J Korean Neurosurg Soc.
2024 Jan;67(1):73-83. 10.3340/jkns.2023.0074.
Recent Trends in the Withdrawal of Life-Sustaining Treatment in Patients with Acute Cerebrovascular Disease : 2017–2021
- Affiliations
-
- 1Department of Neurosurgery, Samsung Changwon Hospital, Sungkyunkwan University School of Medicine, Changwon, Korea
- KMID: 2550461
- DOI: http://doi.org/10.3340/jkns.2023.0074
Abstract
Objective
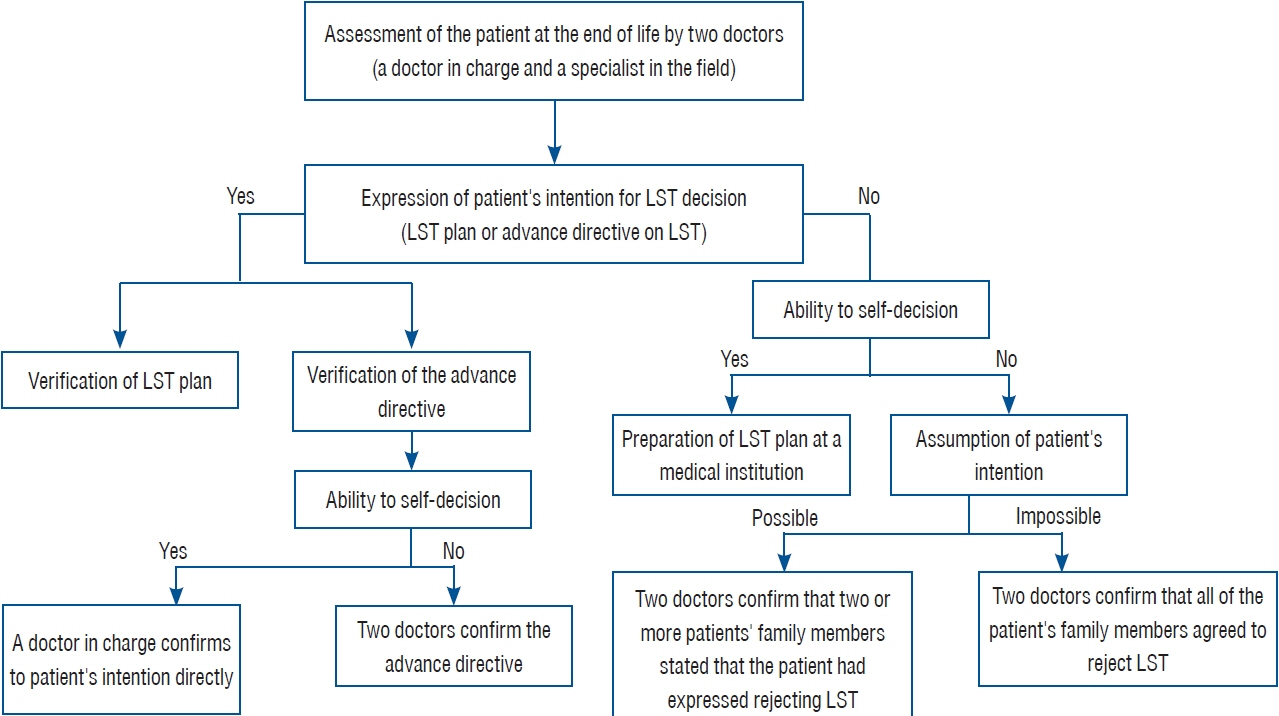
: The Act on Life-Sustaining Treatment (LST) decisions for end-of-life patients has been effective since February 2018. An increasing number of patients and their families want to withhold or withdraw from LST when medical futility is expected. This study aimed to investigate the status of the Act on LST decisions for patients with acute cerebrovascular disease at a single hospital.
Methods
: Between January 2017 and December 2021, 227 patients with acute cerebrovascular diseases, including hemorrhagic stroke (n=184) and ischemic stroke (n=43), died at the hospital. The study period was divided into the periods before and after the Act.
Results
: The duration of hospitalization decreased after the Act was implemented compared to before (15.9±16.1 vs. 11.2±18.6 days, p=0.127). The rate of obtaining consent for the LST plan tended to increase after the Act (139/183 [76.0%] vs. 27/44 [61.4%], p=0.077). Notably, none of the patients made an LST decision independently. Ventilator withdrawal was more frequently performed after the Act than before (52/183 [28.4%] vs. 0/44 [0%], p<0.001). Conversely, the rate of organ donation decreased after the Act was implemented (5/183 [2.7%] vs. 6/44 [13.6%], p=0.008). Refusal to undergo surgery was more common after the Act was implemented than before (87/149 [58.4%] vs. 15/41 [36.6%], p=0.021) among the 190 patients who required surgery.
Conclusion
: After the Act on LST decisions was implemented, the rate of LST withdrawal increased in patients with acute cerebrovascular disease. However, the decision to withdraw LST was made by the patient’s family rather than the patient themselves. After the execution of the Act, we also observed an increased rate of refusal to undergo surgery and a decreased rate of organ donation. The Act on LST decisions may reduce unnecessary treatments that prolong end-of-life processes without a curative effect. However, the widespread application of this law may also reduce beneficial treatments and contribute to a decline in organ donation.
Figure
Reference
-
References
1. Albrecht GL, Devlieger PJ. The disability paradox: high quality of life against all odds. Soc Sci Med. 48:977–988. 1999.
Article2. Alonso A, Ebert AD, Dörr D, Buchheidt D, Hennerici MG, Szabo K. Endof-life decisions in acute stroke patients: an observational cohort study. BMC Palliat Care. 15:38. 2016.
Article3. Becker KJ, Baxter AB, Cohen WA, Bybee HM, Tirschwell DL, Newell DW, et al. Withdrawal of support in intracerebral hemorrhage may lead to self-fulfilling prophecies. Neurology. 56:766–772. 2001.
Article4. Broderick JP, Brott TG, Duldner JE, Tomsick T, Huster G. Volume of intracerebral hemorrhage. A powerful and easy-to-use predictor of 30-day mortality. Stroke. 24:987–993. 1993.
Article5. Cheung RT, Zou LY. Use of the original, modified, or new intracerebral hemorrhage score to predict mortality and morbidity after intracerebral hemorrhage. Stroke. 34:1717–1722. 2003.
Article6. Choi Y, Park M, Kang DH, Lee J, Moon JY, Ahn H. The quality of dying and death for patients in intensive care units: a single center pilot study. Acute Crit Care. 34:192–201. 2019.
Article7. Christakis NA, Lamont EB. Extent and determinants of error in doctors’ prognoses in terminally ill patients: prospective cohort study. BMJ. 320:469–472. 2000.8. Cook D, Rocker G, Marshall J, Sjokvist P, Dodek P, Griffith L, et al. Withdrawal of mechanical ventilation in anticipation of death in the intensive care unit. N Engl J Med. 349:1123–1132. 2003.
Article9. Creutzfeldt CJ, Holloway RG. Treatment decisions after severe stroke: uncertainty and biases. Stroke. 43:3405–3408. 2012.10. Farooq S, Shkirkova K, Villablanca P, Sanossian N, Liebeskind DS, Starkman S, et al. National Institutes of Health Stroke scale correlates well with initial intracerebral hemorrhage volume. J Stroke Cerebrovasc Dis. 31:106348. 2022.
Article11. Friend JM, Alden DL. Improving patient preparedness and confidence in discussing advance directives for end-of-life care with health care providers in the United States and Japan. Med Decis Making. 41:60–73. 2021.
Article12. Gao L, Zhao CW, Hwang DY. End-of-life care decision-making in stroke. Front Neurol. 12:702833. 2021.
Article13. Graw JA, Marsch F, Spies CD, Francis RCE. End-of-life decision-making in intensive care ten years after a law on advance directives in Germany. Medicina (Kaunas). 57:930. 2021.
Article14. Hemphill JC 3rd, Bonovich DC, Besmertis L, Manley GT, Johnston SC. The ICH score: a simple, reliable grading scale for intracerebral hemorrhage. Stroke. 32:891–897. 2001.15. Heo DS, Yoo SH, Keam B, Yoo SH, Koh Y. Problems related to the act on decisions on life-sustaining treatment and directions for improvement. J Hosp Palliat Care. 25:1–11. 2022.
Article16. Holloway RG, Arnold RM, Creutzfeldt CJ, Lewis EF, Lutz BJ, McCann RM, et al. Palliative and end-of-life care in stroke: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 45:1887–1916. 2014.17. Jeong E, Baik S, Park H, Oh J, Lee Y, Lee JM. First organ donation after circulatory death following withdrawal of life-sustaining treatment in Korea: a case report. J Korean Med Sci. 36:e171. 2021.
Article18. Kelly AG, Hoskins KD, Holloway RG. Early stroke mortality, patient preferences, and the withdrawal of care bias. Neurology. 79:941–944. 2012.
Article19. Kim JS, Yoo SH, Choi W, Kim Y, Hong J, Kim MS, et al. Implication of the life-sustaining treatment decisions act on end-of-life care for korean terminal patients. Cancer Res Treat. 52:917–924. 2020.
Article20. Kim S, Lim A, Jang H, Jeon M. Life-sustaining treatment decision in palliative care based on electronic health records analysis. J Clin Nurs. 32:163–173. 2023.
Article21. Kim YJ, Lim CM, Shim TS, Hong SB, Huh JW, Oh DK, et al. The influence of new legislation on the withdrawal of life-sustaining treatment on the perceptions and experiences of residents in a tertiary hospital in Korea. Korean J Med Ethics. 23:279–299. 2020.22. Klein A, Kuehner C, Schwarz S. Attitudes in the general population towards hemi-craniectomy for middle cerebral artery (MCA) infarction. A population-based survey. Neurocrit Care. 16:456–461. 2012.
Article23. Korean Organ Donation Agency : Donation trends over the years. Available at : https://www.koda1458.kr/info/trend.do.24. Lahti AM, Nätynki M, Huhtakangas J, Bode M, Juvela S, Ohtonen P, et al. Long-term survival after primary intracerebral hemorrhage: a population-based case-control study spanning a quarter of a century. Eur J Neurol. 28:3663–3669. 2021.
Article25. Lee HY, Kim HJ, Kwon JH, Baek SK, Won YW, Kim YJ, et al. The situation of life-sustaining treatment one year after enforcement of the act on decisions on life-sustaining treatment for patients at the end-oflife in Korea: data of national agency for management of life-sustaining treatment. Cancer Res Treat. 53:897–907. 2021.
Article26. Lee SH, Kim JM, Yeo Y, Kim J. The impact of the well-dying law in Korea: comparing clinical characteristics and ICU admissions. Ann Palliat Med. 11:3135–3146. 2022.
Article27. Lee YJ, Ahn S, Cho JY, Park TY, Yun SY, Kim J, et al. Change in perception of the quality of death in the intensive care unit by healthcare workers associated with the implementation of the “well-dying law”. Intensive Care Med. 48:281–289. 2022.
Article28. Lomero M, Gardiner D, Coll E, Haase-Kromwijk B, Procaccio F, Immer F, et al. Donation after circulatory death today: an updated overview of the European landscape. Transpl Int. 33:76–88. 2020.
Article29. Maas MB, Francis BA, Sangha RS, Lizza BD, Liotta EM, Naidech AM. Refining prognosis for intracerebral hemorrhage by early reassessment. Cerebrovasc Dis. 43:110–116. 2017.
Article30. Meadow W, Pohlman A, Frain L, Ren Y, Kress JP, Teuteberg W, et al. Power and limitations of daily prognostications of death in the medical intensive care unit. Crit Care Med. 39:474–479. 2011.
Article31. National Agent for Management of Life-Sustaining Treatment : Monthly Statistics. Available at : https://www.lst.go.kr/comm/monthlyStatistics.do.32. National Law Information Center : Hospice and Palliative Care and Life-Sustaining Treatment for patients at the end-of-life. Available at : https://law.go.kr/LSW/lsInfoP.do?lsiSeq=180823&viewCls=engLsInfoR&urlMode=engLsInfoR#0000.33. Navi BB, Kamel H, McCulloch CE, Nakagawa K, Naravetla B, Moheet AM, et al. Accuracy of neurovascular fellows’ prognostication of outcome after subarachnoid hemorrhage. Stroke. 43:702–707. 2012.
Article34. Park H, Jung ES, Oh JS, Lee YM, Lee JM. Organ donation after controlled circulatory death (Maastricht classification III) following the withdrawal of life-sustaining treatment in Korea: a suggested guideline. Korean J Transplant. 35:71–76. 2021.
Article35. Park J, Kim CJ. Recent decrease in organ donation from brain-dead potential organ donors in Korea and possible causes. J Korean Med Sci. 35:e94. 2020.
Article36. Park SY, Lee B, Seon JY, Oh IH. A national study of life-sustaining treatments in South Korea: what factors affect decision-making? Cancer Res Treat. 53:593–600. 2021.
Article37. Rosen DS, Macdonald RL. Subarachnoid hemorrhage grading scales: a systematic review. Neurocrit Care. 2:110–118. 2005.
Article38. Saposnik G, Cote R, Mamdani M, Raptis S, Thorpe KE, Fang J, et al. JURaSSiC: accuracy of clinician vs risk score prediction of ischemic stroke outcomes. Neurology. 81:448–455. 2013.39. Saposnik G, Kapral MK, Liu Y, Hall R, O’Donnell M, Raptis S, et al. IScore: a risk score to predict death early after hospitalization for an acute ischemic stroke. Circulation. 123:739–749. 2011.40. Smith EE, Shobha N, Dai D, Olson DM, Reeves MJ, Saver JL, et al. A risk score for in-hospital death in patients admitted with ischemic or hemorrhagic stroke. J Am Heart Assoc. 2:e005207. 2013.
Article41. Son YJ, Choi J, Ahn JW. Nurses’ perspectives on advance directives before the establishment of the new well-dying law in Korea: a mixed methods study. Appl Nurs Res. 51:151187. 2020.
Article42. Souter MJ, Blissitt PA, Blosser S, Bonomo J, Greer D, Jichici D, et al. Recommendations for the critical care management of devastating brain injury: prognostication, psychosocial, and ethical management : a position statement for healthcare professionals from the Neurocritical Care Society. Neurocrit Care. 23:4–13. 2015.
Article43. Tanaka M, Kodama S, Lee I, Huxtable R, Chung Y. Forgoing life-sustaining treatment - a comparative analysis of regulations in Japan, Korea, Taiwan, and England. BMC Med Ethics. 21:99. 2020.
Article44. Turnbull AE, Ning X, Rao A, Tao JJ, Needham DM. Demonstrating the impact of POLST forms on hospital care requires information not contained in state registries. PLoS One. 14:e0217113. 2019.
Article45. Vahedi K, Benoist L, Kurtz A, Mateo J, Blanquet A, Rossignol M, et al. Quality of life after decompressive craniectomy for malignant middle cerebral artery infarction. J Neurol Neurosurg Psychiatry. 76:1181–1182. 2005.
Article46. Vranas KC, Plinke W, Bourne D, Kansagara D, Lee RY, Kross EK, et al. The influence of POLST on treatment intensity at the end of life: a systematic review. J Am Geriatr Soc. 69:3661–3674. 2021.
Article47. Wang Y, Zhang Y, Hong Y, Zeng P, Hu Z, Xu X, et al. Advance directives and end-of-life care: knowledge and preferences of patients with brain tumours from Anhui, China. BMC Cancer. 21:25. 2021.
Article48. Won YW, Kim HJ, Kwon JH, Lee HY, Baek SK, Kim YJ, et al. Lifesustaining treatment states in Korean cancer patients after enforcement of act on decisions on life-sustaining treatment for patients at the end of life. Cancer Res Treat. 53:908–916. 2021.
Article49. Yen YF, Huang LY, Hu HY, Sun WJ, Ko MC, Lee YL, et al. Association of advance directives completion with the utilization of life-sustaining treatments during the end-of-life care in older patients. J Pain Symptom Manage. 55:265–271. 2018.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Awareness of Nursing Students' Biomedical Ethics and Attitudes toward Withdrawal of Life-Sustaining Treatment
- Mediating Effects of Role Perception of Life-sustaining Treatment in the Relationship between Knowledge of Lifesustaining Treatment Plans and Attitudes toward Withdrawal of Life-sustaining Treatment among Nursing College Students
- The Effects of Nurses’ Knowledge of Withdrawal of LifeSustaining Treatment, Death Anxiety, Perceptions of Hospice on Their Attitudes toward Withdrawal of Life-Sustaining Treatment
- The Relationship among Attitudes toward the Withdrawal of Life-sustaining Treatment, Death Anxiety, and Death Acceptance among Hospitalized Elderly Cancer Patients
- Withdrawal of Life-Sustaining Treatment from Children: Experiences of Nurses Caring for the Children