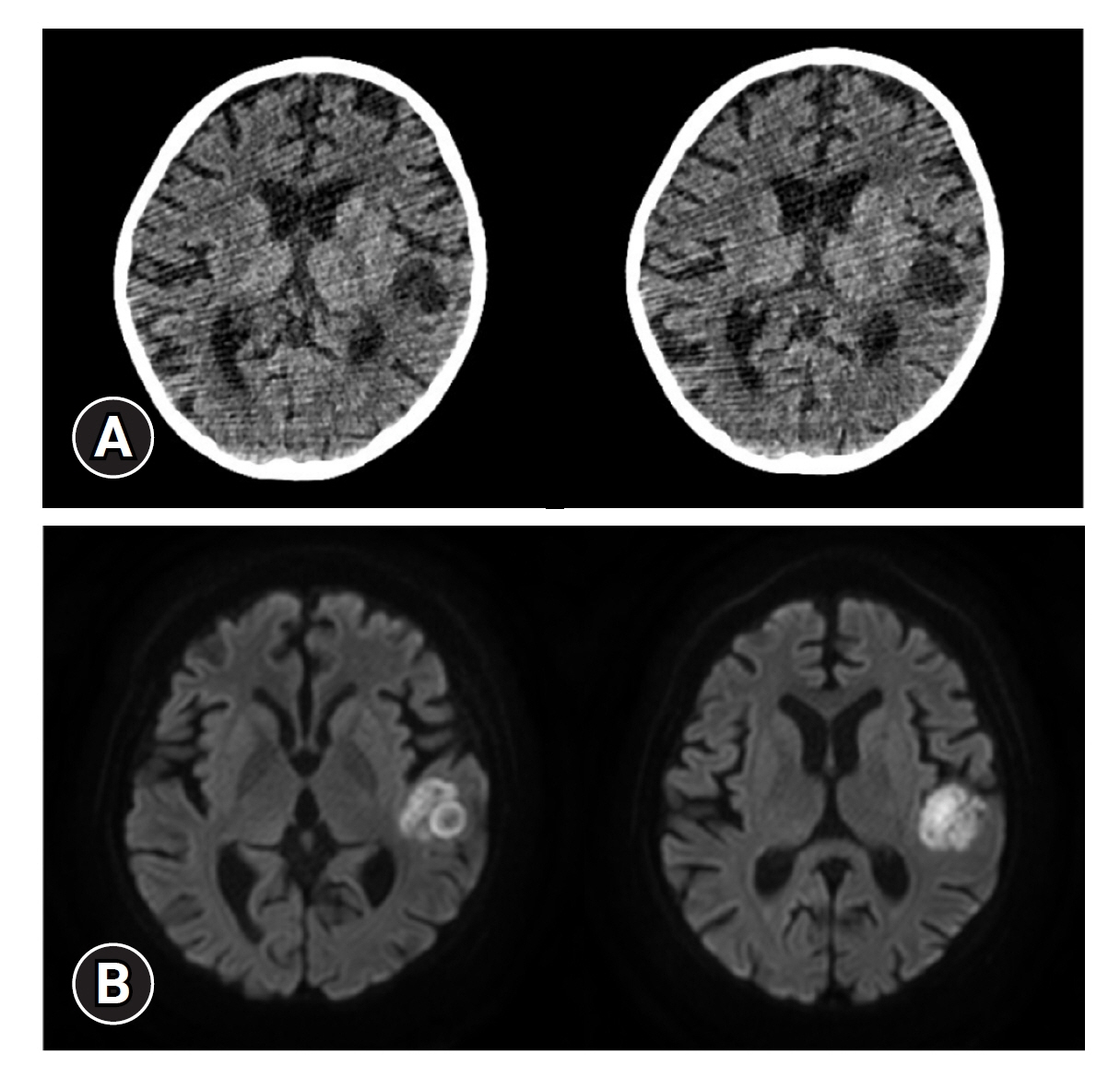
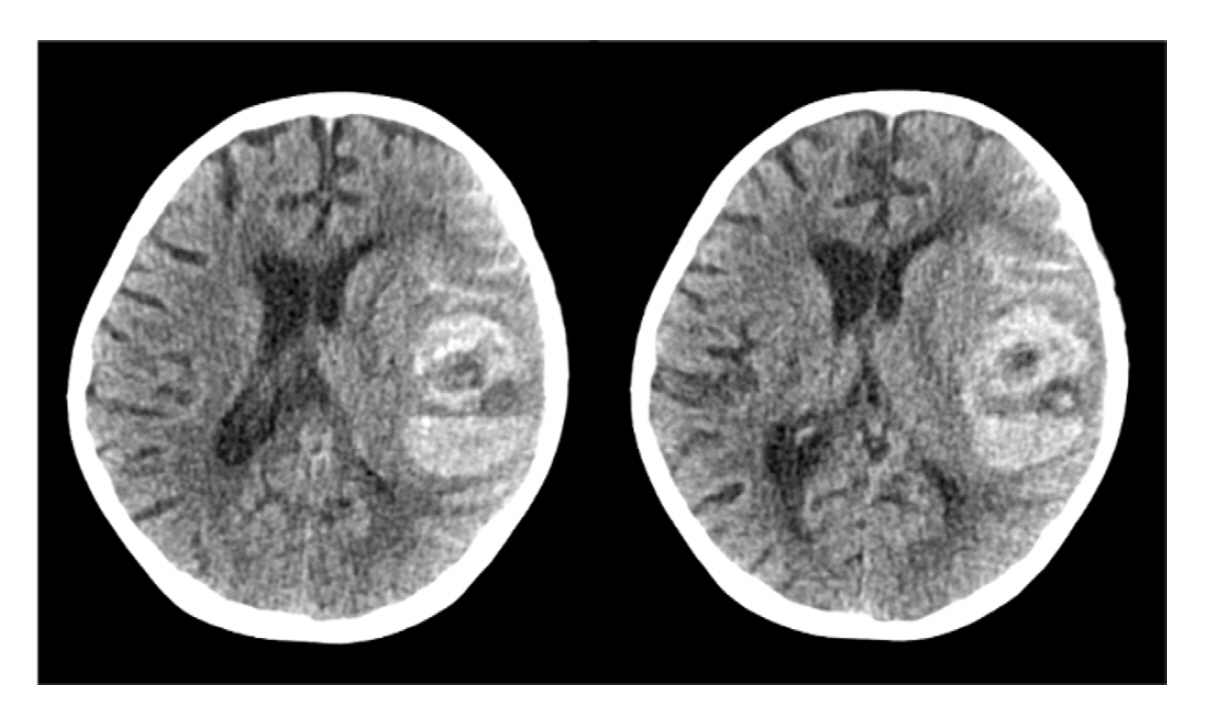
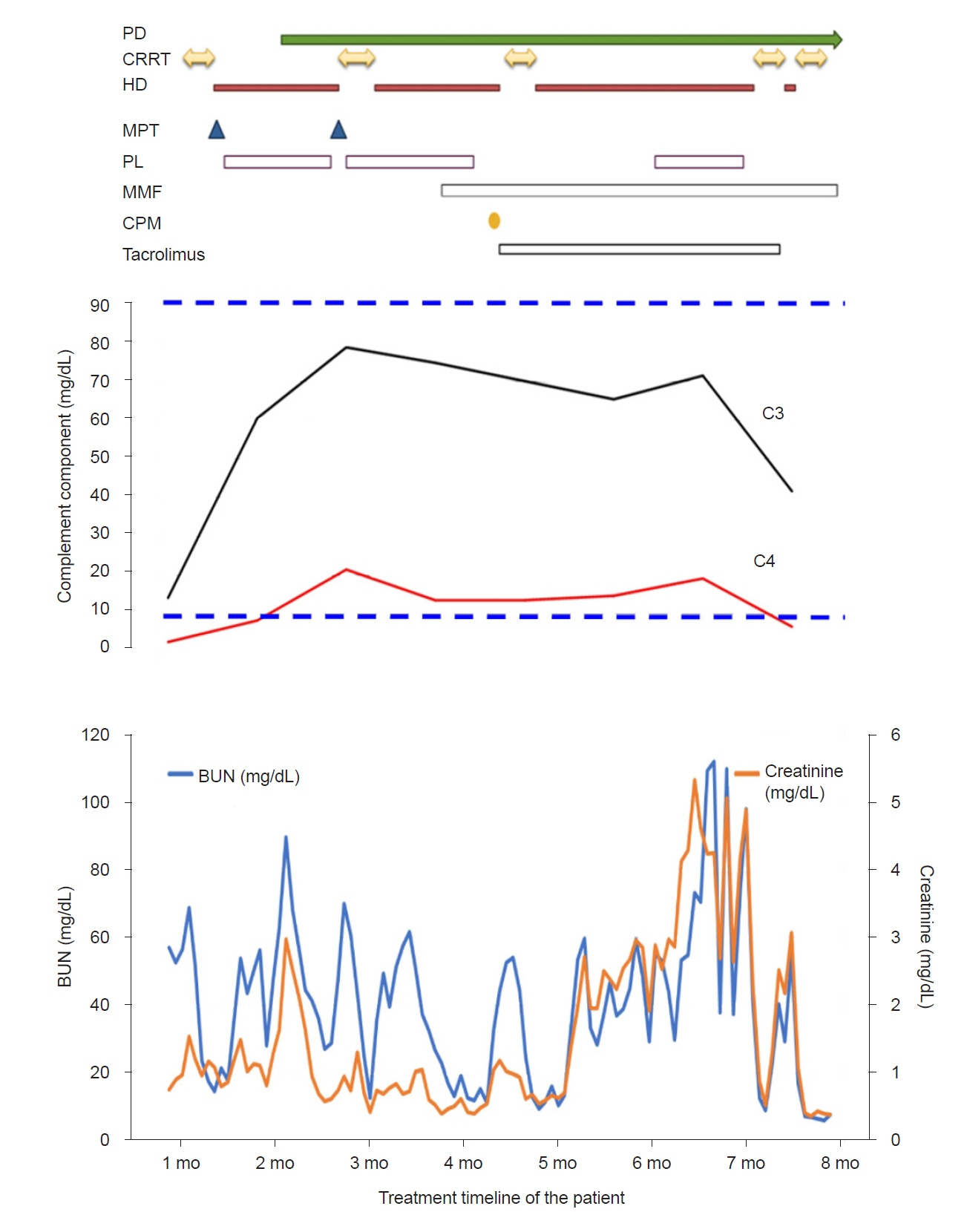
A rare case of childhood-onset systemic lupus erythematosus associated end-stage renal disease with cerebral abscess and hemorrhage
- Affiliations
-
- 1Department of Pediatrics, Yonsei University College of Medicine, Seoul, Republic of Korea
- 2Division of Pediatric Nephrology, Severance Children’s Hospital, Seoul, Republic of Korea
- 3Institute of Kidney Disease Research, Yonsei University College of Medicine, Seoul, Republic of Korea
- 4Department of Pediatrics, Gangnam Severance Hospital, Seoul, Republic of Korea
- KMID: 2553179
- DOI: http://doi.org/10.3339/ckd.24.004
Abstract
- Systemic lupus erythematosus (SLE) is a chronic autoimmune inflammatory disease that affects multiple organs. More than half of the patients with SLE have kidney involvement, and up to 10% of patients with lupus nephritis develop end-stage renal disease (ESRD). Central nervous system (CNS) involvement in SLE occurs in 21% to 95% of patients. Severe neurological manifestations such as seizures, cerebrovascular disease, meningitis, and cerebrovascular accidents can develop in childhood-onset SLE, but cerebral infections, such as brain abscess and hemorrhage, are seldom reported in lupus nephritis, even in adults. Here, we report a rare case of childhood-onset SLE with ESRD, a cerebral abscess, and hemorrhage. A 9-year-old girl diagnosed with lupus nephritis was administered high-dose steroids and immunosuppressant therapy to treat acute kidney injury (AKI) and massive proteinuria. The AKI deteriorated, and after 3 months, she developed ESRD. She received hemodialysis three times a week along with daily peritoneal dialysis to control edema. She developed seizures, and imaging showed a brain abscess. This was complicated by spontaneous cerebral hemorrhage, and she became unstable. She died shortly after the hemorrhage was discovered. In conclusion, CNS complications should always be considered in clinical practice because they increase mortality, especially in those with risk factors for infection.
Figure
Reference
-
References
1. Sinha R, Raut S. Pediatric lupus nephritis: management update. World J Nephrol. 2014; 3:16–23.
Article2. Fatemi A, Matinfar M, Smiley A. Childhood versus adult-onset systemic lupus erythematosus: long-term outcome and predictors of mortality. Clin Rheumatol. 2017; 36:343–50.
Article3. Ambrose N, Morgan TA, Galloway J, Ionnoau Y, Beresford MW, Isenberg DA, et al. Differences in disease phenotype and severity in SLE across age groups. Lupus. 2016; 25:1542–50.
Article4. Levy DM, Kamphuis S. Systemic lupus erythematosus in children and adolescents. Pediatr Clin North Am. 2012; 59:345–64.
Article5. Bertsias GK, Boumpas DT. Connective tissue diseases: Lupus nephritis-winning a few battles but not the war. Nat Rev Rheumatol. 2011; 7:441–2.
Article6. Hanly JG, McCurdy G, Fougere L, Douglas JA, Thompson K. Neuropsychiatric events in systemic lupus erythematosus: attribution and clinical significance. J Rheumatol. 2004; 31:2156–62.7. Manger K, Manger B, Repp R, Geisselbrecht M, Geiger A, Pfahlberg A, et al. Definition of risk factors for death, end stage renal disease, and thromboembolic events in a monocentric cohort of 338 patients with systemic lupus erythematosus. Ann Rheum Dis. 2002; 61:1065–70.
Article8. Kittivisuit S, Vachvanichsanong P, McNeil E, Chotsampancharoen T. Childhood-onset systemic lupus erythematosus and immune thrombocytopenia: prevalence and risk factors. Pediatr Blood Cancer. 2021; 68:e29146.
Article9. Bennett M, Brunner HI. Biomarkers and updates on pediatrics lupus nephritis. Rheum Dis Clin North Am. 2013; 39:833–53.
Article10. Pereira T, Abitbol CL, Seeherunvong W, Katsoufis C, Chandar J, Freundlich M, et al. Three decades of progress in treating childhood-onset lupus nephritis. Clin J Am Soc Nephrol. 2011; 6:2192–9.
Article11. Hiraki LT, Lu B, Alexander SR, Shaykevich T, Alarcon GS, Solomon DH, et al. End-stage renal disease due to lupus nephritis among children in the US, 1995-2006. Arthritis Rheum. 2011; 63:1988–97.
Article12. Hersh AO, von Scheven E, Yazdany J, Panopalis P, Trupin L, Julian L, et al. Differences in long-term disease activity and treatment of adult patients with childhood- and adult-onset systemic lupus erythematosus. Arthritis Rheum. 2009; 61:13–20.
Article13. Doria A, Arienti S, Rampudda M, Canova M, Tonon M, Sarzi-Puttini P. Preventive strategies in systemic lupus erythematosus. Autoimmun Rev. 2008; 7:192–7.
Article14. Poinen K, Quinn RR, Clarke A, Ravani P, Hiremath S, Miller LM, et al. Complications from tunneled hemodialysis catheters: a Canadian observational cohort study. Am J Kidney Dis. 2019; 73:467–75.
Article15. Abbasi SH, Aftab RA, Chua SS. Risk factors associated with nosocomial infections among end stage renal disease patients undergoing hemodialysis: a systematic review. PLoS One. 2020; 15:e0234376.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Ruptured Aneurysm in a Patient with Systemic Lupus Erythematosus: Case Report
- Pulmonary Hemorrhage with Hemoptysis in Systemic Lupus Erythematosis
- Lupus Erythematosus Profundus Associated with Kikuchi's Disease
- Childhood Systemic Lupus Erythematosus Misdiagnosed as Atopic Dermatitis
- A Case of Transverse Myelitis as a First Manifestation of Systemic Lupus Erythematosus