Ann Rehabil Med.
2024 Feb;48(1):31-41. 10.5535/arm.23086.
The Effectiveness of Goal-Oriented Dual Task Proprioceptive Training in Subacute Stroke: A Retrospective Observational Study
- Affiliations
-
- 1Department of Biomedical and Biotechnological Sciences, University of Catania, Catania, Italy
- 2Sant’Agata Rehabilitation Hospital, Catania, Italy
- 3Department of Pain Management, Policlinico-San Marco Hospital, Catania, Italy
- 4Sanitary direction, Policlinico Hospital, Catania, Italy
- 5Provincial health department of Siracusa, Sicily, Italy
- KMID: 2553159
- DOI: http://doi.org/10.5535/arm.23086
Abstract
Objective
To show the effectiveness of goal-oriented proprioceptive training in subacute stroke for balance, autonomy, and fall risk.
Methods
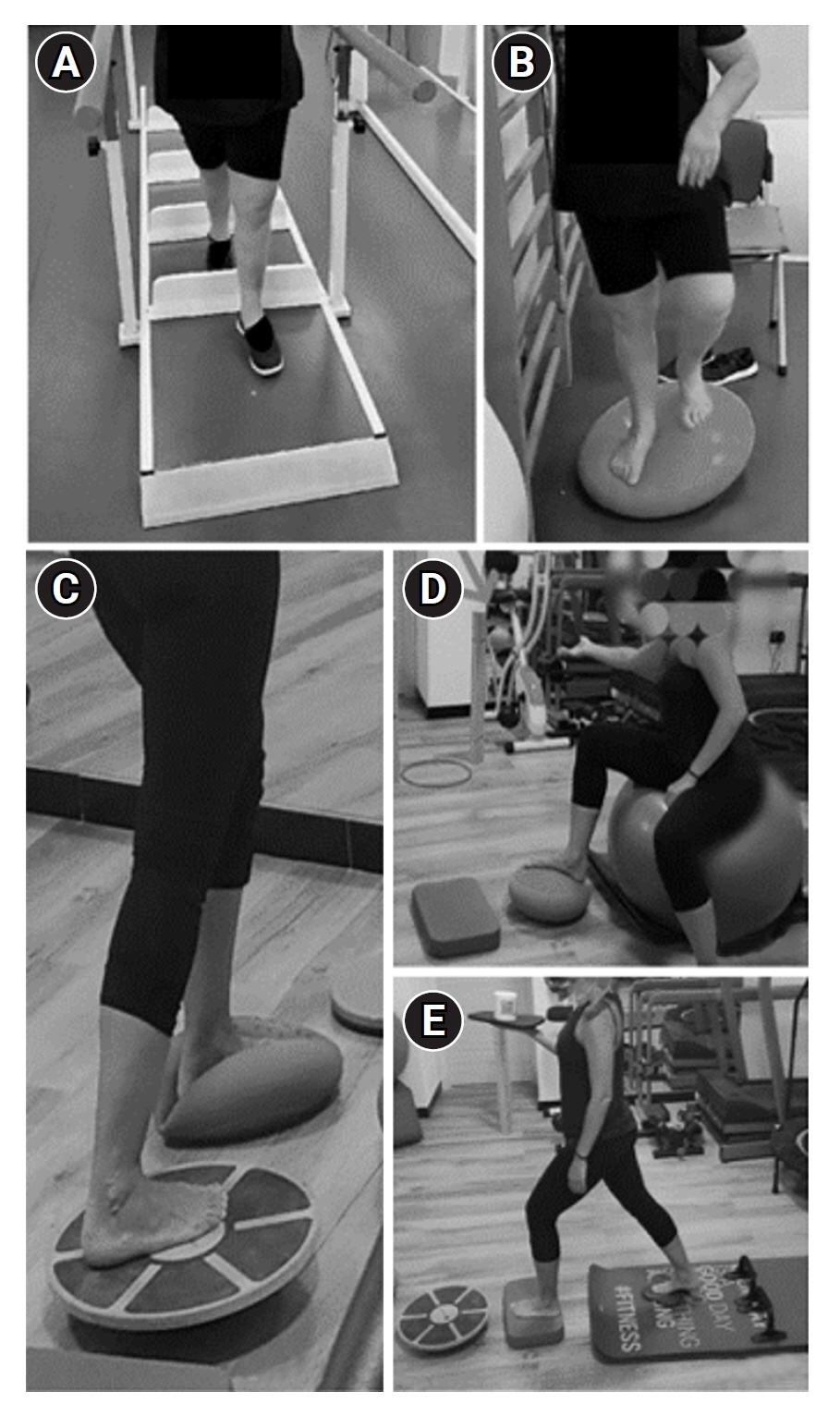
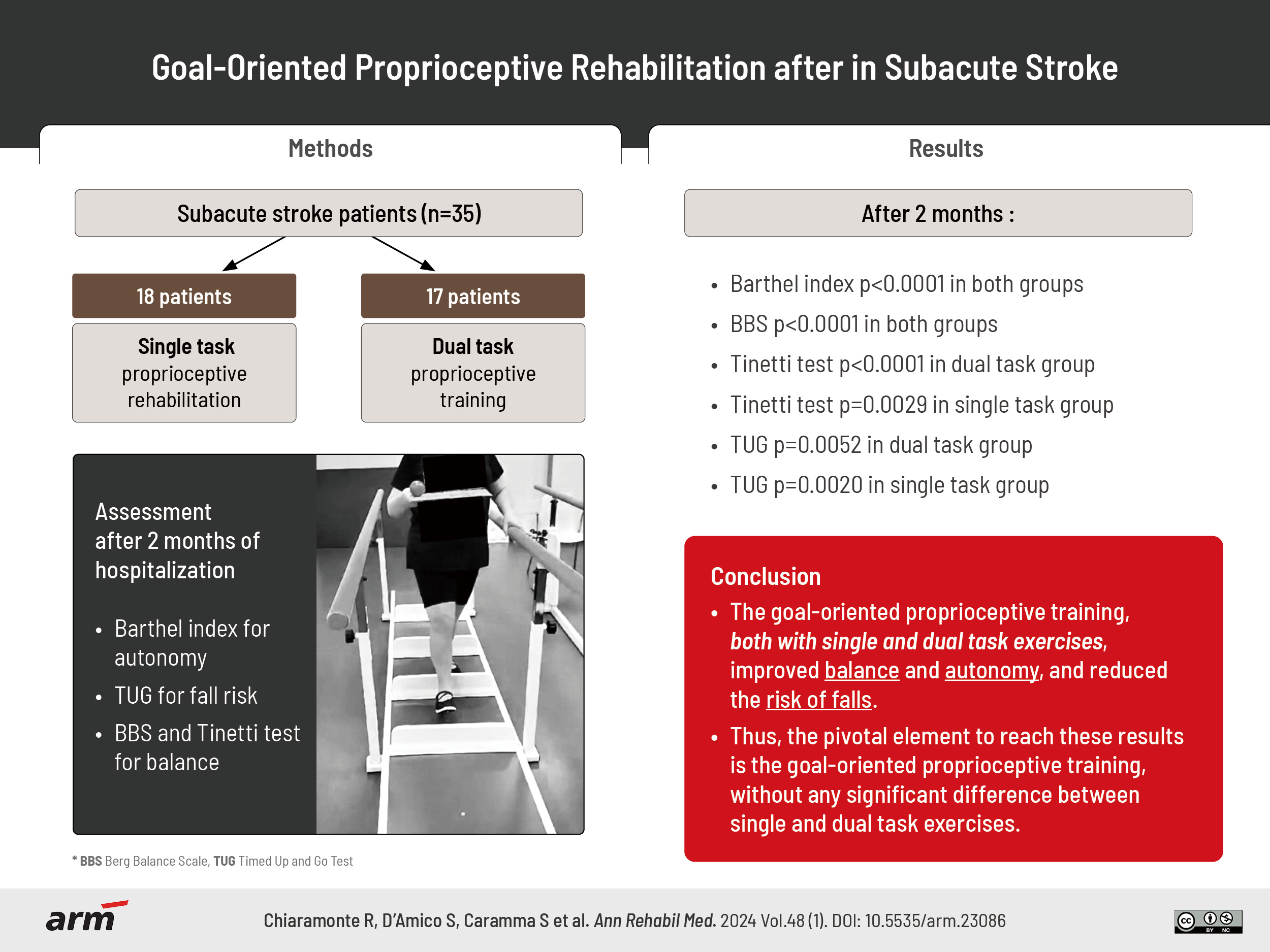
Out a total of 35 patients, consistent in age (75.31±8.65 years), type of stroke (ischemic, 3 to 11 weeks before), and motor impairment, 18 patients underwent solely proprioceptive rehabilitation, the other 17 dual task exercises. The study assessed autonomy using Barthel Index, fall risk with Timed Up and Go Test (TUG), balance through Berg Balance Scale (BBS) and Tinetti test.
Results
After two months, significant improvements were recorded in Barthel Index, BBS (p<0.0001), Tinetti test (p<0.0001 in dual task group, p=0.0029 in single task group), and TUG (p=0.0052 in dual task group, p=0.0020 in single task group) in both groups. Comparing the two groups, dual task group showed a significant difference in Tinetti balance assessment (p=0.0052), between the total score of Tinetti test and TUG in single (p=0.0271), and dual task (p=0.0235). Likewise, Tinetti gait test was significantly related to TUG in single (p=0.0536), and dual task (p=0.0466), while Tinetti balance test to Barthel Index (p=0.0394), BBS (p<0.0001), and TUG in single (p=0.0219), and dual task (p=0.0196). Lastly, there is a positive correlation of the use of aids with BBS (p=0.0074), and total score of Tinetti test (p=0.0160).
Conclusion
In subacute stroke, goal-oriented proprioceptive training improved balance, but only partially autonomy. Furthermore, the use of aids after dual-task exercises improved recovery of balance, but did not reduced falls.
Keyword
Figure
Reference
-
1. Donkor ES. Stroke in the 21st century: a snapshot of the burden, epidemiology, and quality of life. Stroke Res Treat. 2018; 2018:3238165.2. Kelly C, Meyer J, Hanks V, Barefield C. Neurorehabilitation for an individual with bilateral thalamic stroke and preexisting visual impairment presenting with impaired use of sensory cues: a case report. Physiother Theory Pract. 2021; 37:1139–45.3. Khan F, Chevidikunnan MF. Prevalence of balance impairment and factors associated with balance among patients with stroke. A cross sectional retrospective case control study. Healthcare (Basel). 2021; 9:320.4. Connell LA, Lincoln NB, Radford KA. Somatosensory impairment after stroke: frequency of different deficits and their recovery. Clin Rehabil. 2008; 22:758–67.5. Kim OJ. Development of neurophysiology in the early twentieth century: Charles Scott Sherrington and The Integrative action of the nervous system. Uisahak. 2001; 10:1–21.6. Riemann BL, Lephart SM. The sensorimotor system, part I: the physiologic basis of functional joint stability. J Athl Train. 2002; 37:71–9.7. Ribeiro F, Oliveira J. Aging effects on joint proprioception: the role of physical activity in proprioception preservation. Eur Rev Aging Phys Act. 2007; 4:71–6.8. Aman JE, Elangovan N, Yeh IL, Konczak J. The effectiveness of proprioceptive training for improving motor function: a systematic review. Front Hum Neurosci. 2015; 8:1075.9. Ferlinc A, Fabiani E, Velnar T, Gradisnik L. The importance and role of proprioception in the elderly: a short review. Mater Sociomed. 2019; 31:219–21.10. Han J, Waddington G, Adams R, Anson J, Liu Y. Assessing proprioception: a critical review of methods. J Sport Health Sci. 2016; 5:80–90.11. Kaner MT, Hon E, He T, Patira R, Altschuler EL. Rehabilitation after complete hemisensory loss: report of two cases. Am J Phys Med Rehabil. 2020; 99:86–90.12. Gorst T, Rogers A, Morrison SC, Cramp M, Paton J, Freeman J, et al. The prevalence, distribution, and functional importance of lower limb somatosensory impairments in chronic stroke survivors: a cross sectional observational study. Disabil Rehabil. 2019; 41:2443–50.13. Rand D. Proprioception deficits in chronic stroke- upper extremity function and daily living. PLoS One. 2018; 13:e0195043.14. Persson CU, Hansson PO. Determinants of falls after stroke based on data on 5065 patients from the Swedish Väststroke and Riksstroke Registers. Sci Rep. 2021; 11:24035.15. Kim H, Kim HK, Kim N, Nam CS. Dual task effects on speed and accuracy during cognitive and upper limb motor tasks in adults with stroke hemiparesis. Front Hum Neurosci. 2021; 15:671541.16. Campos-Magdaleno M, Pereiro A, Navarro-Pardo E, Juncos-Rabadán O, Facal D. Dual-task performance in old adults: cognitive, functional, psychosocial and socio-demographic variables. Aging Clin Exp Res. 2022; 34:827–35.17. Tsang CSL, Pang MYC. Association of subsequent falls with evidence of dual-task interference while walking in community-dwelling individuals after stroke. Clin Rehabil. 2020; 34:971–80.18. Zhang X, Xu F, Shi H, Liu R, Wan X. Effects of dual-task training on gait and balance in stroke patients: a meta-analysis. Clin Rehabil. 2022; 36:1186–98.19. Mansfield A, Wong JS, McIlroy WE, Biasin L, Brunton K, Bayley M, et al. Do measures of reactive balance control predict falls in people with stroke returning to the community? Physiotherapy. 2015; 101:373–80.20. Chiaramonte R, Bonfiglio M, Leonforte P, Coltraro GL, Guerrera CS, Vecchio M. Proprioceptive and dual-task training: the key of stroke rehabilitation, a systematic review. J Funct Morphol Kinesiol. 2022; 7:53.21. Chiaramonte R, Bonfiglio M, Chisari S. Multidisciplinary protocol for the management of fibromyalgia associated with imbalance. Our experience and literature review. Rev Assoc Med Bras (1992). 2019; 65:1265–74.22. Jensen MP, Turner JA, Romano JM. What is the maximum number of levels needed in pain intensity measurement? Pain. 1994; 58:387–92.23. Castiglia SF, Galeoto G, Lauta A, Palumbo A, Tirinelli F, Viselli F, et al. The culturally adapted Italian version of the Barthel Index (IcaBI): assessment of structural validity, inter-rater reliability and responsiveness to clinically relevant improvements in patients admitted to inpatient rehabilitation centers. Funct Neurol. 2017; 22:221–8.24. Tinetti ME, Richman D, Powell L. Falls efficacy as a measure of fear of falling. J Gerontol. 1990; 45:P239–43.25. Ottonello M, Ferriero G, Benevolo E, Sessarego P, Dughi D. Psychometric evaluation of the Italian version of the Berg Balance Scale in rehabilitation inpatients. Eur Medicophys. 2003; 39:181–9.26. Ferraresi G, Buganè F, Cosma M, Agarici M, Vio A, Manca M, et al. Timed up and go test (tug) temporal phases assessment using a wireless device (free4act®): method validation in healthy subjects. Gait Posture. 2013; 37(Suppl 1):30–1.27. Hillig T, Ma H, Dorsch S. Goal-oriented instructions increase the intensity of practice in stroke rehabilitation compared with non-specific instructions: a within-participant, repeated measures experimental study. J Physiother. 2019; 65:95–8.28. Winter L, Huang Q, Sertic JVL, Konczak J. The effectiveness of proprioceptive training for improving motor performance and motor dysfunction: a systematic review. Front Rehabil Sci. 2022; 3:830166.29. Silsupadol P, Shumway-Cook A, Lugade V, van Donkelaar P, Chou LS, Mayr U, et al. Effects of single-task versus dual-task training on balance performance in older adults: a double-blind, randomized controlled trial. Arch Phys Med Rehabil. 2009; 90:381–7.30. Vecchio M, Gracies JM, Panza F, Fortunato F, Vitaliti G, Malaguarnera G, et al. Change in coefficient of fatigability following rapid, repetitive movement training in post-stroke spastic paresis: a prospective open-label observational study. J Stroke Cerebrovasc Dis. 2017; 26:2536–40.31. Apriliyasari RW, Van Truong P, Tsai PS. Effects of proprioceptive training for people with stroke: a meta-analysis of randomized controlled trials. Clin Rehabil. 2022; 36:431–48.32. Chae SH, Kim YL, Lee SM. Effects of phase proprioceptive training on balance in patients with chronic stroke. J Phys Ther Sci. 2017; 29:839–44.33. Varela-Vásquez LA, Minobes-Molina E, Jerez-Roig J. Dual-task exercises in older adults: a structured review of current literature. J Frailty Sarcopenia Falls. 2020; 5:31–7.34. Chiaramonte R, Cioni M. Critical spatiotemporal gait parameters for individuals with dementia: a systematic review and meta-analysis. Hong Kong Physiother J. 2021; 41:1–14.35. De Freitas TB, Leite PHW, Doná F, Pompeu JE, Swarowsky A, Torriani-Pasin C. The effects of dual task gait and balance training in Parkinson’s disease: a systematic review. Physiother Theory Pract. 2020; 36:1088–96.36. Morelli N, Morelli H. Dual task training effects on gait and balance outcomes in multiple sclerosis: a systematic review. Mult Scler Relat Disord. 2021; 49:102794.37. Baek CY, Chang WN, Park BY, Lee KB, Kang KY, Choi MR. Effects of dual-task gait treadmill training on gait ability, dual-task interference, and fall efficacy in people with stroke: a randomized controlled trial. Phys Ther 2021;101:pzab067. Erratum in: Phys Ther. 2022; 102:pzab184.38. Hong SY, Moon Y, Choi JD. Effects of cognitive task training on dynamic balance and gait of patients with stroke: a preliminary randomized controlled study. Med Sci Monit Basic Res. 2020; 26:e925264.39. Kannan L, Vora J, Bhatt T, Hughes SL. Cognitive-motor exergaming for reducing fall risk in people with chronic stroke: a randomized controlled trial. NeuroRehabilitation. 2019; 44:493–510.40. Spanò B, De Tollis M, Taglieri S, Manzo A, Ricci C, Lombardi MG, et al. The effect of dual-task motor-cognitive training in adults with neurological diseases who are at risk of falling. Brain Sci. 2022; 12:1207.41. Kim KH, Jang SH. Effects of task-specific training after cognitive sensorimotor exercise on proprioception, spasticity, and gait speed in stroke patients: a randomized controlled study. Medicina (Kaunas). 2021; 57:1098.42. Anandan D, Tamil Nidhi PK, Arun B, Vishnu P. Effect of task specific training with proprioceptive neuromuscular facilitation on stroke survivors. Biomedicine. 2020; 40:363–6.43. Saleh MSM, Rehab NI, Aly SMA. Effect of aquatic versus land motor dual task training on balance and gait of patients with chronic stroke: a randomized controlled trial. NeuroRehabilitation. 2019; 44:485–92.44. Hackney ME, Hall CD, Echt KV, Wolf SL. Application of adapted tango as therapeutic intervention for patients with chronic stroke. J Geriatr Phys Ther. 2012; 35:206–17.45. Traxler K, Baum E, Klotz E, Reindl M, Schinabeck F, Seebacher B. Combining specific task-oriented training with manual therapy to improve balance and mobility in patients after stroke: a mixed methods pilot randomised controlled trial. Disabil Rehabil. 2023; doi: 10.1080/09638288.2023.2193432. [Epub ahead of print].46. Fishbein P, Hutzler Y, Ratmansky M, Treger I, Dunsky A. A preliminary study of dual-task training using virtual reality: influence on walking and balance in chronic poststroke survivors. J Stroke Cerebrovasc Dis. 2019; 28:104343.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect of Dual-Task Training on Balance and Cognition in Patients With Subacute Post-Stroke
- Dual Task Training Effects on Upper Extremity Functions and Performance of Daily Activities of Chronic Stroke Patients
- Effects of activities of daily living-based dual-task training on upper extremity function, cognitive function, and quality of life in stroke patients
- The Effects of Task-Oriented Exercise Program on Balance Ability in Patients with Acute Stroke
- The Effects of Horse-riding Simulator Training with Dual-task on Pulmonary Function and Flexibility in Healthy Adults