Kosin Med J.
2023 Dec;38(4):231-240. 10.7180/kmj.23.141.
Prevention of myopia progression using orthokeratology
- Affiliations
-
- 1Department of Ophthalmology, University of California, Los Angeles, Los Angeles, CA, USA
- 2Stein Eye Institute, University of California, Los Angeles, Los Angeles, CA, USA
- 3Department of Ophthalmology, Kosin University College of Medicine, Busan, Korea
- KMID: 2549495
- DOI: http://doi.org/10.7180/kmj.23.141
Abstract
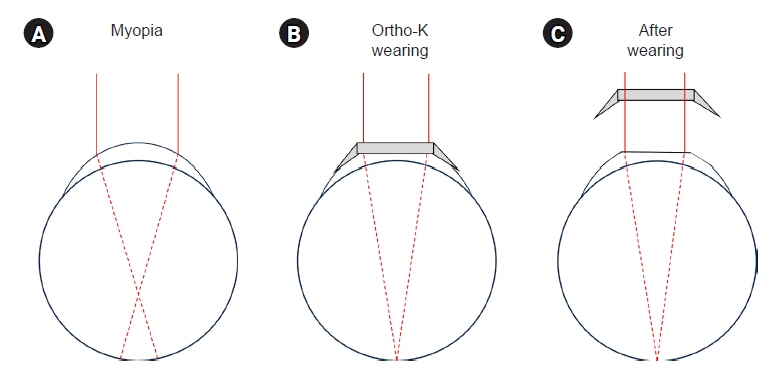
- The prevalence of myopia in children and juveniles has increased significantly in Korea and worldwide; in particular, the rates of myopia and high myopia in East Asia have grown rapidly. Myopia is easily corrected with spectacles or contact lenses. However, as children grow and mature, myopia can progress irreversibly and lead to vision-threatening complications. Thus, the prevention of myopia progression is an essential treatment goal. Many treatment strategies are being employed, including atropine eyedrops, specialized glasses, and orthokeratology (Ortho-K) lenses. Ortho-K is an effective treatment in managing myopia progression by lowering the rate of increase in refractive error and axial length. In this article, we review Ortho-K as a treatment for myopia progression, its history, mechanism, treatment regimen, and safety profile.
Figure
Reference
-
References
1. Magnus H. The knowledge of visual disturbances among the Greeks and Romans. Graefes Arch Clin Exp Ophthalmol. 1877; 23:24–48.2. Hirschberg J. Geschichte der Augenheilkunde. Springer;1899.3. Kang G, Kim SE. How to write an original article in medicine and medical science. Kosin Med J. 2022; 37:96–101.4. Tsai TH, Liu YL, Ma IH, Su CC, Lin CW, Lin LL, et al. Evolution of the prevalence of myopia among taiwanese schoolchildren: a review of survey data from 1983 through 2017. Ophthalmology. 2021; 128:290–301.5. Rim TH, Kim SH, Lim KH, Choi M, Kim HY, Baek SH, et al. Refractive errors in Koreans: the Korea National Health and Nutrition Examination Survey 2008-2012. Korean J Ophthalmol. 2016; 30:214–24.6. Wu LJ, You QS, Duan JL, Luo YX, Liu LJ, Li X, et al. Prevalence and associated factors of myopia in high-school students in Beijing. PLoS One. 2015; 10:e0120764.7. Prabakaran S, Dirani M, Chia A, Gazzard G, Fan Q, Leo SW, et al. Cycloplegic refraction in preschool children: comparisons between the hand-held autorefractor, table-mounted autorefractor and retinoscopy. Ophthalmic Physiol Opt. 2009; 29:422–6.8. Wen G, Tarczy-Hornoch K, McKean-Cowdin R, Cotter SA, Borchert M, Lin J, et al. Prevalence of myopia, hyperopia, and astigmatism in non-Hispanic white and Asian children: multi-ethnic pediatric eye disease study. Ophthalmology. 2013; 120:2109–16.9. Holden BA, Jong M, Davis S, Wilson D, Fricke T, Resnikoff S. Nearly 1 billion myopes at risk of myopia-related sight-threatening conditions by 2050 - time to act now. Clin Exp Optom. 2015; 98:491–3.10. Saw SM, Tong L, Chua WH, Chia KS, Koh D, Tan DT, et al. Incidence and progression of myopia in Singaporean school children. Invest Ophthalmol Vis Sci. 2005; 46:51–7.11. Mutti DO, Mitchell GL, Jones LA, Friedman NE, Frane SL, Lin WK, et al. Axial growth and changes in lenticular and corneal power during emmetropization in infants. Invest Ophthalmol Vis Sci. 2005; 46:3074–80.12. Gordon RA, Donzis PB. Refractive development of the human eye. Arch Ophthalmol. 1985; 103:785–9.13. Baird PN, Saw SM, Lanca C, Guggenheim JA, Smith Iii EL, Zhou X, et al. Myopia. Nat Rev Dis Primers. 2020; 6:99.14. Benavente-Perez A, Nour A, Troilo D. Axial eye growth and refractive error development can be modified by exposing the peripheral retina to relative myopic or hyperopic defocus. Invest Ophthalmol Vis Sci. 2014; 55:6765–73.15. Bez D, Megreli J, Bez M, Avramovich E, Barak A, Levine H. Association between type of educational system and prevalence and severity of myopia among male adolescents in Israel. JAMA Ophthalmol. 2019; 137:887–93.16. Guggenheim JA, Northstone K, McMahon G, Ness AR, Deere K, Mattocks C, et al. Time outdoors and physical activity as predictors of incident myopia in childhood: a prospective cohort study. Invest Ophthalmol Vis Sci. 2012; 53:2856–65.17. Vitale S, Ellwein L, Cotch MF, Ferris FL 3rd, Sperduto R. Prevalence of refractive error in the United States, 1999-2004. Arch Ophthalmol. 2008; 126:1111–9.18. Yusufu M, Wang N. How China is responding to the challenge of myopia. Community Eye Health. 2021; 34:76.19. Zhu Z, Chen Y, Tan Z, Xiong R, McGuinness MB, Muller A. Interventions recommended for myopia prevention and control among children and adolescents in China: a systematic review. Br J Ophthalmol. 2023; 107:160–6.20. Baird PN, Schache M, Dirani M. The GEnes in Myopia (GEM) study in understanding the aetiology of refractive errors. Prog Retin Eye Res. 2010; 29:520–42.21. Tedja MS, Haarman AE, Meester-Smoor MA, Kaprio J, Mackey DA, Guggenheim JA, et al. IMI: myopia genetics report. Invest Ophthalmol Vis Sci. 2019; 60:M89–105.22. Chen YP, Hocking PM, Wang L, Povazay B, Prashar A, To CH, et al. Selective breeding for susceptibility to myopia reveals a gene-environment interaction. Invest Ophthalmol Vis Sci. 2011; 52:4003–11.23. Lee SJ, Ahn KS, Yu BC. Determining factors of myopic refractive error in 19 years old men. Kosin Med J. 2008; 23:66–71.24. Jones-Jordan LA, Sinnott LT, Chu RH, Cotter SA, Kleinstein RN, Manny RE, et al. Myopia progression as a function of sex, age, and ethnicity. Invest Ophthalmol Vis Sci. 2021; 62:36.25. Tricard D, Marillet S, Ingrand P, Bullimore MA, Bourne RRA, Leveziel N. Progression of myopia in children and teenagers: a nationwide longitudinal study. Br J Ophthalmol. 2022; 106:1104–9.26. Jones LA, Mitchell GL, Mutti DO, Hayes JR, Moeschberger ML, Zadnik K. Comparison of ocular component growth curves among refractive error groups in children. Invest Ophthalmol Vis Sci. 2005; 46:2317–27.27. Han X, Guo X, Lee PY, Morgan IG, He M. Six-year changes in refraction and related ocular biometric factors in an adult Chinese population. PLoS One. 2017; 12:e0183364.28. Cooper J, Tkatchenko AV. A review of current concepts of the etiology and treatment of myopia. Eye Contact Lens. 2018; 44:231–47.29. Irving EL, Callender MG, Sivak JG. Inducing myopia, hyperopia, and astigmatism in chicks. Optom Vis Sci. 1991; 68:364–8.30. Mandell RB. Myopia control with bifocal correction. Am J Optom Arch Am Acad Optom. 1959; 36:652–8.31. Fulk GW, Cyert LA, Parker DE. A randomized trial of the effect of single-vision vs. bifocal lenses on myopia progression in children with esophoria. Optom Vis Sci. 2000; 77:395–401.32. Leung JT, Brown B. Progression of myopia in Hong Kong Chinese schoolchildren is slowed by wearing progressive lenses. Optom Vis Sci. 1999; 76:346–54.33. Goss DA. Variables related to the rate of childhood myopia progression. Optom Vis Sci. 1990; 67:631–6.34. Gwiazda J, Thorn F, Held R. Accommodation, accommodative convergence, and response AC/A ratios before and at the onset of myopia in children. Optom Vis Sci. 2005; 82:273–8.35. Sankaridurg P, Donovan L, Varnas S, Ho A, Chen X, Martinez A, et al. Spectacle lenses designed to reduce progression of myopia: 12-month results. Optom Vis Sci. 2010; 87:631–41.36. Edwards MH, Li RW, Lam CS, Lew JK, Yu BS. The Hong Kong progressive lens myopia control study: study design and main findings. Invest Ophthalmol Vis Sci. 2002; 43:2852–8.37. Bedrossian RH. The effect of atropine on myopia. Ann Ophthalmol. 1971; 3:891–7.38. Chia A, Lu QS, Tan D. Five-year clinical trial on atropine for the treatment of myopia 2: myopia control with atropine 0.01% eyedrops. Ophthalmology. 2016; 123:391–9.39. Chua WH, Balakrishnan V, Chan YH, Tong L, Ling Y, Quah BL, et al. Atropine for the treatment of childhood myopia. Ophthalmology. 2006; 113:2285–91.40. Chia A, Chua WH, Cheung YB, Wong WL, Lingham A, Fong A, et al. Atropine for the treatment of childhood myopia: safety and efficacy of 0.5%, 0.1%, and 0.01% doses (Atropine for the Treatment of Myopia 2). Ophthalmology. 2012; 119:347–54.41. Gallego P, Martinez-Garcia C, Perez-Merino P, Ibares-Frias L, Mayo-Iscar A, Merayo-Lloves J. Scleral changes induced by atropine in chicks as an experimental model of myopia. Ophthalmic Physiol Opt. 2012; 32:478–84.42. Wildsoet CF, Chia A, Cho P, Guggenheim JA, Polling JR, Read S, et al. IMI - Interventions myopia institute: interventions for controlling myopia onset and progression report. Invest Ophthalmol Vis Sci. 2019; 60:M106–31.43. Gong Q, Janowski M, Luo M, Wei H, Chen B, Yang G, et al. Efficacy and adverse effects of atropine in childhood myopia: a meta-analysis. JAMA Ophthalmol. 2017; 135:624–30.44. Rose KA, Morgan IG, Ip J, Kifley A, Huynh S, Smith W, et al. Outdoor activity reduces the prevalence of myopia in children. Ophthalmology. 2008; 115:1279–85.45. He M, Xiang F, Zeng Y, Mai J, Chen Q, Zhang J, et al. Effect of time spent outdoors at school on the development of myopia among children in China: a randomized clinical trial. JAMA. 2015; 314:1142–8.46. Mutti DO, Marks AR. Blood levels of vitamin D in teens and young adults with myopia. Optom Vis Sci. 2011; 88:377–82.47. Zhou X, Pardue MT, Iuvone PM, Qu J. Dopamine signaling and myopia development: what are the key challenges. Prog Retin Eye Res. 2017; 61:60–71.48. Rose KA, French AN, Morgan IG. Environmental factors and myopia: paradoxes and prospects for prevention. Asia Pac J Ophthalmol (Phila). 2016; 5:403–10.49. Sherwin JC, Reacher MH, Keogh RH, Khawaja AP, Mackey DA, Foster PJ. The association between time spent outdoors and myopia in children and adolescents: a systematic review and meta-analysis. Ophthalmology. 2012; 119:2141–51.50. Cheng D, Woo GC, Drobe B, Schmid KL. Effect of bifocal and prismatic bifocal spectacles on myopia progression in children: three-year results of a randomized clinical trial. JAMA Ophthalmol. 2014; 132:258–64.51. Gwiazda J, Hyman L, Hussein M, Everett D, Norton TT, Kurtz D, et al. A randomized clinical trial of progressive addition lenses versus single vision lenses on the progression of myopia in children. Invest Ophthalmol Vis Sci. 2003; 44:1492–500.52. Cho P, Cheung SW. Retardation of Myopia in Orthokeratology (ROMIO) study: a 2-year randomized clinical trial. Invest Ophthalmol Vis Sci. 2012; 53:7077–85.53. Walline JJ, Walker MK, Mutti DO, Jones-Jordan LA, Sinnott LT, Giannoni AG, et al. Effect of high add power, medium add power, or single-vision contact lenses on myopia progression in children: the BLINK Randomized Clinical Trial. JAMA. 2020; 324:571–80.54. Berntsen DA, Sinnott LT, Mutti DO, Zadnik K. A randomized trial using progressive addition lenses to evaluate theories of myopia progression in children with a high lag of accommodation. Invest Ophthalmol Vis Sci. 2012; 53:640–9.55. Swarbrick HA. Orthokeratology review and update. Clin Exp Optom. 2006; 89:124–43.56. Jessen GN. Contact lenses as a therapeutic device. Am J Optom Arch Am Acad Optom. 1964; 41:429–35.57. Lui WO, Edwards MH, Cho P. Contact lenses in myopia reduction: from orthofocus to accelerated orthokeratology. Cont Lens Anterior Eye. 2000; 23:68–76.58. Nti AN, Berntsen DA. Optical changes and visual performance with orthokeratology. Clin Exp Optom. 2020; 103:44–54.59. Charm J. Orthokeratology: clinical utility and patient perspectives. Clin Optom (Auckl). 2017; 9:33–40.60. Lipson MJ, Brooks MM, Koffler BH. The role of orthokeratology in myopia control: a review. Eye Contact Lens. 2018; 44:224–30.61. Swarbrick HA, Alharbi A, Watt K, Lum E, Kang P. Myopia control during orthokeratology lens wear in children using a novel study design. Ophthalmology. 2015; 122:620–30.62. Cho P, Tan Q. Myopia and orthokeratology for myopia control. Clin Exp Optom. 2019; 102:364–77.63. Vincent SJ, Cho P, Chan KY, Fadel D, Ghorbani-Mojarrad N, Gonzalez-Meijome JM, et al. CLEAR: orthokeratology. Cont Lens Anterior Eye. 2021; 44:240–69.64. Wu J, Fang W, Xu H, Liu X, Zhao D, Rong Q. The biomechanical response of the cornea in orthokeratology. Front Bioeng Biotechnol. 2021; 9:743745.65. Kim SJ, Lee JE. Influence of orthokeratology lens on axial length elongation and myopic progression in childhood myopia. Kosin Med J. 2017; 32:204–11.66. Smith EL 3rd, Hung LF, Huang J. Relative peripheral hyperopic defocus alters central refractive development in infant monkeys. Vision Res. 2009; 49:2386–92.67. Irving EL, Callender MG, Sivak JG. Inducing ametropias in hatchling chicks by defocus: aperture effects and cylindrical lenses. Vision Res. 1995; 35:1165–74.68. Mutti DO, Sholtz RI, Friedman NE, Zadnik K. Peripheral refraction and ocular shape in children. Invest Ophthalmol Vis Sci. 2000; 41:1022–30.69. Lumb E, Sulley A, Logan NS, Jones D, Chamberlain P. Six years of wearer experience in children participating in a myopia control study of MiSight® 1 day. Cont Lens Anterior Eye. 2023; 46:101849.70. Karimian F, Feizi S, Doozande A. Higher-order aberrations in myopic eyes. J Ophthalmic Vis Res. 2010; 5:3–9.71. Hiraoka T, Kotsuka J, Kakita T, Okamoto F, Oshika T. Relationship between higher-order wavefront aberrations and natural progression of myopia in schoolchildren. Sci Rep. 2017; 7:7876.72. Lau JK, Vincent SJ, Collins MJ, Cheung SW, Cho P. Ocular higher-order aberrations and axial eye growth in young Hong Kong children. Sci Rep. 2018; 8:6726.73. Gifford P, Li M, Lu H, Miu J, Panjaya M, Swarbrick HA. Corneal versus ocular aberrations after overnight orthokeratology. Optom Vis Sci. 2013; 90:439–47.74. Allen PM, Radhakrishnan H, Rae S, Calver RI, Theagarayan BP, Nelson P, et al. Aberration control and vision training as an effective means of improving accommodation in individuals with myopia. Invest Ophthalmol Vis Sci. 2009; 50:5120–9.75. Summers JA. The choroid as a sclera growth regulator. Exp Eye Res. 2013; 114:120–7.76. Felipe-Marquez G, Nombela-Palomo M, Cacho I, Nieto-Bona A. Accommodative changes produced in response to overnight orthokeratology. Graefes Arch Clin Exp Ophthalmol. 2015; 253:619–26.77. Chen Z, Xue F, Zhou J, Qu X, Zhou X. Effects of orthokeratology on choroidal thickness and axial length. Optom Vis Sci. 2016; 93:1064–71.78. Li Z, Cui D, Hu Y, Ao S, Zeng J, Yang X. Choroidal thickness and axial length changes in myopic children treated with orthokeratology. Cont Lens Anterior Eye. 2017; 40:417–23.79. Cho P, Cheung SW. Discontinuation of orthokeratology on eyeball elongation (DOEE). Cont Lens Anterior Eye. 2017; 40:82–7.80. Wang M, Cui C, Sui Y, Yu SA, Ma JX, Fu AC. Effect of 0.02% and 0.01% atropine on astigmatism: a two-year clinical trial. BMC Ophthalmol. 2022; 22:161.81. VanderVeen DK, Kraker RT, Pineles SL, Hutchinson AK, Wilson LB, Galvin JA, et al. Use of orthokeratology for the prevention of myopic progression in children: a report by the American Academy of Ophthalmology. Ophthalmology. 2019; 126:623–36.82. Cho P, Cheung SW, Edwards M. The longitudinal orthokeratology research in children (LORIC) in Hong Kong: a pilot study on refractive changes and myopic control. Curr Eye Res. 2005; 30:71–80.83. Liu YM, Xie P. The safety of orthokeratology: a systematic review. Eye Contact Lens. 2016; 42:35–42.84. Santodomingo-Rubido J. Foreword: orthokeratology for myopia control in everyday practice. Cont Lens Anterior Eye. 2023; 46:101798.85. Kam KW, Yung W, Li GK, Chen LJ, Young AL. Infectious keratitis and orthokeratology lens use: a systematic review. Infection. 2017; 45:727–35.86. Watt KG, Swarbrick HA. Trends in microbial keratitis associated with orthokeratology. Eye Contact Lens. 2007; 33(6 Pt 2):373–82.87. Chan B, Cho P, Cheung SW. Orthokeratology practice in children in a university clinic in Hong Kong. Clin Exp Optom. 2008; 91:453–60.88. Cho P, Chui WS, Mountford J, Cheung SW. Corneal iron ring associated with orthokeratology lens wear. Optom Vis Sci. 2002; 79:565–8.89. Cho P, Chui WS, Cheung SW. Reversibility of corneal pigmented arc associated with orthokeratology. Optom Vis Sci. 2003; 80:791–5.90. Gonzalez-Meijome JM, Gonzalez-Perez J, Garcia-Porta N, Diaz-Rey A, Parafita-Mato MA. Pigmented corneal ring associated with orthokeratology in Caucasians: case reports. Clin Exp Optom. 2012; 95:548–52.91. Sun L, Li ZX, Chen Y, He ZQ, Song HX. The effect of orthokeratology treatment zone decentration on myopia progression. BMC Ophthalmol. 2022; 22:76.92. Gispets J, Yebana P, Lupon N, Cardona G, Perez-Corral J, Paune J, et al. Efficacy, predictability and safety of long-term orthokeratology: an 18-year follow-up study. Cont Lens Anterior Eye. 2022; 45:101530.93. Lo J, Kuo MT, Chien CC, Tseng SL, Lai YH, Fang PC. Microbial bioburden of orthokeratology contact lens care system. Eye Contact Lens. 2016; 42:61–7.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Characteristics of Prescribing Orthokeratology Lenses in Adult
- Comparison of Myopic Progression before and after Orthokeratology Lens Treatment
- Prescription and effect of orthokeratology lenses
- The Inhibitory Effect of Myopic and Astigmatic Progression by Orthokeratology Lens
- Influence of Orthokeratology Lens on Axial length Elongation and Myopic Progression in Childhood Myopia