Ewha Med J.
2023 Dec;46(S1):e29. 10.12771/emj.2023.e29.
Preventing Anastomotic Leakage, a Devastating Complication of Colorectal Surgery
- Affiliations
-
- 1Department of Surgery, Kyung Hee University Hospital at Gangdong, Kyung Hee University School of Medicine, Seoul, Korea
- KMID: 2550849
- DOI: http://doi.org/10.12771/emj.2023.e29
Abstract
- Anastomotic leakage (AL) after colorectal surgery is a significant concern, as it can lead to adverse functional and oncologic outcomes. Numerous studies have been conducted with the aim of identifying risk factors for AL and developing strategies to prevent its occurrence, thereby reducing the severe morbidity associated with AL. The intraoperative method for reducing AL includes a mechanical assessment of AL, an assessment of bowel perfusion, drain placement, and the creation of diverting stomas. The anastomosis technique is also associated with AL, and the appropriate selection and accurate application of anastomotic methods are crucial for preventing AL. Indocyanine green fluorescence imaging has recently gained popularity as a method for assessing bowel perfusion. While it is useful for detecting bowel perfusion, standardized protocols and measurement methods need to be established to ensure its reliability and effectiveness in clinical practice. The use of intraoperative drains to reduce AL has produced inconsistent results, and the routine adoption of this practice is not currently recommended. Diverting stomas can be used to help reduce the morbidity associated with AL. However, it is important to carefully consider the complications that can arise directly from the stoma itself. It should be noted that while a stoma can reduce AL, it cannot completely prevent it. This descriptive review examines various intraoperative methods aimed at reducing AL, discussing their effectiveness in reducing AL.
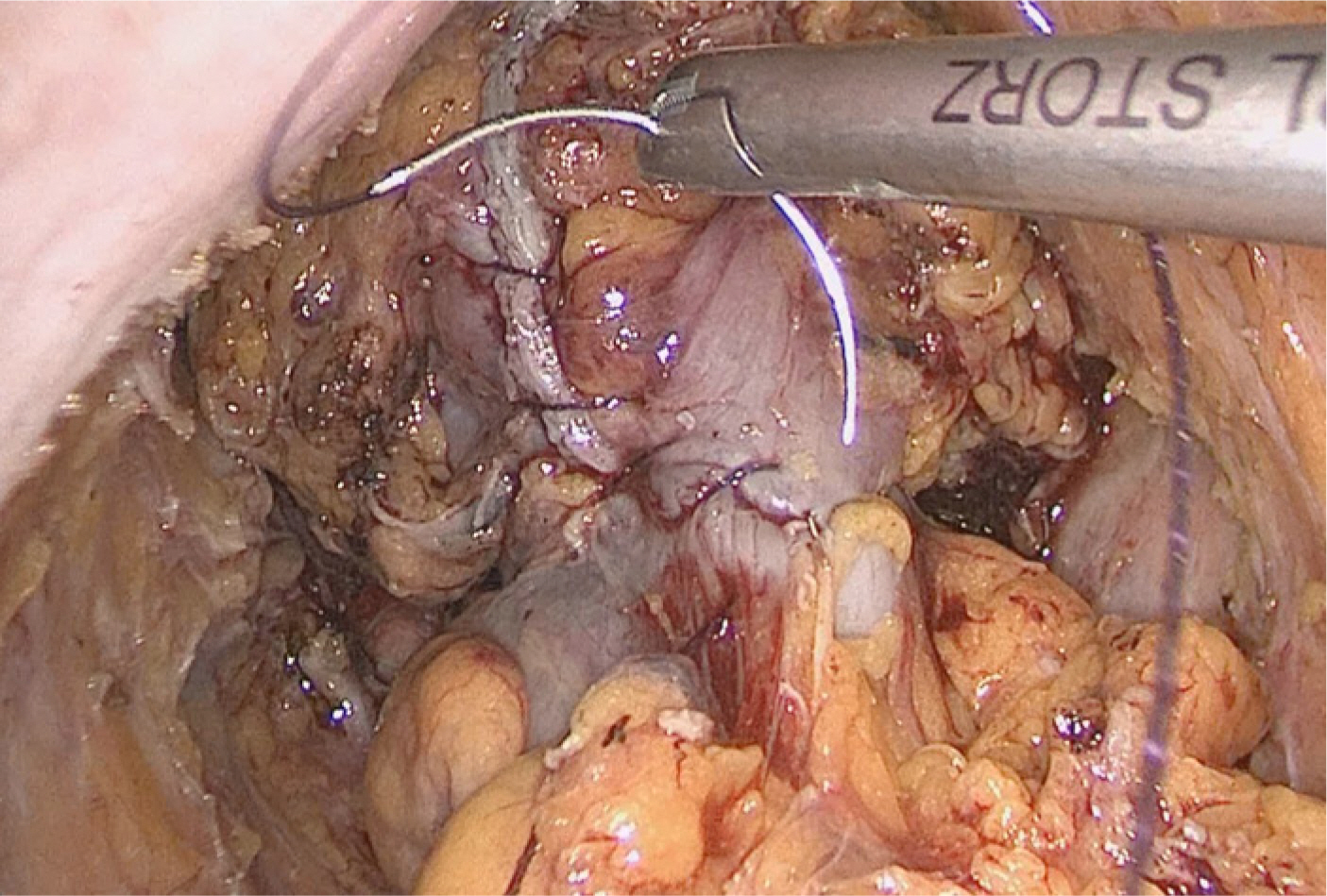
Figure
Reference
-
References
1. Kim MH, Park S, Yi N, Kang B, Park IJ. Colorectal cancer mortality trends in the era of cancer survivorship in Korea: 2000–2020. Ann Coloproctol. 2022; 38(5):343–352. DOI: 10.3393/ac.2022.00535.0076. PMID: 36353833. PMCID: PMC9650346.2. Sauer R, Liersch T, Merkel S, Fietkau R, Hohenberger W, Hess C, et al. Preoperative versus postoperative chemoradiotherapy for locally advanced rectal cancer: results of the German CAO/ARO/AIO-94 randomized phase III trial after a median follow-up of 11 years. J Clin Oncol. 2012; 30(16):1926–1933. DOI: 10.1200/JCO.2011.40.1836. PMID: 22529255.3. Clinical Outcomes of Surgical Therapy Study Group. A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med. 2004; 350(20):2050–2059. DOI: 10.1056/NEJMoa032651. PMID: 15141043.4. Mody K, Baldeo C, Bekaii-Saab T. Antiangiogenic therapy in colorectal cancer. Cancer J. 2018; 24(4):165–170. DOI: 10.1097/PPO.0000000000000328. PMID: 30119079.5. Park IJ. Precision medicine for primary rectal cancer will become a reality. Ann Coloproctol. 2022; 38(4):281–282. DOI: 10.3393/ac.2022.00500.0071. PMID: 36059074. PMCID: PMC9441542.6. Jutesten H, Buchwald PL, Angenete E, Rutegård M, Lydrup ML. High risk of low anterior resection syndrome in long-term follow-up after anastomotic leakage in anterior resection for rectal cancer. Dis Colon Rectum. 2022; 65(10):1264–1273. DOI: 10.1097/DCR.0000000000002334. PMID: 35482994.7. Kim S, Kang SI, Kim SH, Kim JH. The effect of anastomotic leakage on the incidence and severity of low anterior resection syndrome in patients undergoing proctectomy: a propensity score matching analysis. Ann Coloproctol. 2021; 37(5):281–290. DOI: 10.3393/ac.2021.03.15. PMID: 34098631. PMCID: PMC8566143.8. Koedam TWA, Bootsma BT, Deijen CL, van De Brug T, Kazemier G, Cuesta MA, et al. Oncological outcomes after anastomotic leakage after surgery for colon or rectal cancer: increased risk of local recurrence. Ann Surg. 2022; 275(2):e420–e427. DOI: 10.1097/SLA.0000000000003889. PMID: 32224742.9. Ng JY, Chen CC. Transanal total mesorectal excision for rectal cancer: it’s come a long way and here to stay. Ann Coloproctol. 2022; 38(4):283–289. DOI: 10.3393/ac.2022.00374.0053. PMID: 36059075. PMCID: PMC9441544.10. Park JW, Kang SB, Hao J, Lim SB, Choi HS, Kim DW, et al. Open versus laparoscopic surgery for mid or low rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): 10-year follow-up of an open-label, non-inferiority, randomised controlled trial. Lancet Gastroenterol Hepatol. 2021; 6(7):569–577. DOI: 10.1016/S2468-1253(21)00094-7. PMID: 33894918.11. Piozzi GN, Kim SH. Robotic intersphincteric resection for low rectal cancer: technical controversies and a systematic review on the perioperative, oncological, and functional outcomes. Ann Coloproctol. 2021; 37(6):351–367. DOI: 10.3393/ac.2021.00836.0119. PMID: 34784706. PMCID: PMC8717069.12. Jayne D, Pigazzi A, Marshall H, Croft J, Corrigan N, Copeland J, et al. Effect of robotic-assisted vs conventional laparoscopic surgery on risk of conversion to open laparotomy among patients undergoing resection for rectal cancer: the ROLARR randomized clinical trial. JAMA. 2017; 318(16):1569–1580. DOI: 10.1001/jama.2017.7219. PMID: 29067426. PMCID: PMC5818805.13. Varela C, Nassr M, Razak A, Kim NK. Double-layered hand-sewn anastomosis: a valuable resource for the colorectal surgeon. Ann Coloproctol. 2022; 38(3):271–275. DOI: 10.3393/ac.2021.00990.0141. PMID: 35295072. PMCID: PMC9263307.14. Slieker JC, Daams F, Mulder IM, Jeekel J, Lange JF. Systematic review of the technique of colorectal anastomosis. JAMA Surg. 2013; 148(2):190–201. DOI: 10.1001/2013.jamasurg.33. PMID: 23426599.15. Radovanovic Z, Petrovic T, Radovanovic D, Breberina M, Golubovic A, Lukic D. Single versus double stapling anastomotic technique in rectal cancer surgery. Surg Today. 2014; 44:1026–1031. DOI: 10.1007/s00595-013-0646-x. PMID: 23801054.16. Varela C, Kim NK. Surgical treatment of low-lying rectal cancer: updates. Ann Coloproctol. 2021; 37(6):395–424. DOI: 10.3393/ac.2021.00927.0132. PMID: 34961303. PMCID: PMC8717072.17. Balciscueta Z, Uribe N, Caubet L, López M, Torrijo I, Tabet J, et al. Impact of the number of stapler firings on anastomotic leakage in laparoscopic rectal surgery: a systematic review and meta-analysis. Tech Coloproctol. 2020; 24(9):919–925. DOI: 10.1007/s10151-020-02240-7. PMID: 32451807.18. Braunschmid T, Hartig N, Baumann L, Dauser B, Herbst F. Influence of multiple stapler firings used for rectal division on colorectal anastomotic leak rate. Surg Endosc. 2017; 31(12):5318–5326. DOI: 10.1007/s00464-017-5611-0. PMID: 28634627. PMCID: PMC5715046.19. Mizuuchi Y, Tanabe Y, Sada M, Tamura K, Nagayoshi K, Nagai S, et al. Cross-sectional area of psoas muscle as a predictive marker of anastomotic failure in male rectal cancer patients: Japanese single institutional retrospective observational study. Ann Coloproctol. 2022; 38(5):353–361. DOI: 10.3393/ac.2022.00122.0017. PMID: 35410111. PMCID: PMC9650344.20. Ito M, Sugito M, Kobayashi A, Nishizawa Y, Tsunoda Y, Saito N. Relationship between multiple numbers of stapler firings during rectal division and anastomotic leakage after laparoscopic rectal resection. Int J Colorectal Dis. 2008; 23(7):703–707. DOI: 10.1007/s00384-008-0470-8. PMID: 18379795.21. Lee S, Ahn B, Lee S. The relationship between the number of intersections of staple lines and anastomotic leakage after the use of a double stapling technique in laparoscopic colorectal surgery. Surg Laparosc Endosc Percutan Tech. 2017; 27(4):273–281. DOI: 10.1097/SLE.0000000000000422. PMID: 28614172. PMCID: PMC5542784.22. Chen ZF, Liu X, Jiang WZ, Guan GX. Laparoscopic double-stapled colorectal anastomosis without “dog-ears”. Tech Coloproctol. 2016; 20:243–247. DOI: 10.1007/s10151-016-1437-3. PMID: 26902367.23. De Robles MS, John Young C. Triple-staple technique effectively reduces operating time for rectal anastomosis. Ann Coloproctol. 2021; 37(1):16–20. DOI: 10.3393/ac.2019.06.30. PMID: 32054240. PMCID: PMC7989554.24. Maeda K, Nagahara H, Shibutani M, Ohtani H, Sakurai K, Toyokawa T, et al. Efficacy of intracorporeal reinforcing sutures for anastomotic leakage after laparoscopic surgery for rectal cancer. Surg Endosc. 2015; 29(12):3535–3542. DOI: 10.1007/s00464-015-4104-2. PMID: 25673349.25. Lin H, Yu M, Ye G, Qin S, Fang H, Jing R, et al. Intracorporeal reinforcement with barbed suture is associated with low anastomotic leakage rates after laparoscopic low anterior resection for rectal cancer: a retrospective study. BMC Surg. 2022; 22(1):335. DOI: 10.1186/s12893-022-01782-x. PMID: 36085058. PMCID: PMC9461121.26. Ban B, Shang A, Shi J. Efficacy of staple line reinforcement by barbed suture for preventing anastomotic leakage in laparoscopic rectal cancer surgery. World J Gastrointest Surg. 2022; 14(8):821–832. DOI: 10.4240/wjgs.v14.i8.821. PMID: 36157360. PMCID: PMC9453327.27. Jiang TY, Zang L, Dong F, Feng B, Zong YP, Sun J, et al. Effect of different reinforcement methods on anastomotic leakage prevention after laparoscopic double anastomosis. J Surg Oncol. 2021; 123((Suppl 1)):S81–S87. DOI: 10.1002/jso.26333.28. Kim IY, Kim BR, Kim YW. Applying reinforcing sutures to stapled colorectal anastomosis after low anterior resection for rectal cancer. Eur J Surg Oncol. 2015; 41(6):808–809. DOI: 10.1016/j.ejso.2015.03.230. PMID: 25890493.29. Ryu HS, Lim SB, Choi ET, Song I, Lee JL, Kim CW, et al. Intraoperative perfusion assessment of the proximal colon by a visual grading system for safe anastomosis after resection in left-sided colorectal cancer patients. Sci Rep. 2021; 11(1):2746. DOI: 10.1038/s41598-021-82486-9. PMID: 33531598. PMCID: PMC7854740.30. Son GM, Ahn H, Lee IY, Ha GW. Multifunctional indocyanine green applications for fluorescence-guided laparoscopic colorectal surgery. Ann Coloproctol. 2021; 37(3):133–140. DOI: 10.3393/ac.2021.05.07. PMID: 34102813. PMCID: PMC8273708.31. Alekseev M, Rybakov E, Khomyakov E, Zarodnyuk I, Shelygin Y. Intraoperative fluorescence angiography as an independent factor of anastomotic leakage and a nomogram for predicting leak for colorectal anastomoses. Ann Coloproctol. 2022; 38(5):380–386. DOI: 10.3393/ac.2021.00171.0024. PMID: 34289650. PMCID: PMC9650343.32. Jafari MD, Pigazzi A, McLemore EC, Mutch MG, Haas E, Rasheid SH, et al. Perfusion assessment in left-sided/low anterior resection (PILLAR III): a randomized, controlled, parallel, multicenter study assessing perfusion outcomes with PINPOINT near-infrared fluorescence imaging in low anterior resection. Dis Colon Rectum. 2021; 64(8):995–1002. DOI: 10.1097/DCR.0000000000002007. PMID: 33872284.33. Shen Y, Yang T, Yang J, Meng W, Wang Z. Intraoperative indocyanine green fluorescence angiography to prevent anastomotic leak after low anterior resection for rectal cancer: a meta-analysis. ANZ J Surg. 2020; 90(11):2193–2200. DOI: 10.1111/ans.15809. PMID: 32159273.34. Kim JC, Lee JL, Park SH. Interpretative guidelines and possible indications for indocyanine green fluorescence imaging in robot-assisted sphincter-saving operations. Dis Colon Rectum. 2017; 60(4):376–384. DOI: 10.1097/DCR.0000000000000782. PMID: 28267004.35. Crafa F, Striano A, Esposito F, Rossetti ARR, Baiamonte M, Gianfreda V, et al. The “reverse air leak test”: a new technique for the assessment of low colorectal anastomosis. Ann Coloproctol. 2022; 38(1):20–27. DOI: 10.3393/ac.2020.09.21.1. PMID: 33332954. PMCID: PMC8898631.36. Aly M, O'Brien JW, Clark F, Kapur S, Stearns AT, Shaikh I. Does intra-operative flexible endoscopy reduce anastomotic complications following left-sided colonic resections? A systematic review and meta-analysis. Colorectal Dis. 2019; 21(12):1354–1363. DOI: 10.1111/codi.14740. PMID: 31243879.37. Ha RK, Han KS, Park SS, Sohn DK, Hong CW, Kim BC, et al. Efficacy and safety of endoscopic clipping for acute anastomotic bleeding after colorectal surgery. Ann Coloproctol. 2022; 38(3):262–265. DOI: 10.3393/ac.2021.00297.0042. PMID: 34696537. PMCID: PMC9263306.38. Shigeta K, Okabayashi K, Baba H, Hasegawa H, Tsuruta M, Yamafuji K, et al. A meta-analysis of the use of a transanal drainage tube to prevent anastomotic leakage after anterior resection by double-stapling technique for rectal cancer. Surg Endosc. 2016; 30(2):543–550. DOI: 10.1007/s00464-015-4237-3. PMID: 26091985.39. Guo C, Fu Z, Qing X, Deng M. Prophylactic transanal drainage tube placement for preventing anastomotic leakage after anterior resection for rectal cancer: a meta-analysis. Colorectal Dis. 2022; 24(11):1273–1284. DOI: 10.1111/codi.16231. PMID: 35735261.40. Denost Q, Rouanet P, Faucheron JL, Panis Y, Meunier B, Cotte E, et al. To drain or not to drain infraperitoneal anastomosis after rectal excision for cancer: the GRECCAR 5 randomized trial. Ann Surg. 2017; 265(3):474–480. DOI: 10.1097/SLA.0000000000001991. PMID: 27631776.41. Podda M, Di Saverio S, Davies RJ, Atzeni J, Balestra F, Virdis F, et al. Prophylactic intra-abdominal drainage following colorectal anastomoses. A systematic review and meta-analysis of randomized controlled trials. Am J Surg. 2020; 219(1):164–174. DOI: 10.1016/j.amjsurg.2019.05.006. PMID: 31138400.42. Maeda K. Prolapse of intestinal stoma. Ann Coloproctol. 2022; 38(5):335–342. DOI: 10.3393/ac.2022.00465.0066. PMID: 36353832. PMCID: PMC9650348.43. Kim HS, Kang JH, Kim H, Kim YH, Bae H, Kim NK. Clostridium difficile infection after ileostomy reversal. Ann Coloproctol. 2021; 37((Suppl 1)):S4–S6. DOI: 10.3393/ac.2019.09.24. PMID: 32178491. PMCID: PMC8359696.44. Hüser N, Michalski CW, Erkan M, Schuster T, Rosenberg R, Kleeff J, et al. Systematic review and meta-analysis of the role of defunctioning stoma in low rectal cancer surgery. Ann Surg. 2008; 248(1):52–60. DOI: 10.1097/SLA.0b013e318176bf65. PMID: 18580207.45. Ahmad NZ, Abbas MH, Khan SU, Parvaiz A. A meta-analysis of the role of diverting ileostomy after rectal cancer surgery. Int J Colorectal Dis. 2021; 36(3):445–455. DOI: 10.1007/s00384-020-03771-z. PMID: 33064212.46. Park Y, Choi DU, Kim HO, Kim YB, Min C, Son JT, et al. Comparison of blowhole colostomy and loop ostomy for palliation of acute malignant colonic obstruction. Ann Coloproctol. 2022; 38(4):319–326. DOI: 10.3393/ac.2021.00682.0097. PMID: 35255204. PMCID: PMC9441536.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Omental Free-Shaped Flap Reinforcement on the Anastomosis and Dissected Area (OFFROAD) Following Reconstruction after Gastrectomy: A Retrospective Case-Control Study
- Optimal anastomotic technique in rectal surgery to prevent anastomotic leakage
- Transanal tube placement for prevention of anastomotic leakage following low anterior resection for rectal cancer: a systematic review and meta-analysis
- Risk Factors for Anastomotic Leakage after Laparoscopic Rectal Resection in Rectal Cancer: Does Laparoscopic Rectal Resection Increase Anastomotic Leakage Rate?
- Transanal gauze packing to manage massive presacral bleeding secondary to prescral abscess caused by rectal anastomotic leakage: a novel approach