Ann Surg Treat Res.
2015 Dec;89(6):313-318. 10.4174/astr.2015.89.6.313.
Transanal tube placement for prevention of anastomotic leakage following low anterior resection for rectal cancer: a systematic review and meta-analysis
- Affiliations
-
- 1Research Institute of Clinical Medicine of Chonbuk National University-Biomedical Research Institute of Chonbuk National University Hospital, Jeonju, Korea. gsminro@jbnu.ac.kr
- 2Institute for Evidence-Based Medicine, Department of Preventive Medicine, Korea University College of Medicine, Seoul, Korea.
- KMID: 2148306
- DOI: http://doi.org/10.4174/astr.2015.89.6.313
Abstract
- PURPOSE
Anastomotic leakage following low anterior resection (LAR) for rectal cancer is a serious complication that increases morbidity and mortality rates. Transanal tube placement may reduce postoperative anastomotic leakage rate by reducing intraluminal pressure and preventing fecal extrusion through the staple line. This meta-analysis evaluated the effectiveness of transanal tube placement to prevent anastomotic leakage after LAR for rectal cancer using a stapling technique.
METHODS
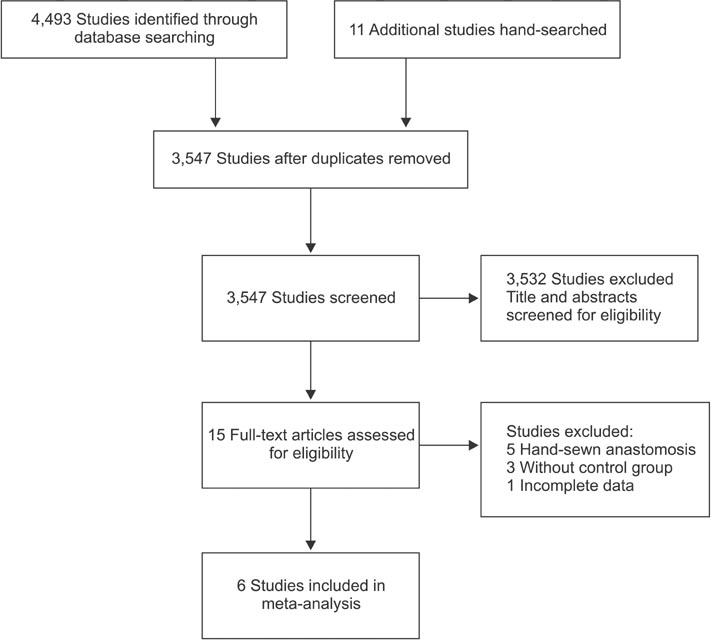
A systematic review of the literature was consistent with the recommendations of the PRISMA (preferred reporting items for systematic reviews and meta-analyses) statement. Multiple comprehensive databases, including PubMed, Embase, Cochrane Library and KoreaMed, were searched. The main study outcomes were anastomotic leakage.
RESULTS
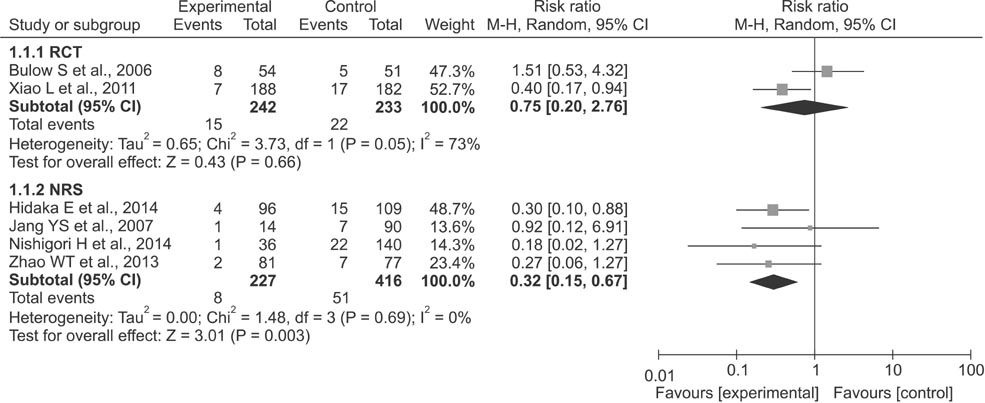
Two randomized clinical trials and 4 nonrandomized studies involving 1,118 patients were included. Subgroup analyses of randomized clinical trials found that transanal tube placement had no effect on study outcomes. Meta-analysis of nonrandomized studies showed that transanal tube placement was associated with a lower incidence of anastomotic leakage (relative risk, 0.32; 95% CI, 0.15-0.67; I2 = 0%).
CONCLUSION
Transanal tube placement may be effective in preventing or reducing the occurrence of anastomotic leakage after LAR for rectal cancer using a stapling technique. Randomized clinical trials with sufficient power are needed to confirm the benefit of transanal tube placement.
MeSH Terms
Figure
Reference
-
1. Akyol AM, McGregor JR, Galloway DJ, Murray GD, George WD. Anastomotic leaks in colorectal cancer surgery: a risk factor for recurrence? Int J Colorectal Dis. 1991; 6:179–183.2. Fujita S, Teramoto T, Watanabe M, Kodaira S, Kitajima M. Anastomotic leakage after colorectal cancer surgery: a risk factor for recurrence and poor prognosis. Jpn J Clin Oncol. 1993; 23:299–302.3. Wang J. Principle and complications of anus-preserving operation for low rectal cancer. J Clinical Surg. 2005; 13:678–679.4. Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009; 151:264–269. W645. Higgins JP, Green S, editors. Cochrane handbook for systematic reviews of interventions. version 5.1.0 [Internet]. The Cochrane Collaboration;2011. uptated 2011 Mar. cited 2014 Dec 11. Available from: www.cochrane-handbook.org.6. Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M. . The Newcastle Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses. Ottawa (ON): Ottawa Hospital Research Institute;c2014. cited 2014 Dec 17. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.7. Zhao WT, Hu FL, Li YY, Li HJ, Luo WM, Sun F. Use of a transanal drainage tube for prevention of anastomotic leakage and bleeding after anterior resection for rectal cancer. World J Surg. 2013; 37:227–232.8. Bulow S, Bulut O, Christensen IJ, Harling H. Rectal Stent Study Group. Transanal stent in anterior resection does not prevent anastomotic leakage. Colorectal Dis. 2006; 8:494–496.9. Vignali A, Fazio VW, Lavery IC, Milsom JW, Church JM, Hull TL, et al. Factors associated with the occurrence of leaks in stapled rectal anastomoses: a review of 1,014 patients. J Am Coll Surg. 1997; 185:105–113.10. Bertelsen CA, Andreasen AH, Jorgensen T, Harling H. Danish Colorectal Cancer Group. Anastomotic leakage after anterior resection for rectal cancer: risk factors. Colorectal Dis. 2010; 12:37–43.11. Cong ZJ, Fu CG, Wang HT, Liu LJ, Zhang W, Wang H. Influencing factors of symptomatic anastomotic leakage after anterior resection of the rectum for cancer. World J Surg. 2009; 33:1292–1297.12. Snijders HS, Wouters MW, van Leersum NJ, Kolfschoten NE, Henneman D, de Vries AC, et al. Meta-analysis of the risk for anastomotic leakage, the postoperative mortality caused by leakage in relation to the overall postoperative mortality. Eur J Surg Oncol. 2012; 38:1013–1019.13. Eberl T, Jagoditsch M, Klingler A, Tschmelitsch J. Risk factors for anastomotic leakage after resection for rectal cancer. Am J Surg. 2008; 196:592–598.14. Lee WS, Yun SH, Roh YN, Yun HR, Lee WY, Cho YB, et al. Risk factors and clinical outcome for anastomotic leakage after total mesorectal excision for rectal cancer. World J Surg. 2008; 32:1124–1129.15. Park JS, Choi GS, Kim SH, Kim HR, Kim NK, Lee KY, et al. Multicenter analysis of risk factors for anastomotic leakage after laparoscopic rectal cancer excision: the Korean laparoscopic colorectal surgery study group. Ann Surg. 2013; 257:665–671.16. Hidaka E, Ishida F, Mukai S, Nakahara K, Takayanagi D, Maeda C, et al. Efficacy of transanal tube for prevention of anastomotic leakage following laparoscopic low anterior resection for rectal cancers: a retrospective cohort study in a single institution. Surg Endosc. 2015; 29:863–867.17. Amin AI, Ramalingam T, Sexton R, Heald RJ, Leppington-Clarke A, Moran BJ. Comparison of transanal stent with defunctioning stoma in low anterior resection for rectal cancer. Br J Surg. 2003; 90:581–582.18. Xiao L, Zhang WB, Jiang PC, Bu XF, Yan Q, Li H, et al. Can transanal tube placement after anterior resection for rectal carcinoma reduce anastomotic leakage rate? A single-institution prospective randomized study. World J Surg. 2011; 35:1367–1377.19. Jang YS, Lim KH, Kang BM, Choi GS, Jun SH. Anastomosis protection with Mallecot in low rectal anastomosis. J Korean Soc Coloproctol. 2007; 23:420–423.20. Nishigori H, Ito M, Nishizawa Y, Nishizawa Y, Kobayashi A, Sugito M, et al. Effectiveness of a transanal tube for the prevention of anastomotic leakage after rectal cancer surgery. World J Surg. 2014; 38:1843–1851.21. Matthiessen P, Hallbook O, Rutegard J, Simert G, Sjodahl R. Defunctioning stoma reduces symptomatic anastomotic leakage after low anterior resection of the rectum for cancer: a randomized multicenter trial. Ann Surg. 2007; 246:207–214.22. Huser N, Michalski CW, Erkan M, Schuster T, Rosenberg R, Kleeff J, et al. Systematic review and meta-analysis of the role of defunctioning stoma in low rectal cancer surgery. Ann Surg. 2008; 248:52–60.23. Shiomi A, Ito M, Saito N, Ohue M, Hirai T, Kubo Y, et al. Diverting stoma in rectal cancer surgery: a retrospective study of 329 patients from Japanese cancer centers. Int J Colorectal Dis. 2011; 26:79–87.24. Seo SI, Yu CS, Kim GS, Lee JL, Yoon YS, Kim CW, et al. The role of diverting stoma after an ultra-low anterior resection for rectal cancer. Ann Coloproctol. 2013; 29:66–71.25. Kaiser AM, Israelit S, Klaristenfeld D, Selvindoss P, Vukasin P, Ault G, et al. Morbidity of ostomy takedown. J Gastrointest Surg. 2008; 12:437–441.26. Koperna T. Cost-effectiveness of defunctioning stomas in low anterior resections for rectal cancer: a call for benchmarking. Arch Surg. 2003; 138:1334–1338.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Single port–assisted diverting ileostomy formation for anastomotic leakage after low anterior resection
- Optimal anastomotic technique in rectal surgery to prevent anastomotic leakage
- Analysis of Anastomotic Leakage after an Anterior Resection for Rectal Cancer
- Transanal gauze packing to manage massive presacral bleeding secondary to prescral abscess caused by rectal anastomotic leakage: a novel approach
- Risk Factors for Anastomotic Leakage after Laparoscopic Rectal Resection in Rectal Cancer: Does Laparoscopic Rectal Resection Increase Anastomotic Leakage Rate?