Korean Circ J.
2024 Feb;54(2):78-90. 10.4070/kcj.2023.0200.
Long-Term Outcomes of Modified Cone Reconstruction for Ebstein’s Anomaly in Pediatric Patients in a Single Center
- Affiliations
-
- 1Department of Thoracic and Cardiovascular Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Department of Pediatrics, Cardiovascular Imaging Center, Cardiac and Vascular Center, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2552233
- DOI: http://doi.org/10.4070/kcj.2023.0200
Abstract
- Background and Objective
We aimed to investigate long-term clinical and echocardiographic outcomes, including tricuspid valve durability, annular growth, and left ventricular reverse remodeling, after modified cone reconstruction in patients with Ebstein’s anomaly.
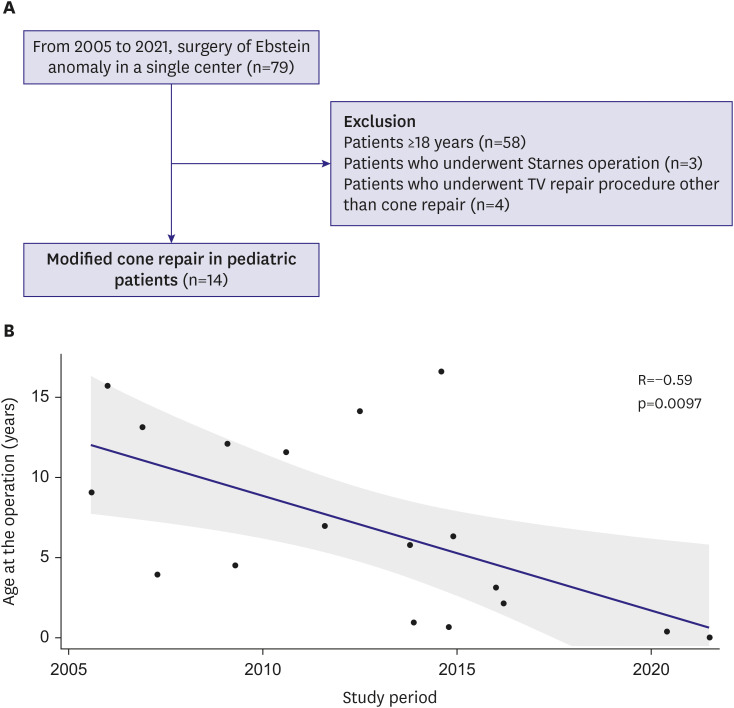
Methods
This was a retrospective analysis of all pediatric patients who underwent modified cone reconstruction for Ebstein’s anomaly at a single tertiary center between January 2005 and June 2021.
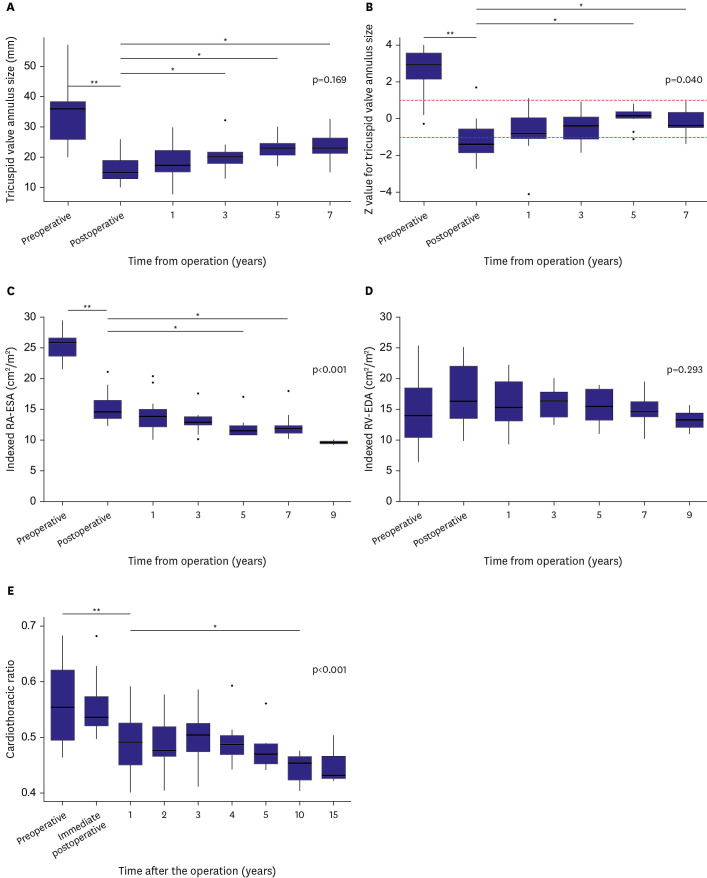
Results
A total of 14 pediatric patients underwent modified cone reconstruction for Ebstein’s anomaly; the median age was 5.8 years (range, 0.01–16.6). There were three patients (21.4%) with Carpentier type B, ten patients with Carpentier type C (71.4%), and one patient with Carpentier type D (7.1%). There was no early or late mortality, arrhythmia, or readmission for heart failure at a 10-year follow-up. There were no cases of more than mild tricuspid stenosis or more than moderate tricuspid regurgitation during the study period, except for one patient with severe tricuspid regurgitation who underwent reoperation. The z value for tricuspid valve annular size significantly decreased immediately after the operation (2.46 vs. −1.15, p<0.001). However, from 1 year to 7 years after surgery, the z values were maintained between −1 and +1. Left ventricular end-systolic volume, end-diastolic volume, and stroke volume increased after surgery and remained elevated until seven years postoperatively.
Conclusions
Ebstein’s anomaly in children can be repaired by modified cone reconstruction with low mortality and morbidity, good tricuspid valve durability, and annular growth relative to somatic growth.
Figure
Reference
-
1. Attenhofer Jost CH, Connolly HM, Dearani JA, Edwards WD, Danielson GK. Ebstein’s anomaly. Circulation. 2007; 115:277–285. PMID: 17228014.2. Carpentier A, Chauvaud S, Macé L, et al. A new reconstructive operation for Ebstein’s anomaly of the tricuspid valve. J Thorac Cardiovasc Surg. 1988; 96:92–101. PMID: 3386297.3. da Silva JP, Baumgratz JF, da Fonseca L, et al. The cone reconstruction of the tricuspid valve in Ebstein’s anomaly. The operation: early and midterm results. J Thorac Cardiovasc Surg. 2007; 133:215–223. PMID: 17198815.4. Dearani JA, Said SM, O’Leary PW, Burkhart HM, Barnes RD, Cetta F. Anatomic repair of Ebstein’s malformation: lessons learned with cone reconstruction. Ann Thorac Surg. 2013; 95:220–226. PMID: 23200240.5. Lange R, Burri M, Eschenbach LK, et al. Da Silva’s cone repair for Ebstein’s anomaly: effect on right ventricular size and function. Eur J Cardiothorac Surg. 2015; 48:316–320. PMID: 25535206.6. Mizuno M, Hoashi T, Sakaguchi H, et al. Application of cone reconstruction for neonatal Ebstein anomaly or tricuspid valve dysplasia. Ann Thorac Surg. 2016; 101:1811–1817. PMID: 26916715.7. Holst KA, Dearani JA, Said S, et al. Improving results of surgery for Ebstein anomaly: where are we after 235 cone repairs? Ann Thorac Surg. 2018; 105:160–168. PMID: 29174783.8. Burri M, Mrad Agua K, Cleuziou J, et al. Cone versus conventional repair for Ebstein’s anomaly. J Thorac Cardiovasc Surg. 2020; 160:1545–1553. PMID: 32711971.9. Schulz A, Marathe SP, Chávez M, et al. The association of age and repair modification with outcome after cone repair for Ebstein’s malformation. Semin Thorac Cardiovasc Surg. 2022; 34:205–212. PMID: 33965550.10. Huang SC, Wu ET, Chen SJ, et al. Surgical strategy toward biventricular repair for severe Ebstein anomaly in neonates and infancy. Ann Thorac Surg. 2017; 104:917–925. PMID: 28434546.11. Danielson GK, Driscoll DJ, Mair DD, Warnes CA, Oliver WC Jr. Operative treatment of Ebstein’s anomaly. J Thorac Cardiovasc Surg. 1992; 104:1195–1202. PMID: 1434695.12. Wackel PL, Dearani JA, Cetta F. Neonatal Ebstein repair-where are we now? Ann Transl Med. 2017; 5:109. PMID: 28361074.13. Postma AV, van Engelen K, van de Meerakker J, et al. Mutations in the sarcomere gene MYH7 in Ebstein anomaly. Circ Cardiovasc Genet. 2011; 4:43–50. PMID: 21127202.14. Bagur RH, Lederlin M, Montaudon M, et al. Images in cardiovascular medicine. Ebstein anomaly associated with left ventricular noncompaction. Circulation. 2008; 118:e662–e664. PMID: 18852371.15. Attenhofer Jost CH, Connolly HM, O’Leary PW, Warnes CA, Tajik AJ, Seward JB. Left heart lesions in patients with Ebstein anomaly. Mayo Clin Proc. 2005; 80:361–368. PMID: 15757018.16. Dearani JA. Ebstein repair: how I do it. JTCVS Tech. 2020; 3:269–276. PMID: 34317896.17. Kumar TK, Boston US, Knott-Craig CJ. Neonatal Ebstein anomaly. Semin Thorac Cardiovasc Surg. 2017; 29:331–337. PMID: 28958645.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cone Repair in Adult Patients with Ebstein Anomaly
- Cone Reconstruction for Tricuspid Valve Repair in a Patient with Ebstein's Anomaly : A case report
- Tricuspid Valve Re-Repair in Ebstein Anomaly Using the Cone Technique
- Current Trends in the Surgical Correction of Ebstein Anomaly
- Morphologic Spectrum of Ebstein's Anomaly