Korean J Orthod.
2024 Jan;54(1):3-15. 10.4041/kjod24.007.
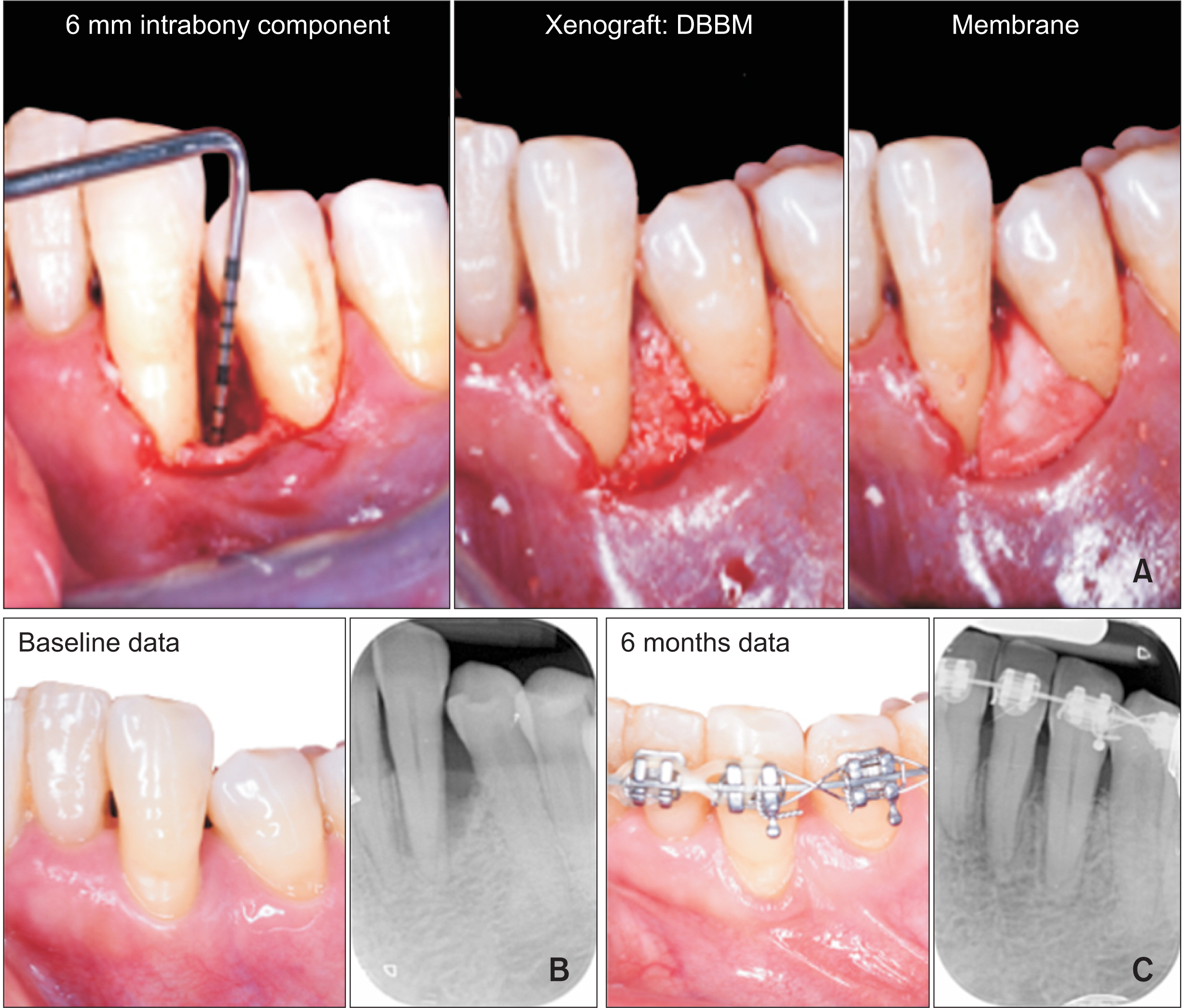
Orthodontic tooth movement after periodontal regeneration of intrabony defects
- Affiliations
-
- 1Section of Orthodontics, Department of Dental Clinical Specialties, Complutense University of Madrid, Madrid, Spain
- 2BIOCRAN (Craniofacial Biology: Orthodontics and Dentofacial Orthopedics) Research Group, Complutense University of Madrid, Madrid, Spain
- 3ETEP (Etiology and Therapy of Periodontal and Peri-implant Diseases) Research Group, Complutense University of Madrid, Madrid, Spain
- KMID: 2551471
- DOI: http://doi.org/10.4041/kjod24.007
Abstract
- The prevalence of intrabony defects in patients with advanced periodontitis stages III and IV is high. These patients usually need both periodontal treatment and orthodontic therapy, including tooth movement through bone defects, to improve masticatory function, aesthetics, and overall quality of life. Clinical practice guidelines recommend periodontal regenerative surgical interventions to resolve these defects and propose initiating orthodontic tooth movement (OTM) once periodontal therapy goals have been met. Surgical interventions using various regenerative technologies like barrier membranes and enamel matrix proteins, combined or not with bone replacement grafts, have proven effective in regenerating lost periodontal tissues. However, the combination of periodontal and orthodontic treatments requires consideration of how periodontal regenerative therapies influence OTM. Studies suggest that regenerated bone may differ in density, composition, vascularity, and cellular activity, potentially affecting the speed and efficiency of OTM, and potential root resorption of moved teeth. Understanding the sequence and timing of implementing OTM after regenerative periodontal interventions is crucial due to their interlinked processes of bone resorption and formation. This narrative review aims to uncover scientific evidence regarding these combined treatments, examining the impacts of different regenerative technologies on OTM and delineating their advantages, limitations, and best practices.
Figure
Reference
-
1. Kim Y. 2017; Study on the perception of orthodontic treatment according to age: a questionnaire survey. Korean J Orthod. 47:215–21. https://doi.org/10.4041/kjod.2017.47.4.215. DOI: 10.4041/kjod.2017.47.4.215. PMID: 28670562. PMCID: PMC5466903.2. Herrera D, Sanz M, Kebschull M, Jepsen S, Sculean A, Berglundh T, et al. 2022; Treatment of stage IV periodontitis: the EFP S3 level clinical practice guideline. J Clin Periodontol. 49 Suppl 24:4–71. https://doi.org/10.1111/jcpe.13639. DOI: 10.1111/jcpe.13639. PMID: 35688447.3. Zasčiurinskienė E, Bulotaitė S, Bjerklin K, Lodienė G, Šidlauskas A, Zaborskis A. 2023; Knowledge, attitudes, and interest in orthodontic treatment: a cross-sectional study in adults with stage III-IV periodontitis and secondary malocclusions. BMC Oral Health. 23:853. https://doi.org/10.1186/s12903-023-03605-8. DOI: 10.1186/s12903-023-03605-8. PMID: 37951899. PMCID: PMC10640755. PMID: 280ed84ef3f94cba887bc687515fa028.4. Sanz M, Herrera D, Kebschull M, Chapple I, Jepsen S, Beglundh T, et al. 2020; Treatment of stage I-III periodontitis-the EFP S3 level clinical practice guideline. J Clin Periodontol. 47(Suppl 22):4–60. https://doi.org/10.1111/jcpe.13290. Erratum in: J Clin Periodontol 2021;48:163. https://doi.org/10.1111/jcpe.13403. DOI: 10.1111/jcpe.13403. PMID: 33370480. PMCID: PMC8094210.5. Nibali L, Koidou VP, Nieri M, Barbato L, Pagliaro U, Cairo F. 2020; Regenerative surgery versus access flap for the treatment of intra-bony periodontal defects: a systematic review and meta-analysis. J Clin Periodontol. 47 Suppl 22:320–51. https://doi.org/10.1111/jcpe.13237. DOI: 10.1111/jcpe.13237. PMID: 31860134.6. Sculean A, Nikolidakis D, Nikou G, Ivanovic A, Chapple IL, Stavropoulos A. 2015; Biomaterials for promoting periodontal regeneration in human intrabony defects: a systematic review. Periodontol 2000. 68:182–216. https://doi.org/10.1111/prd.12086. DOI: 10.1111/prd.12086. PMID: 25867987.7. Attia MS, Shoreibah EA, Ibrahim SA, Nassar HA. 2012; Regenerative therapy of osseous defects combined with orthodontic tooth movement. J Int Acad Periodontol. 14:17–25. https://pubmed.ncbi.nlm.nih.gov/22479985/.8. Alalola B, Asiri A, Binmoghaiseeb I, Baharoon W, Alrassi Y, Alanizy B, et al. 2023; Impact of bone-grafting materials on the rate of orthodontic tooth movement: a systematic review. Cureus. 15:e44535. https://doi.org/10.7759/cureus.44535. DOI: 10.7759/cureus.44535. PMID: 37790063. PMCID: PMC10544668.9. Nibali L, Sultan D, Arena C, Pelekos G, Lin GH, Tonetti M. 2021; Periodontal infrabony defects: systematic review of healing by defect morphology following regenerative surgery. J Clin Periodontol. 48:100–13. https://doi.org/10.1111/jcpe.13381. DOI: 10.1111/jcpe.13381. PMID: 33025619.10. Stavropoulos A, Bertl K, Sculean A, Kantarci A. 2022; Regenerative periodontal therapy in intrabony defects and long-term tooth prognosis. Dent Clin North Am. 66:103–9. https://doi.org/10.1016/j.cden.2021.09.002. DOI: 10.1016/j.cden.2021.09.002. PMID: 34794548.11. Moqadam AS, Arash V, Mirzaie M, Fereydooni M, Haghani H, Rahmani A. 2016; Effect of alveolar ridge preservation with PDFDBA on orthodontic tooth movement rate, formation of gingival invagination and root resorption: a randomized, controlled pilot study. Biomed Pharmacol J. 9:3. https://doi.org/10.13005/bpj/1072. DOI: 10.13005/bpj/1072.12. Tehranchi A, Behnia H, Pourdanesh F, Behnia P, Pinto N, Younessian F. 2018; The effect of autologous leukocyte platelet rich fibrin on the rate of orthodontic tooth movement: a prospective randomized clinical trial. Eur J Dent. 12:350–7. https://doi.org/10.4103/ejd.ejd_424_17. DOI: 10.4103/ejd.ejd_424_17. PMID: 30147398. PMCID: PMC6089057.13. Reyes Pacheco AA, Collins JR, Contreras N, Lantigua A, Pithon MM, Tanaka OM. 2020; Distalization rate of maxillary canines in an alveolus filled with leukocyte-platelet-rich fibrin in adults: a randomized controlled clinical split-mouth trial. Am J Orthod Dentofacial Orthop. 158:182–91. https://doi.org/10.1016/j.ajodo.2020.03.020. DOI: 10.1016/j.ajodo.2020.03.020. PMID: 32591274.14. Barhate UH, Duggal I, Mangaraj M, Sharan J, Duggal R, Jena AK. 2022; Effects of autologous leukocyte-platelet rich fibrin (L-PRF) on the rate of maxillary canine retraction and various biomarkers in gingival crevicular fluid (GCF): a split mouth randomized controlled trial. Int Orthod. 20:100681. https://doi.org/10.1016/j.ortho.2022.100681. DOI: 10.1016/j.ortho.2022.100681. PMID: 36151016.15. Hossain MZ, Kyomen S, Tanne K. 1996; Biologic responses of autogenous bone and beta-tricalcium phosphate ceramics transplanted into bone defects to orthodontic forces. Cleft Palate Craniofac J. 33:277–83. https://doi.org/10.1597/1545-1569_1996_033_0277_broaba_2.3.co_2. DOI: 10.1597/1545-1569_1996_033_0277_broaba_2.3.co_2. PMID: 8827382.16. Araújo MG, Carmagnola D, Berglundh T, Thilander B, Lindhe J. 2001; Orthodontic movement in bone defects augmented with Bio-Oss. An experimental study in dogs. J Clin Periodontol. 28:73–80. https://pubmed.ncbi.nlm.nih.gov/11142670/. DOI: 10.1034/j.1600-051x.2001.280111.x. PMID: 11142670.17. Kawamoto T, Motohashi N, Kitamura A, Baba Y, Takahashi K, Suzuki S, et al. 2002; A histological study on experimental tooth movement into bone induced by recombinant human bone morphogenetic protein-2 in beagle dogs. Cleft Palate Craniofac J. 39:439–48. https://doi.org/10.1597/1545-1569_2002_039_0439_ahsoet_2.0.co_2. DOI: 10.1597/1545-1569_2002_039_0439_ahsoet_2.0.co_2. PMID: 12071792.18. Kawamoto T, Motohashi N, Kitamura A, Baba Y, Suzuki S, Kuroda T. 2003; Experimental tooth movement into bone induced by recombinant human bone morphogenetic protein-2. Cleft Palate Craniofac J. 40:538–43. https://doi.org/10.1597/1545-1569_2003_040_0538_etmibi_2.0.co_2. DOI: 10.1597/1545-1569_2003_040_0538_etmibi_2.0.co_2. PMID: 12943432.19. Zhang D, Chu F, Yang Y, Xia L, Zeng D, Uludağ H, et al. 2011; Orthodontic tooth movement in alveolar cleft repaired with a tissue engineering bone: an experimental study in dogs. Tissue Eng Part A. 17:1313–25. https://doi.org/10.1089/ten.TEA.2010.0490. DOI: 10.1089/ten.tea.2010.0490. PMID: 21226625.20. Seifi M, Ghoraishian SA. 2012; Determination of orthodontic tooth movement and tissue reaction following demineralized freeze-dried bone allograft grafting intervention. Dent Res J (Isfahan). 9:203–8. https://pubmed.ncbi.nlm.nih.gov/22623939/. DOI: 10.4103/1735-3327.95237. PMID: 22623939. PMCID: PMC3353699. PMID: 0ba86559f07944d38cbeb3f26f7ce156.21. Ahn HW, Ohe JY, Lee SH, Park YG, Kim SJ. 2014; Timing of force application affects the rate of tooth movement into surgical alveolar defects with grafts in beagles. Am J Orthod Dentofacial Orthop. 145:486–95. https://doi.org/10.1016/j.ajodo.2013.12.021. DOI: 10.1016/j.ajodo.2013.12.021. PMID: 24703287.22. Seifi M, Arayesh A, Shamloo N, Hamedi R. 2015; Effect of nanocrystalline hydroxyapatite socket preservation on orthodontically induced inflammatory root resorption. Cell J. 16:514–27. https://doi.org/10.22074/cellj.2015.496. DOI: 10.22074/cellj.2015.496. PMID: 25685742. PMCID: PMC4297490.23. Kim KA, Choi EK, Ohe JY, Ahn HW, Kim SJ. 2015; Effect of low-level laser therapy on orthodontic tooth movement into bone-grafted alveolar defects. Am J Orthod Dentofacial Orthop. 148:608–17. https://doi.org/10.1016/j.ajodo.2015.04.034. DOI: 10.1016/j.ajodo.2015.04.034. PMID: 26432316.24. Tanimoto K, Sumi K, Yoshioka M, Oki N, Tanne Y, Awada T, et al. 2015; Experimental tooth movement into new bone area regenerated by use of bone marrow-derived mesenchymal stem cells. Cleft Palate Craniofac J. 52:386–94. https://doi.org/10.1597/12-232. DOI: 10.1597/12-232. PMID: 23782420.25. Machibya FM, Zhuang Y, Guo W, You D, Lin S, Wu D, et al. 2018; Effects of bone regeneration materials and tooth movement timing on canine experimental orthodontic treatment. Angle Orthod. 88:171–8. https://doi.org/10.2319/062017-407. DOI: 10.2319/062017-407. PMID: 29154676. PMCID: PMC8312530.26. Jiang S, Liu T, Wu G, Li W, Feng X, Pathak JL, et al. 2020; BMP2-functionalized biomimetic calcium phosphate graft promotes alveolar defect healing during orthodontic tooth movement in beagle dogs. Front Bioeng Biotechnol. 8:517. https://doi.org/10.3389/fbioe.2020.00517. DOI: 10.3389/fbioe.2020.00517. PMID: 32548104. PMCID: PMC7272671. PMID: f7be293ba9c44bf0b700154db691d9b8.27. Abe T, Kunimatsu R, Tanimoto K. 2023; Comparison of orthodontic tooth movement of regenerated bone induced by carbonated hydroxyapatite or deproteinized bovine bone mineral in beagle dogs. Materials (Basel). 17:112. https://doi.org/10.3390/ma17010112. DOI: 10.3390/ma17010112. PMID: 38203967. PMCID: PMC10779819. PMID: 9734d78963cb4c81885bdc1210f490be.28. Ru N, Liu SS, Bai Y, Li S, Liu Y, Wei X. 2016; BoneCeramic graft regenerates alveolar defects but slows orthodontic tooth movement with less root resorption. Am J Orthod Dentofacial Orthop. 149:523–32. https://doi.org/10.1016/j.ajodo.2015.09.027. DOI: 10.1016/j.ajodo.2015.09.027. PMID: 27021457.29. Möhlhenrich SC, Kniha K, Magnuska Z, Hermanns-Sachweh B, Gremse F, Hölzle F, et al. 2021; Evaluation of different grafting materials for alveolar cleft repair in the context of orthodontic tooth movement in rats. Sci Rep. 11:13586. https://doi.org/10.1038/s41598-021-93033-x. DOI: 10.1038/s41598-021-93033-x. PMID: 34193933. PMCID: PMC8245488. PMID: 6624e5da058a4d9fac8a0ff7324aaf07.30. Möhlhenrich SC, Kniha K, Magnuska Z, Chhatwani S, Hermanns-Sachweh B, Gremse F, et al. 2022; Development of root resorption during orthodontic tooth movement after cleft repair using different grafting materials in rats. Clin Oral Investig. 26:5809–21. https://doi.org/10.1007/s00784-022-04537-3. DOI: 10.1007/s00784-022-04537-3. PMID: 35567639. PMCID: PMC9474460.31. Klein Y, Fleissig O, Stabholz A, Chaushu S, Polak D. 2019; Bone regeneration with bovine bone impairs orthodontic tooth movement despite proper osseous wound healing in a novel mouse model. J Periodontol. 90:189–99. https://doi.org/10.1002/JPER.17-0550. DOI: 10.1002/JPER.17-0550. PMID: 30059146.32. Klein Y, Kunthawong N, Fleissig O, Casap N, Polak D, Chaushu S. 2020; The impact of alloplast and allograft on bone homeostasis: orthodontic tooth movement into regenerated bone. J Periodontol. 91:1067–75. https://doi.org/10.1002/JPER.19-0145. DOI: 10.1002/JPER.19-0145. PMID: 31887228.33. Sheats RD, Strauss RA, Rubenstein LK. 1991; Effect of a resorbable bone graft material on orthodontic tooth movement through surgical defects in the cat mandible. J Oral Maxillofac Surg. 49:1299–303. discussion 1304https://doi.org/10.1016/0278-2391(91)90307-8. DOI: 10.1016/0278-2391(91)90307-8. PMID: 1955922.34. de Ruiter A, Meijer G, Dormaar T, Janssen N, van der Bilt A, Slootweg P, et al. 2011; TCP versus autologous bone for repair of alveolar clefts in a goat model. Cleft Palate Craniofac J. 48:654–62. https://doi.org/10.1597/09-219. DOI: 10.1597/09-219. PMID: 20815732.35. Oltramari PV, de Lima Navarro R, Henriques JF, Taga R, Cestari TM, Ceolin DS, et al. 2007; Orthodontic movement in bone defects filled with xenogenic graft: an experimental study in minipigs. Am J Orthod Dentofacial Orthop. 131:302.e10–7. https://doi.org/10.1016/j.ajodo.2006.07.020. DOI: 10.1016/j.ajodo.2006.07.020. PMID: 17346582.36. Seifi M, Atri F, Yazdani MM. 2014; Effects of low-level laser therapy on orthodontic tooth movement and root resorption after artificial socket preservation. Dent Res J (Isfahan). 11:61–6. https://pubmed.ncbi.nlm.nih.gov/24688562/. PMID: 68bddd5e60d649b2add147c98c2bef72.37. Tietmann C, Bröseler F, Axelrad T, Jepsen K, Jepsen S. 2021; Regenerative periodontal surgery and orthodontic tooth movement in stage IV periodontitis: a retrospective practice-based cohort study. J Clin Periodontol. 48:668–78. https://doi.org/10.1111/jcpe.13442. DOI: 10.1111/jcpe.13442. PMID: 33555608.38. Tietmann C, Jepsen S, Heibrok H, Wenzel S, Jepsen K. 2023; Long-term stability of regenerative periodontal surgery and orthodontic tooth movement in stage IV periodontitis: 10-year data of a retrospective study. J Periodontol. 94:1176–86. https://doi.org/10.1002/JPER.23-0081. DOI: 10.1002/JPER.23-0081. PMID: 37010261.39. Tu CC, Lo CY, Chang PC, Yin HJ. 2022; Orthodontic treatment of periodontally compromised teeth after periodontal regeneration: a restrospective study. J Formos Med Assoc. 121:2065–73. https://doi.org/10.1016/j.jfma.2022.02.021. DOI: 10.1016/j.jfma.2022.02.021. PMID: 35305894.40. Ghezzi C, Vigano V, Francinetti P, Zanotti G, Masiero SA. 2013; Orthodontic treatment after induced periodontal regeneration in deep infrabony defects. Clin Adv Periodontics. 3:24–31. https://doi.org/10.1902/cap.2012.110085. DOI: 10.1902/cap.2012.110085.41. Ghezzi C, Masiero S, Silvestri M, Zanotti G, Rasperini G. 2008; Orthodontic treatment of periodontally involved teeth after tissue regeneration. Int J Periodontics Restorative Dent. 28:559–67. https://pubmed.ncbi.nlm.nih.gov/19146051/.42. Cardaropoli D, Re S, Manuzzi W, Gaveglio L, Cardaropoli G. 2006; Bio-Oss collagen and orthodontic movement for the treatment of infrabony defects in the esthetic zone. Int J Periodontics Restorative Dent. 26:553–9. https://pubmed.ncbi.nlm.nih.gov/17243328/.43. Attia MS, Hazzaa HH, Al-Aziz FA, Elewa GM. 2019; Evaluation of adjunctive use of low-level diode laser biostimulation with combined orthodontic regenerative therapy. J Int Acad Periodontol. 21:63–73. https://pubmed.ncbi.nlm.nih.gov/31522153/.44. Ogihara S, Wang HL. 2010; Periodontal regeneration with or without limited orthodontics for the treatment of 2- or 3-wall infrabony defects. J Periodontol. 81:1734–42. https://doi.org/10.1902/jop.2010.100127. DOI: 10.1902/jop.2010.100127. PMID: 20629545.45. Zampara E, Alshammari M, De Bortoli J, Mullings O, Gkisakis IG, Benalcázar Jalkh EB, et al. 2022; A histologic and histomorphometric evaluation of an allograft, xenograft, and alloplast graft for alveolar ridge preservation in humans: a randomized controlled clinical trial. J Oral Implantol. 48:541–9. https://doi.org/10.1563/aaid-joi-D-21-00012. DOI: 10.1563/aaid-joi-D-21-00012. PMID: 35446950.46. Jepsen K, Tietmann C, Martin C, Kutschera E, Jäger A, Wüllenweber P, et al. 2023; Synergy of regenerative periodontal surgery and orthodontics improves quality of life of patients with stage iv periodontitis: 24-month outcomes of a multicenter RCT. Bioengineering (Basel). 10:695. https://doi.org/10.3390/bioengineering10060695. DOI: 10.3390/bioengineering10060695. PMID: 37370626. PMCID: PMC10295428. PMID: acf44c67de8d46f38abd20b880d241cc.47. Vardimon AD, Nemcovsky CE, Dre E. 2001; Orthodontic tooth movement enhances bone healing of surgical bony defects in rats. J Periodontol. 72:858–64. https://doi.org/10.1902/jop.2001.72.7.858. DOI: 10.1902/jop.2001.72.7.858. PMID: 11495132.48. Jepsen K, Tietmann C, Kutschera E, Wüllenweber P, Jäger A, Cardaropoli D, et al. 2021; The effect of timing of orthodontic therapy on the outcomes of regenerative periodontal surgery in patients with stage IV periodontitis: a multicenter randomized trial. J Clin Periodontol. 48:1282–92. https://doi.org/10.1111/jcpe.13528. DOI: 10.1111/jcpe.13528. PMID: 34312872.49. Attia MS, Shoreibah EA, Ibrahim SA, Nassar HA. 2012; Histological evaluation of osseous defects combined with orthodontic tooth movement. J Int Acad Periodontol. 14:7–16. https://pubmed.ncbi.nlm.nih.gov/22479984/.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect of Calcium Sulfate on the Periodontal Healing of 2-Wall Intrabony Defects in Dogs
- The effects of horizontal orthodontic tooth movement on the periodontally diseased tissue in dogs
- Autologous Stem Cell Application in Periodontal Regeneration Technique (SAI-PRT) Using PDLSCs Directly From an Extracted Tooth...An Insight
- The change of tooth mobility following orthodontic tooth movement ; A short-term study
- The study on the periodontal vascular changes of rat incisors following experimental tooth movement