J Korean Med Sci.
2024 Jan;39(3):e33. 10.3346/jkms.2024.39.e33.
Pediatric Extracorporeal Membrane Oxygenation in Korea: A Multicenter Retrospective Study on Utilization and Outcomes Spanning Over a Decade
- Affiliations
-
- 1Department of Pediatrics, Seoul Medical Center, Seoul, Korea
- 2Department of Pediatrics, Asan Medical Center Children's Hospital, College of Medicine, University of Ulsan, Seoul, Korea
- 3Department of Pediatrics, Keimyung University School of Medicine, Keimyung University Dongsan Hospital, Daegu, Korea
- 4Department of Pediatrics, Jeju National University Hospital, Jeju National University College of Medicine, Jeju, Korea
- 5Department of Pediatrics, School of Medicine, Kyungpook National University, Daegu, Korea
- 6Department of Pediatrics, Eunpyeong St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 7Department of Pediatrics, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 8Department of Pediatrics, Seoul National University College of Medicine, Seoul, Korea
- 9Department of Pediatrics, Sejong General Hospital, Bucheon, Korea
- 10Department of Pediatrics, Hanyang University College of Medicine, Seoul, Korea
- 11Department of Pediatrics, Chungnam National University Hospital, Daejeon, Korea
- 12Department of Critical Care Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 13Department of Pediatrics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 14Department of Pediatrics, Chonnam National University Children's Hospital and Medical School, Gwangju, Korea
- 15Department of Pediatrics, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- 16Department of Thoracic and Cardiovascular Surgery, Yonsei University College of Medicine, Seoul, Korea
- 17Department of Pediatrics, Pusan National University Yangsan Hospital, Pusan National University School of Medicine, Yangsan, Korea
- KMID: 2551180
- DOI: http://doi.org/10.3346/jkms.2024.39.e33
Abstract
- Background
Over the last decade, extracorporeal membrane oxygenation (ECMO) use in critically ill children has increased and is associated with favorable outcomes. Our study aims to evaluate the current status of pediatric ECMO in Korea, with a specific focus on its volume and changes in survival rates based on diagnostic indications.
Methods
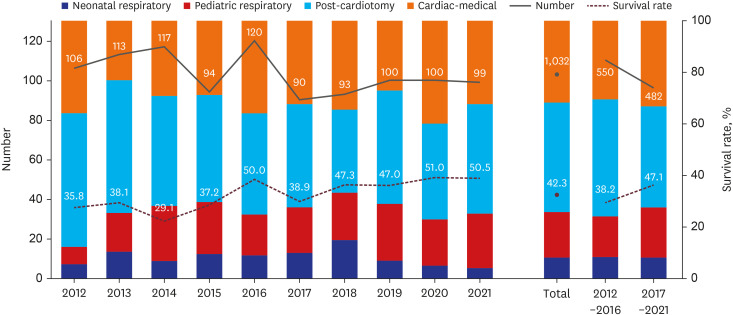
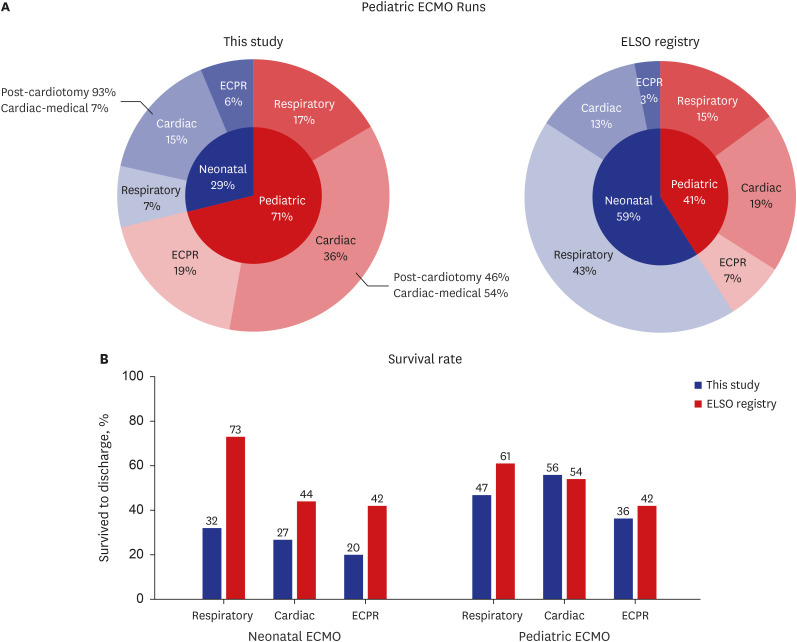
This multicenter study retrospectively analyzed the indications and outcomes of pediatric ECMO over 10 years in patients at 14 hospitals in Korea from January 2012 to December 2021. Four diagnostic categories (neonatal respiratory, pediatric respiratory, postcardiotomy, and cardiac-medical) and trends were compared between periods 1 (2012–2016) and 2 (2017–2021).
Results
Overall, 1065 ECMO runs were performed on 1032 patients, with the annual number of cases remaining unchanged over the 10 years. ECMO was most frequently used for post-cardiotomy (42.4%), cardiac-medical (31.8%), pediatric respiratory (17.5%), and neonatal respiratory (8.2%) cases. A 3.7% increase and 6.1% decrease in pediatric respiratory and post-cardiotomy cases, respectively, were noted between periods 1 and 2. Among the four groups, the cardiac-medical group had the highest survival rate (51.2%), followed by the pediatric respiratory (46.4%), post-cardiotomy (36.5%), and neonatal respiratory (29.4%) groups. A consistent improvement was noted in patient survival over the 10 years, with a significant increase between the two periods from 38.2% to 47.1% (P = 0.004). Improvement in survival was evident in post-cardiotomy cases (30–45%, P = 0.002). Significant associations with mortality were observed in neonates, patients requiring dialysis, and those treated with extracorporeal cardiopulmonary resuscitation (P < 0.001). In pediatric respiratory ECMO, immunocompromised patients also showed a significant correlation with mortality (P < 0.001).
Conclusion
Pediatric ECMO demonstrated a steady increase in overall survival in Korea; however, further efforts are needed since the outcomes remain suboptimal compared with global outcomes.
Figure
Reference
-
1. Rycus P, Stead C. Extracorporeal Life Support Organization registry report 2022. J Card Crit Care. 2022; 6(2):100–102.2. Thiagarajan RR, Barbaro RP, Rycus PT, Mcmullan DM, Conrad SA, Fortenberry JD, et al. Extracorporeal Life Support Organization registry international report 2016. ASAIO J. 2017; 63(1):60–67. PMID: 27984321.3. Barbaro RP, Paden ML, Guner YS, Raman L, Ryerson LM, Alexander P, et al. Pediatric Extracorporeal Life Support Organization registry international report 2016. ASAIO J. 2017; 63(4):456–463. PMID: 28557863.4. Rosario DC, Ambati S. Extracorporeal Membrane Oxygenation in Children. Treasure Island, FL, USA: StatPearls Publishing;2023.5. Haefner SM, Bratton SL, Annich GM, Bartlett RH, Custer JR. Complications of intermittent prone positioning in pediatric patients receiving extracorporeal membrane oxygenation for respiratory failure. Chest. 2003; 123(5):1589–1594. PMID: 12740278.6. Kamdar A, Rintoul N, Raffini L. Anticoagulation in neonatal ECMO. Semin Perinatol. 2018; 42(2):122–128. PMID: 29336832.7. The Society of Thoracic Surgeons-European Association of Cardio-Thoracic Surgery Congenital Heart Surgery Mortality Categories. CHSD Appendix C - STAT Categories. Updated 2020. Accessed August 3, 2023. https://www.sts.org/sites/default/files/CHSD%20Appendix%20C%20-%20STAT%20Categories.pdf .8. Jacobs I, Nadkarni V, Bahr J, Berg RA, Billi JE, Bossaert L, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa). Circulation. 2004; 110(21):3385–3397. PMID: 15557386.9. Choi H, Lee WG, Lee SM, Moon HS, Chung YK, Lee KH, et al. Prolonged extracorporeal lung heart assist (extracorporeal membrane oxygenation) - 4 cases report. Korean J Anesthesiol. 1992; 25(2):424–432.10. Cho HW, Song IA, Oh TK. Trends in extracorporeal membrane oxygenation treatment from 2005 to 2018 in South Korea. Perfusion. 2022; 37(6):545–552. PMID: 34013822.11. Yun J, Kim CY, Son SH, Bae CW, Choi YS, Chung SH. Birth rate transition in the Republic of Korea: trends and prospects. J Korean Med Sci. 2022; 37(42):e304. PMID: 36325608.12. Korean Statistical Information Service. Updated 2023. Accessed March 15, 2023. https://kosis.kr/index/index.do .13. Korean Heart Foundation. 2021 Statistics for cardiac surgery in congenital heart disease. Updated 2022. Accessed March 15, 2023. https://www.heart.or.kr/Home/reference .14. Lee JY. Global burden of congenital heart disease: experience in Korea as a potential solution to the problem. Korean Circ J. 2020; 50(8):691–694. PMID: 32725976.15. Lee JH, Youn Y, Chang YS. Short- and long-term outcomes of very low birth weight infants in Korea: Korean Neonatal Network update in 2019. Clin Exp Pediatr. 2020; 63(8):284–290. PMID: 32023404.16. Shim JW, Jin HS, Bae CW. Changes in survival rate for very-low-birth-weight infants in Korea: comparison with other countries. J Korean Med Sci. 2015; 30(Suppl 1):S25–S34. PMID: 26566354.17. Shin HJ, Park YH, Cho BK. Recent surgical outcomes of congenital heart disease according to Korea Heart Foundation data. Korean Circ J. 2020; 50(8):677–690. PMID: 32212426.18. Choi W, Cho WC, Choi ES, Yun TJ, Park CS. Outcomes after extracorporeal membrane oxygenation in neonates with congenital diaphragmatic hernia: a single-center experience. J Chest Surg. 2021; 54(5):348–355. PMID: 34611083.19. Becher PM, Goßling A, Schrage B, Twerenbold R, Fluschnik N, Seiffert M, et al. Procedural volume and outcomes in patients undergoing VA-ECMO support. Crit Care. 2020; 24(1):291. PMID: 32503646.20. Aso S, Matsui H, Fushimi K, Yasunaga H. In-hospital mortality and successful weaning from venoarterial extracorporeal membrane oxygenation: analysis of 5,263 patients using a national inpatient database in Japan. Crit Care. 2016; 20(1):80. PMID: 27044572.21. Barbaro RP, Odetola FO, Kidwell KM, Paden ML, Bartlett RH, Davis MM, et al. Association of hospital-level volume of extracorporeal membrane oxygenation cases and mortality. Analysis of the extracorporeal life support organization registry. Am J Respir Crit Care Med. 2015; 191(8):894–901. PMID: 25695688.22. Karamlou T, Vafaeezadeh M, Parrish AM, Cohen GA, Welke KF, Permut L, et al. Increased extracorporeal membrane oxygenation center case volume is associated with improved extracorporeal membrane oxygenation survival among pediatric patients. J Thorac Cardiovasc Surg. 2013; 145(2):470–475. PMID: 23246046.23. MacLaren G, Conrad S, Peek G. Indications for pediatric respiratory extracorporeal life support. Updated 2015. Accessed December 20, 2022. https://www.elso.org/portals/0/files/elso%20guidelines%20paeds%20resp_may2015.pdf .24. Goligher EC, Tomlinson G, Hajage D, Wijeysundera DN, Fan E, Jüni P, et al. Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome and posterior probability of mortality benefit in a post hoc Bayesian analysis of a randomized clinical trial. JAMA. 2018; 320(21):2251–2259. PMID: 30347031.25. Munshi L, Walkey A, Goligher E, Pham T, Uleryk EM, Fan E. Venovenous extracorporeal membrane oxygenation for acute respiratory distress syndrome: a systematic review and meta-analysis. Lancet Respir Med. 2019; 7(2):163–172. PMID: 30642776.26. Combes A, Peek GJ, Hajage D, Hardy P, Abrams D, Schmidt M, et al. ECMO for severe ARDS: systematic review and individual patient data meta-analysis. Intensive Care Med. 2020; 46(11):2048–2057. PMID: 33021684.27. Na SJ, Chung CR, Choi HJ, Cho YH, Sung K, Yang JH, et al. The effect of multidisciplinary extracorporeal membrane oxygenation team on clinical outcomes in patients with severe acute respiratory failure. Ann Intensive Care. 2018; 8(1):31. PMID: 29484504.28. Goh KJ, Tan QL, Tay CK, Sewa DW, Lee KC, Phua GC. Impact of an extracorporeal membrane oxygenation intensivist-led multidisciplinary team on venovenous extracorporeal membrane oxygenation outcomes. Crit Care Explor. 2020; 2(12):e0297. PMID: 33251521.29. Brown KL, Ridout DA, Shaw M, Dodkins I, Smith LC, O’Callaghan MA, et al. Healthcare-associated infection in pediatric patients on extracorporeal life support: The role of multidisciplinary surveillance. Pediatr Crit Care Med. 2006; 7(6):546–550. PMID: 17006389.30. Yoon JS, Jhang WK, Choi YH, Lee B, Kim YH, Cho HJ, et al. Current status of pediatric critical care in Korea: results of 2015 national survey. J Korean Med Sci. 2018; 33(49):e308. PMID: 30505252.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Outcomes of Extracorporeal Membrane Oxygenation in Children: An 11-Year Single-Center Experience in Korea
- Successful Retrieval of a Fractured Guidewire during Extracorporeal Membrane Oxygenator Insertion
- A case of rescuing a patient with acute cardiovascular instability from sudden and massive intraoperative pulmonary thromboembolism by extracorporeal membrane oxygenation
- Treatment of acute respiratory failure: extracorporeal membrane oxygenation
- Emergency Bilobectomy under the Extracorporeal Membrane Oxygenation Support for Pediatric Patient with Blunt Traumatic Bronchial Transection: A case report