Anesth Pain Med.
2023 Oct;18(4):331-339. 10.17085/apm.23123.
A comprehensive review of difficult airway management strategies for patient safety
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, School of Medicine, Kyungpook National University, Daegu, Korea
- KMID: 2550912
- DOI: http://doi.org/10.17085/apm.23123
Abstract
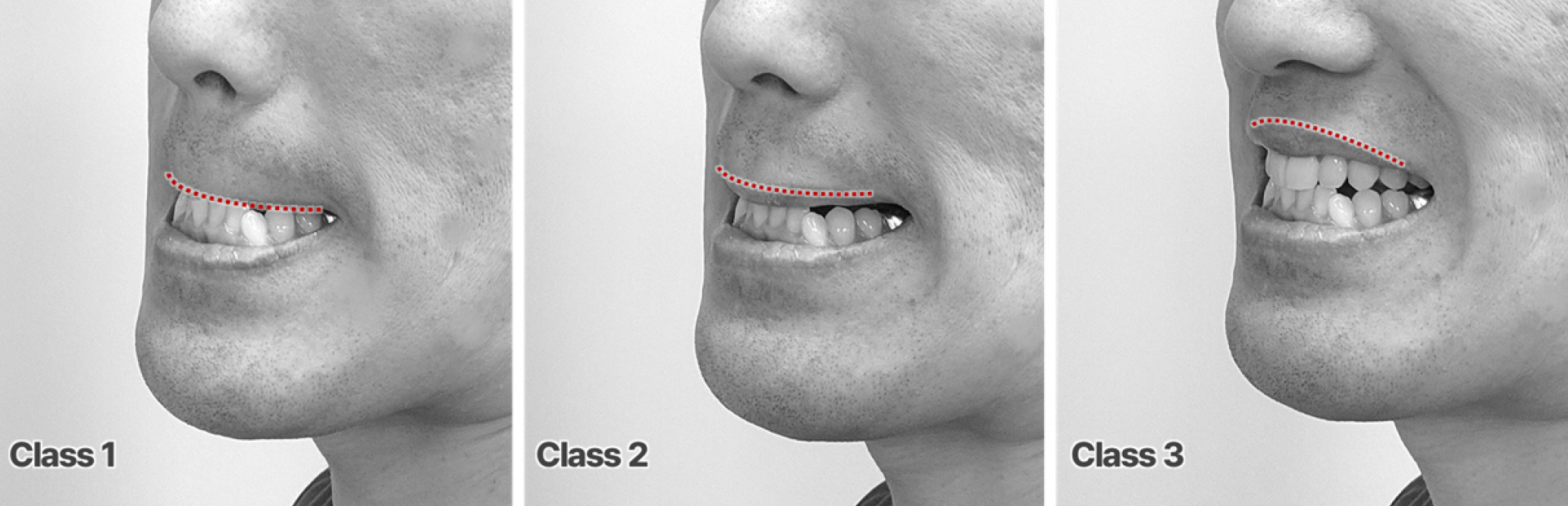
- Difficult airway management is critical to ensuring patient safety. It involves addressing the challenges and failures that can occur, even with skilled healthcare providers, during face mask ventilation, intubation, supraglottic airway placement, invasive airway procedures, or extubation. Although the incidence of the most critical situation in airway management, “cannot intubate, cannot oxygenate,” is low at 0.0019–0.04%, its occurrence can have severe consequences, including dental injury, airway injury, hypoxic brain damage, and even death. This study aimed to offer healthcare providers a comprehensive and evidence-based approach for difficult airway management by reviewing recent guidelines and incorporating the latest evidence-based practices to improve their preparedness and competence in difficult airway management, and thus ultimately contribute to improved patient safety.
Keyword
Figure
Reference
-
1. Niven AS, Doerschug KC. Techniques for the difficult airway. Curr Opin Crit Care. 2013; 19:9–15.
Article2. Apfelbaum JL, Hagberg CA, Connis RT, Abdelmalak BB, Agarkar M, Dutton RP, et al. 2022 American Society of Anesthesiologists Practice Guidelines for management of the difficult airway. Anesthesiology. 2022; 136:31–81.
Article3. Kheterpal S, Han R, Tremper KK, Shanks A, Tait AR, O'Reilly M, et al. Incidence and predictors of difficult and impossible mask ventilation. Anesthesiology. 2006; 105:885–91.
Article4. Langeron O, Masso E, Huraux C, Guggiari M, Bianchi A, Coriat P, et al. Prediction of difficult mask ventilation. Anesthesiology. 2000; 92:1229–36.
Article5. Levitan RM, Heitz JW, Sweeney M, Cooper RM. The complexities of tracheal intubation with direct laryngoscopy and alternative intubation devices. Ann Emerg Med. 2011; 57:240–7.
Article6. Furman WR. Hagberg and Benumof’s airway management, 4th ed. Anesthesia & Analgesia. 2018; 127:e17.
Article7. Ramachandran SK, Mathis MR, Tremper KK, Shanks AM, Kheterpal S. Predictors and clinical outcomes from failed Laryngeal Mask Airway Unique™: a study of 15,795 patients. Anesthesiology. 2012; 116:1217–26.8. Ahmad I, El-Boghdadly K, Bhagrath R, Hodzovic I, McNarry AF, Mir F, et al. Difficult airway society guidelines for awake tracheal intubation (ATI) in adults. Anaesthesia. 2020; 75:509–28.
Article9. Kwon YS, Lee CA, Park S, Ha SO, Sim YS, Baek MS. Incidence and outcomes of cricothyrotomy in the "cannot intubate, cannot oxygenate" situation. Medicine (Baltimore). 2019; 98:e17713.
Article10. Detsky ME, Jivraj N, Adhikari NK, Friedrich JO, Pinto R, Simel DL, et al. Will this patient be difficult to intubate?: The rational clinical examination systematic eeview. Jama. 2019; 321:493–503.11. Siddiqui KM, Hameed F, Ali MA. Diagnostic accuracy of combined mallampati and Wilson score to predict difficult intubation in obese patients: a descriptive cross-sectional study. Anesth Pain Med. 2021; 11:e118626.
Article12. Caro DA. 1 - Basic airway management. In: Emergency medicine. 2nd ed. Edited by Adams JG: Philadelphia, W.B. Saunders. 2013, pp 1-7.e2.13. Frerk C, Mitchell VS, McNarry AF, Mendonca C, Bhagrath R, Patel A, et al. Difficult Airway Society 2015 guidelines for management of unanticipated difficult intubation in adults. Br J Anaesth. 2015; 115:827–48.
Article14. Dixon BJ, Dixon JB, Carden JR, Burn AJ, Schachter LM, Playfair JM, et al. Preoxygenation is more effective in the 25 degrees head-up position than in the supine position in severely obese patients: A randomized controlled study. Anesthesiology. 2005; 102:1110–5; discussion 5A.15. Tanoubi I, Drolet P, Donati F. Optimizing preoxygenation in adults. Can J Anaesth. 2009; 56:449–66.
Article16. Maxwell C, Forrest P. The role of ECMO support in airway procedures. BJA Educ. 2023; 23:248–55.
Article17. Park SC, Ryu JH, Yeom SR, Jeong JW, Cho SJ. Confirmation of endotracheal intubation by combined ultrasonographic methods in the emergency department. Emerg Med Australas. 2009; 21:293–7.
Article18. Grmec S. Comparison of three different methods to confirm tracheal tube placement in emergency intubation. Intensive Care Med. 2002; 28:701–4.
Article19. Williamson JA, Webb RK, Szekely S, Gillies ER, Dreosti AV. The Australian Incident Monitoring Study. Difficult intubation: an analysis of 2000 incident reports. Anaesth Intensive Care. 1993; 21:602–7.
Article20. Dohi S, Inomata S, Tanaka M, Ishizawa Y, Matsumiya N. End-tidal carbon dioxide monitoring during awake blind nasotracheal intubation. J Clin Anesth. 1990; 2:415–9.
Article21. Cook TM, Woodall N, Frerk C. Major complications of airway management in the UK: results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 1: anaesthesia. Br J Anaesth. 2011; 106:617–31.
Article22. Popat M, Mitchell V, Dravid R, Patel A, Swampillai C, Higgs A; Difficult Airway Society Extubation Guidelines Group. Difficult Airway Society Guidelines for the management of tracheal extubation. Anaesthesia. 2012; 67:318–40.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Airway Management
- Use of supraglottic airway devices in children
- Preoperative risk evaluation and perioperative management of patients with obstructive sleep apnea: a narrative review
- Difficult intubation of a patient with progressive multifocal leukoencephalopathy and muscle spasticity: A case report
- Acute traumatic injury and delayed airway obstruction after the use of a GlideScope in a patient with a difficult airway: A case report