Intest Res.
2024 Jan;22(1):82-91. 10.5217/ir.2023.00093.
Effectiveness of transabdominal ultrasonography in predicting clinical relapse of Crohn’s disease
- Affiliations
-
- 1Department of Gastroenterology and Hepatology, Hokkaido University Hospital, Sapporo, Japan
- 2Division of Laboratory and Transfusion Medicine, Hokkaido University Hospital, Sapporo, Japan
- 3Diagnostic Center for Sonography, Hokkaido University Hospital, Sapporo, Japan
- KMID: 2551281
- DOI: http://doi.org/10.5217/ir.2023.00093
Abstract
- Background/Aims
Transabdominal ultrasonography (US) helps evaluate Crohn’s disease (CD) activity. We investigated whether the US could predict subsequent adverse outcomes for patients with CD in clinical remission.
Methods
This single-center retrospective study included patients with CD in clinical remission who underwent US between April 2011 and April 2021, focusing on the predictability of subsequent adverse outcomes within 5 years. We used the US-CD, which was calculated using multiple US findings. Predictive variables were assessed using Cox proportional hazards regression analysis, and the predictive value was evaluated using receiver operating characteristic curves.
Results
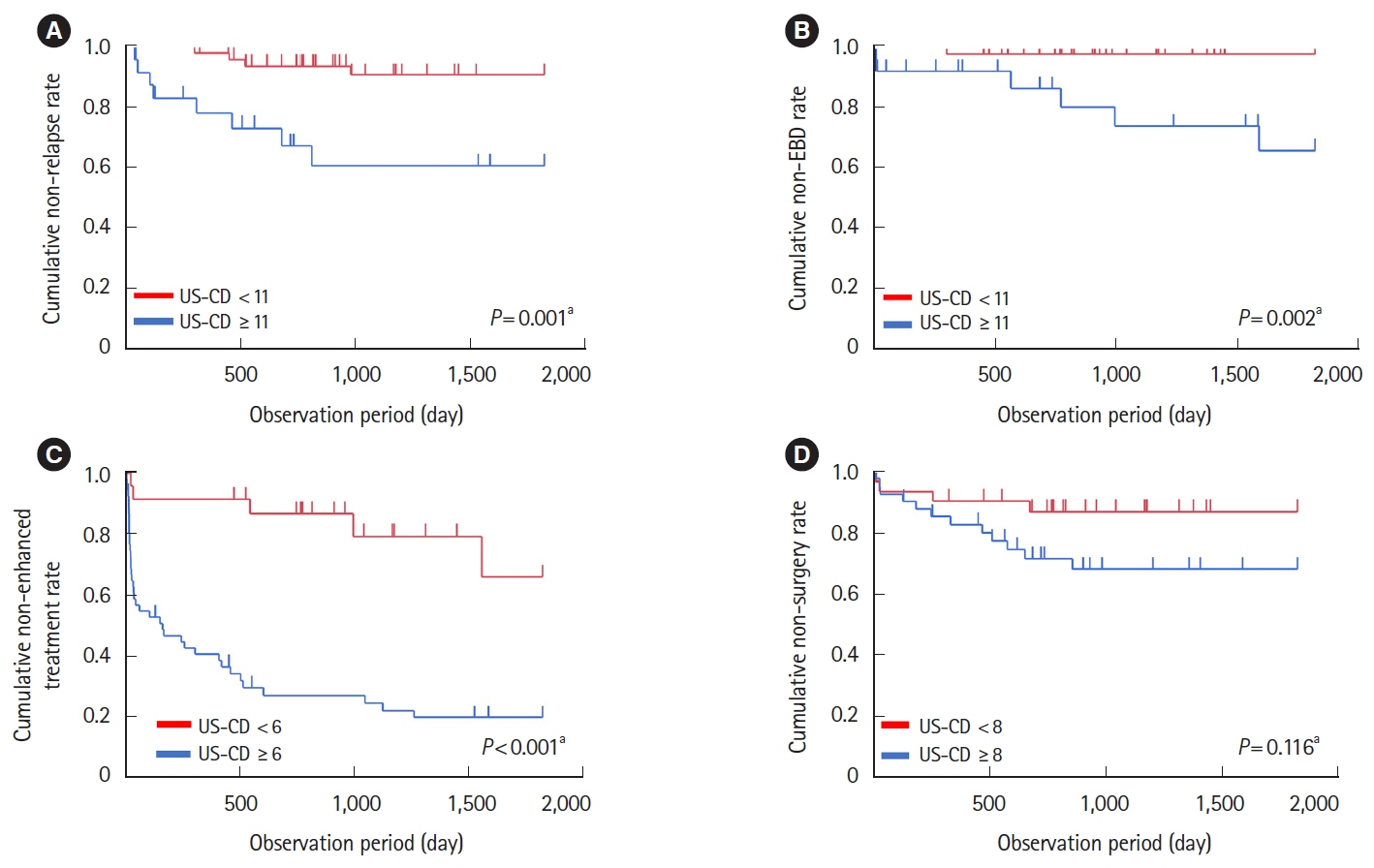
Seventy-three patients were included. During a median follow-up of 1,441 days (range, 41–1,825 days), 16.4% (12/73) experienced clinical relapse, 9.6% (7/73) required endoscopic balloon dilation (EBD), 58.9% (43/73) required enhanced treatment, and 20.5% (15/73) underwent surgery. In the multivariate analysis, US-CD was significantly associated with clinical relapse (P= 0.038) and the need for enhanced treatment (P= 0.005). The area under the receiver operating characteristic curve for predicting clinical relapse and the need for EBD was 0.77 and 0.81, respectively, with US-CD (cutoff value = 11), and that for requiring enhanced treatment was 0.74 with US-CD (cutoff value = 6). Patients with US-CD ≥ 11 demonstrated a significantly higher occurrence of clinical relapse (P= 0.001) and EBD (P= 0.002) within 5 years. Patients with US-CD ≥ 6 experienced a significantly higher likelihood of requiring enhanced treatment (P< 0.001) within 5 years.
Conclusions
High US-CD is associated with subsequent adverse outcomes in patients with CD.
Figure
Reference
-
1. Baumgart DC, Sandborn WJ. Crohn’s disease. Lancet. 2012; 380:1590–1605.
Article2. Peyrin-Biroulet L, Loftus EV Jr, Colombel JF, Sandborn WJ. The natural history of adult Crohn’s disease in populationbased cohorts. Am J Gastroenterol. 2010; 105:289–297.
Article3. Heine GD, Hadithi M, Groenen MJ, Kuipers EJ, Jacobs MA, Mulder CJ. Double-balloon enteroscopy: indications, diagnostic yield, and complications in a series of 275 patients with suspected small-bowel disease. Endoscopy. 2006; 38:42–48.
Article4. Baert F, Moortgat L, Van Assche G, et al. Mucosal healing predicts sustained clinical remission in patients with early-stage Crohn’s disease. Gastroenterology. 2010; 138:463–468.
Article5. Pineton de Chambrun G, Peyrin-Biroulet L, Lémann M, Colombel JF. Clinical implications of mucosal healing for the management of IBD. Nat Rev Gastroenterol Hepatol. 2010; 7:15–29.
Article6. Rondonotti E, Spada C, Adler S, et al. Small-bowel capsule endoscopy and device-assisted enteroscopy for diagnosis and treatment of small-bowel disorders: European Society of Gastrointestinal Endoscopy (ESGE) Technical Review. Endoscopy. 2018; 50:423–446.
Article7. Gionchetti P, Dignass A, Danese S, et al. 3rd European evidence-based consensus on the diagnosis and management of Crohn’s disease 2016: Part 2: surgical management and special situations. J Crohns Colitis. 2017; 11:135–149.
Article8. Mathews JD, Forsythe AV, Brady Z, et al. Cancer risk in 680,000 people exposed to computed tomography scans in childhood or adolescence: data linkage study of 11 million Australians. BMJ. 2013; 346–f2360.9. Low RN, Sebrechts CP, Politoske DA, et al. Crohn disease with endoscopic correlation: single-shot fast spin-echo and gadolinium-enhanced fat-suppressed spoiled gradient-echo MR imaging. Radiology. 2002; 222:652–660.
Article10. Maccioni F, Bruni A, Viscido A, et al. MR imaging in patients with Crohn disease: value of T2-versus T1-weighted gadolinium-enhanced MR sequences with use of an oral superparamagnetic contrast agent. Radiology. 2006; 238:517–530.
Article11. Horsthuis K, Bipat S, Bennink RJ, Stoker J. Inflammatory bowel disease diagnosed with US, MR, scintigraphy, and CT: meta-analysis of prospective studies. Radiology. 2008; 247:64–79.
Article12. Kucharzik T, Maaser C. Intestinal ultrasound and management of small bowel Crohn’s disease. Therap Adv Gastroenterol. 2018; 11:1756284818771367.
Article13. Dong J, Wang H, Zhao J, et al. Ultrasound as a diagnostic tool in detecting active Crohn’s disease: a meta-analysis of prospective studies. Eur Radiol. 2014; 24:26–33.
Article14. Bots S, Nylund K, Löwenberg M, Gecse K, Gilja OH, D’Haens G. Ultrasound for assessing disease activity in IBD patients: a systematic review of activity scores. J Crohns Colitis. 2018; 12:920–929.
Article15. Kucharzik T, Wittig BM, Helwig U, et al. Use of intestinal ultrasound to monitor Crohn’s disease activity. Clin Gastroenterol Hepatol. 2017; 15:535–542.
Article16. Goodsall TM, Jairath V, Feagan BG, et al. Standardisation of intestinal ultrasound scoring in clinical trials for luminal Crohn’s disease. Aliment Pharmacol Ther. 2021; 53:873–886.
Article17. Fernandes SR, Rodrigues RV, Bernardo S, et al. Transmural healing is associated with improved long-term outcomes of patients with Crohn’s disease. Inflamm Bowel Dis. 2017; 23:1403–1409.
Article18. Civitelli F, Nuti F, Oliva S, et al. Looking beyond mucosal healing: effect of biologic therapy on transmural healing in pediatric Crohn’s disease. Inflamm Bowel Dis. 2016; 22:2418–2424.
Article19. Helwig U, Fischer I, Hammer L, et al. Transmural response and transmural healing defined by intestinal ultrasound: new potential therapeutic targets? J Crohns Colitis. 2022; 16:57–67.
Article20. Castiglione F, Testa A, Rea M, et al. Transmural healing evaluated by bowel sonography in patients with Crohn’s disease on maintenance treatment with biologics. Inflamm Bowel Dis. 2013; 19:1928–1934.
Article21. Christensen B, Erlich J, Gibson PR, Turner JR, Hart J, Rubin DT. Histologic healing is more strongly associated with clinical outcomes in ileal Crohn’s disease than endoscopic healing. Clin Gastroenterol Hepatol. 2020; 18:2518–2525.
Article22. Peyrin-Biroulet L, Sandborn W, Sands BE, et al. Selecting Therapeutic Targets in Inflammatory Bowel Disease (STRIDE): determining therapeutic goals for treat-to-target. Am J Gastroenterol. 2015; 110:1324–1338.23. Vaughan R, Tjandra D, Patwardhan A, et al. Toward transmural healing: sonographic healing is associated with improved long-term outcomes in patients with Crohn’s disease. Aliment Pharmacol Ther. 2022; 56:84–94.
Article24. Yamanashi K, Katsurada T, Nishida M, et al. Crohn’s disease activity evaluation by transabdominal ultrasonography: correlation with double-balloon endoscopy. J Ultrasound Med. 2021; 40:2595–2605.
Article25. Van Assche G, Dignass A, Panes J, et al. The second European evidence-based consensus on the diagnosis and management of Crohn’s disease: definitions and diagnosis. J Crohns Colitis. 2010; 4:7–27.
Article26. Gomollón F, Dignass A, Annese V, et al. 3rd European evidence-based consensus on the diagnosis and management of Crohn’s disease 2016: Part 1: diagnosis and medical management. J Crohns Colitis. 2017; 11:3–25.
Article27. Nishida M, Hasegawa Y, Hata J. Basic practices for gastrointestinal ultrasound. J Med Ultrason (2001). 2023; 50:285–310.
Article28. Best WR, Becktel JM, Singleton JW, Kern F Jr. Development of a Crohn’s disease activity index. National Cooperative Crohn’s Disease Study. Gastroenterology. 1976; 70:439–444.29. Allocca M, Craviotto V, Bonovas S, et al. Predictive value of bowel ultrasound in Crohn’s disease: a 12-month prospective study. Clin Gastroenterol Hepatol. 2022; 20:e723–e740.
Article30. Peduzzi P, Concato J, Feinstein AR, Holford TR. Importance of events per independent variable in proportional hazards regression analysis. II. Accuracy and precision of regression estimates. J Clin Epidemiol. 1995; 48:1503–1510.
Article31. Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. 1996; 49:1373–1379.
Article32. Novak KL, Kaplan GG, Panaccione R, et al. A simple ultrasound score for the accurate detection of inflammatory activity in Crohn’s disease. Inflamm Bowel Dis. 2017; 23:2001–2010.
Article33. Sævik F, Eriksen R, Eide GE, Gilja OH, Nylund K. Development and validation of a simple ultrasound activity score for Crohn’s disease. J Crohns Colitis. 2021; 15:115–124.
Article34. Lichtenstein GR, Olson A, Travers S, et al. Factors associated with the development of intestinal strictures or obstructions in patients with Crohn’s disease. Am J Gastroenterol. 2006; 101:1030–1038.
Article35. Bettenworth D, Bokemeyer A, Baker M, et al. Assessment of Crohn’s disease-associated small bowel strictures and fibrosis on cross-sectional imaging: a systematic review. Gut. 2019; 68:1115–1126.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Efficacy of Early Infliximab Treatment for Pediatric Crohn's Disease: A Three-year Follow-up
- Gastric Subepithelial Tumor Diagnosed by Transabdominal Ultrasonography
- Contrast-Enhanced Ultrasonography for the Evaluation of Crohn’s Disease in Pediatric Patients
- Transabdominal Ultrasonography of Seminal Vesicles with Combined Use of Electronic Linear Probe and Mechanical Sector Scanner
- Prevention of Post-operative Recurrence in Crohn's Disease