Ann Surg Treat Res.
2024 Feb;106(2):78-84. 10.4174/astr.2024.106.2.78.
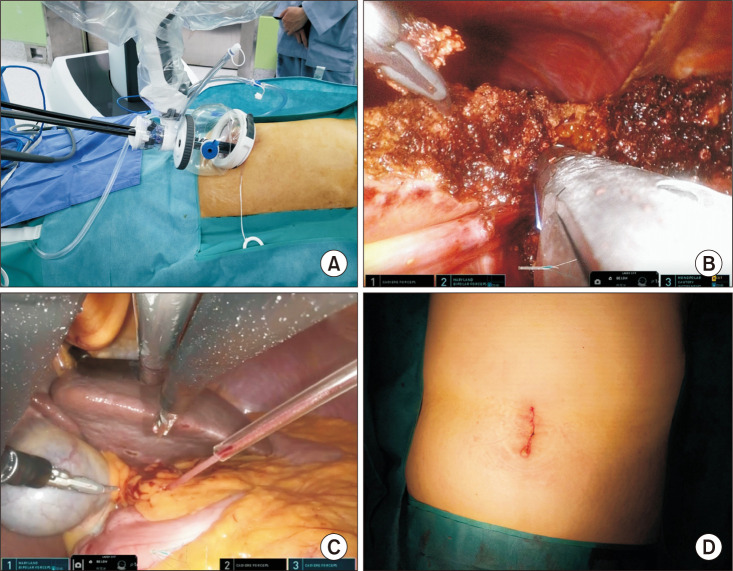
Early outcomes of single-port robotic left lateral sectionectomy in patients with hepatic tumor
- Affiliations
-
- 1Division of Pediatric Surgery, Department of Surgery, Korea University Guro Hospital, Korea University Medical College, Seoul, Korea
- 2Division of Hepatobiliary Pancreas Surgery, Department of Surgery, Korea University Guro Hospital, Korea University Medical College, Seoul, Korea
- KMID: 2552388
- DOI: http://doi.org/10.4174/astr.2024.106.2.78
Abstract
- Purpose
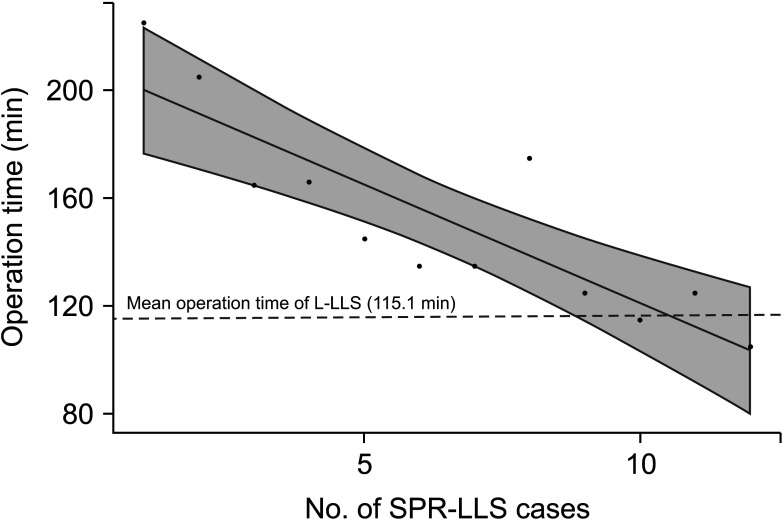
Laparoscopic left lateral sectionectomy (L-LLS) stands as a cornerstone procedure in hepatobiliary minimal surgery, frequently employed for various benign and malignant liver lesions. This study aimed to analyze the peri- and postoperative surgical outcomes of single-port robotic left lateral sectionectomy (SPR-LLS) vs. those of L-LLS in patients with hepatic tumors.
Methods
From January 2020 through June 2023, 12 patients underwent SPR-LLS. During the same period, 30 L-LLS procedures were performed. In total, 12 patients in the robotic group and 24 patients in the laparoscopic group were matched.
Results
When the SPR-LLS and L-LLS groups were compared, the operation time was longer in the SPR-LLS group with less blood loss and shorter hospital stay. Postoperative complications were observed in 3 patients in the L-LLS group (12.5%) and 1 patient in the SPR-LLS group (8.3%).
Conclusion
SPR-LLS using the da Vinci SP system was comparable to laparoscopic LLS in terms of surgical outcomes. SPR-LLS was associated with lower blood loss and less postoperative length of stay compared to L-LLS. These findings suggest that left lateral sectionectomy is technically feasible and safe with the da Vinci SP system in select patients.
Keyword
Figure
Reference
-
1. Ocuin LM, Tsung A. Robotic liver resection for malignancy: current status, oncologic outcomes, comparison to laparoscopy, and future applications. J Surg Oncol. 2015; 112:295–301. PMID: 26119652.2. Qiu J, Chen S, Chengyou D. A systematic review of robotic-assisted liver resection and meta-analysis of robotic versus laparoscopic hepatectomy for hepatic neoplasms. Surg Endosc. 2016; 30:862–875. PMID: 26092026.3. Bang YJ, Jun JH, Gwak MS, Ko JS, Kim JM, Choi GS, et al. Postoperative outcomes of purely laparoscopic donor hepatectomy compared to open living donor hepatectomy: a preliminary observational study. Ann Surg Treat Res. 2021; 100:235–245. PMID: 33854993.4. Kim JM, Rhu J, Ha SY, Choi GS, Kwon CHD, Kim G, et al. Realization of improved outcomes following liver resection in hepatocellular carcinoma patients aged 75 years and older. Ann Surg Treat Res. 2021; 101:257–265. PMID: 34796141.5. Tsung A, Geller DA, Sukato DC, Sabbaghian S, Tohme S, Steel J, et al. Robotic versus laparoscopic hepatectomy: a matched comparison. Ann Surg. 2014; 259:549–555. PMID: 24045442.6. Fagenson AM, Gleeson EM, Pitt HA, Lau KN. Minimally invasive hepatectomy in North America: laparoscopic versus robotic. J Gastrointest Surg. 2021; 25:85–93. PMID: 32583323.7. Ciria R, Berardi G, Alconchel F, Briceño J, Choi GH, Wu YM, et al. The impact of robotics in liver surgery: a worldwide systematic review and short-term outcomes meta-analysis on 2,728 cases. J Hepatobiliary Pancreat Sci. 2022; 29:181–197. PMID: 33200536.8. Hu M, Liu Y, Li C, Wang G, Yin Z, Lau WY, et al. Robotic versus laparoscopic liver resection in complex cases of left lateral sectionectomy. Int J Surg. 2019; 67:54–60. PMID: 31121328.9. Soubrane O, Cherqui D, Scatton O, Stenard F, Bernard D, Branchereau S, et al. Laparoscopic left lateral sectionectomy in living donors: safety and reproducibility of the technique in a single center. Ann Surg. 2006; 244:815–820. PMID: 17060776.10. Salloum C, Lim C, Lahat E, Gavara CG, Levesque E, Compagnon P, et al. Robotic-assisted versus laparoscopic left lateral sectionectomy: analysis of surgical outcomes and costs by a propensity score matched cohort study. World J Surg. 2017; 41:516–524. PMID: 27743071.11. Kim JK, Park JS, Han DH, Choi GH, Kim KS, Choi JS, et al. Robotic versus laparoscopic left lateral sectionectomy of liver. Surg Endosc. 2016; 30:4756–4764. PMID: 26902613.12. Kim WJ, Park PJ, Choi SB, Kim WB. Case report of pure single-port robotic left lateral sectionectomy using the da Vinci SP system. Medicine (Baltimore). 2021; 100:e28248. PMID: 34941098.13. Goh BK, Lee SY, Koh YX, Kam JH, Chan CY. Minimally invasive major hepatectomies: a Southeast Asian single institution contemporary experience with its first 120 consecutive cases. ANZ J Surg. 2020; 90:553–557. PMID: 31721400.14. Goh BK, Lee SY, Teo JY, Kam JH, Jeyaraj PR, Cheow PC, et al. Changing trends and outcomes associated with the adoption of minimally invasive hepatectomy: a contemporary single-institution experience with 400 consecutive resections. Surg Endosc. 2018; 32:4658–4665. PMID: 29967997.15. Gravetz A, Sucandy I, Wilfong C, Patel N, Spence J, Ross S, et al. Single-institution early experience and learning curve with robotic liver resections. Am Surg. 2019; 85:115–119. PMID: 30760356.16. Goh BK, Chan CY, Lee SY, Chung AY. Early experience with totally laparoscopic major hepatectomies: single institution experience with 31 consecutive cases. ANZ J Surg. 2018; 88:E329–E333. PMID: 28470679.17. Dalsgaard T, Jensen MD, Hartwell D, Mosgaard BJ, Jørgensen A, Jensen BR. Robotic surgery is less physically demanding than laparoscopic surgery: paired cross sectional study. Ann Surg. 2020; 271:106–113. PMID: 29923873.18. Azagra JS, Goergen M, Brondello S, Calmes MO, Philippe P, Schmitz B. Laparoscopic liver sectionectomy 2 and 3 (LLS 2 and 3): towards the “gold standard”. J Hepatobiliary Pancreat Surg. 2009; 16:422–426. PMID: 19466378.19. Chong CC, Lok HT, Fung AK, Fong AK, Cheung YS, Wong J, et al. Robotic versus laparoscopic hepatectomy: application of the difficulty scoring system. Surg Endosc. 2020; 34:2000–2006. PMID: 31312961.20. Ji WB, Wang HG, Zhao ZM, Duan WD, Lu F, Dong JH. Robotic-assisted laparoscopic anatomic hepatectomy in China: initial experience. Ann Surg. 2011; 253:342–348. PMID: 21135692.21. Packiam V, Bartlett DL, Tohme S, Reddy S, Marsh JW, Geller DA, et al. Minimally invasive liver resection: robotic versus laparoscopic left lateral sectionectomy. J Gastrointest Surg. 2012; 16:2233–2238. PMID: 23054901.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Solo Reduced Port Laparoscopic Left Lateral Sectionectomy
- Single-port plus an additional port robotic complete mesocolic excision and intracorporeal anastomosis using a robotic stapler for right-sided colon cancer
- Laparoscopy-assisted Hepatic Resection in a Patient with Eosinophilic Liver Abscess by Toxocaris Cani Involving Liver
- Feasibility of Left Hemi-hepatectomy for the Treatment of Left Intrahepatic Duct Stones
- Robotic harvest of a latissimus dorsi flap using a single-port surgical robotic system in breast reconstruction