J Neurocrit Care.
2023 Dec;16(2):115-118. 10.18700/jnc.230043.
Lateral medullary infarction in a patient with Moyamoya disease associated with RNF213 variants: a case report
- Affiliations
-
- 1Department of Neurology, CHA Bundang Medical Center, CHA University School of Medicine, Seongnam, Korea
- KMID: 2549490
- DOI: http://doi.org/10.18700/jnc.230043
Abstract
- Background
Moyamoya disease (MMD) is a rare cerebrovascular disease radiologically characterized by progressive bilateral occlusion of the distal portion of the internal carotid artery and compensating collaterals. Herein, we report a case of medullary infarction in a patient with MMD.
Case Report
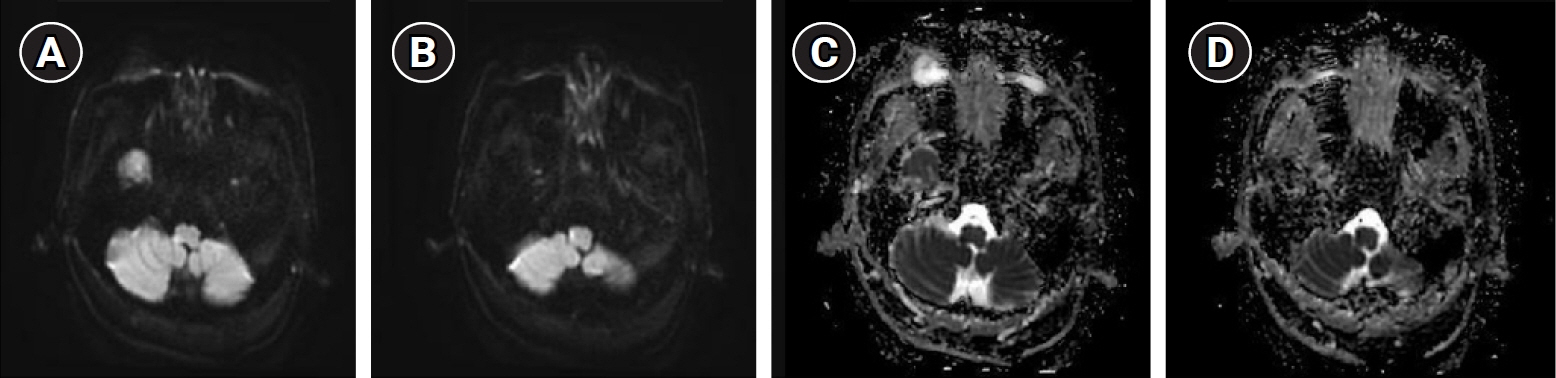
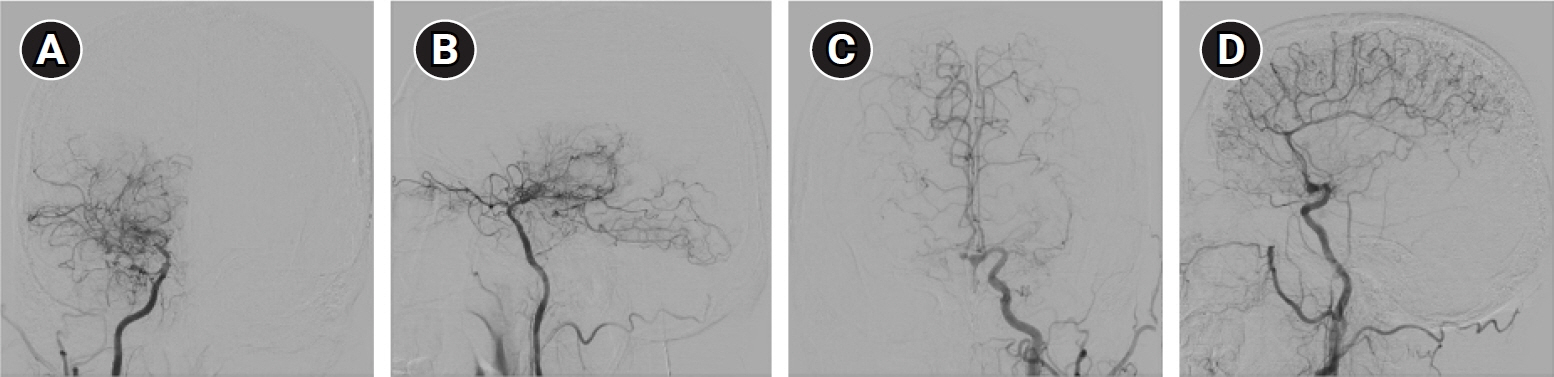
We present the case of a 54-year-old male with hypertension, hyperlipidemia, and unstable angina with sudden onset dysarthria and ataxia. Diffusion-weighted and T2-weighted images of magnetic resonance imaging showed a high-signal intensity lesion on the right lateral medulla, suggestive of acute infarction. Transfemoral cerebral angiography also demonstrated bilateral middle cerebral artery (MCA) occlusion. Testing of the ring finger protein 213 (RNF213) gene revealed a homozygous p.R4810K variant that was possibly associated with posterior circulation involvement.
Conclusion
When the MCA is occluded in MMD, there is a possibility that medullary infarction may occur due to the mechanism of increased hemodynamic stress on the anastomotic posterior vessels.
Figure
Reference
-
1. Suzuki J, Kodama N. Moyamoya disease: a review. Stroke. 1983; 14:104–9.2. Scott RM, Smith ER. Moyamoya disease and moyamoya syndrome. N Engl J Med. 2009; 360:1226–37.3. Mugikura S, Higano S, Shirane R, Fujimura M, Shimanuki Y, Takahashi S. Posterior circulation and high prevalence of ischemic stroke among young pediatric patients with Moyamoya disease: evidence of angiography-based differences by age at diagnosis. AJNR Am J Neuroradiol. 2011; 32:192–8.4. Funaki T, Takahashi JC, Takagi Y, Yoshida K, Araki Y, Kikuchi T, et al. Impact of posterior cerebral artery involvement on long-term clinical and social outcome of pediatric moyamoya disease. J Neurosurg Pediatr. 2013; 12:626–32.5. Kuroda S, Fujimura M, Takahashi J, Kataoka H, Ogasawara K, Iwama T, et al. Diagnostic criteria for Moyamoya disease: 2021 revised version. Neurol Med Chir (Tokyo). 2022; 62:307–12.6. Ihara M, Yamamoto Y, Hattori Y, Liu W, Kobayashi H, Ishiyama H, et al. Moyamoya disease: diagnosis and interventions. Lancet Neurol. 2022; 21:747–58.7. Jang MA, Shin S, Yoon JH, Ki CS. Frequency of the moyamoya-related RNF213 p.Arg4810Lys variant in 1,516 Korean individuals. BMC Med Genet. 2015; 16:109.8. Kim JE, Jeon JS. An update on the diagnosis and treatment of adult Moyamoya disease taking into consideration controversial issues. Neurol Res. 2014; 36:407–16.9. Kim WH, Kim SD, Nam MH, Jung JM, Jin SW, Ha SK, et al. Posterior circulation involvement and collateral flow pattern in moyamoya disease with the RNF213 polymorphism. Childs Nerv Syst. 2019; 35:309–14.10. Miyatake S, Miyake N, Touho H, Nishimura-Tadaki A, Kondo Y, Okada I, et al. Homozygous c.14576G>A variant of RNF213 predicts early-onset and severe form of moyamoya disease. Neurology. 2012; 78:803–10.11. Kim JS, Lee JH, Choi CG. Patterns of lateral medullary infarction: vascular lesion-magnetic resonance imaging correlation of 34 cases. Stroke. 1998; 29:645–52.12. Kinoshita Y, Kohshi K, Yokota A. Moyamoya disease of adult onset brain stem haemorrhage associated with bilateral occlusion of the vertebral arteries: case report. Acta Neurochir (Wien). 1998; 140:181–4.13. Tan C, Duan R, Ye X, Zhang D, Wang R. Posterior circulation Moyamoya disease versus primitive vertebral-basilar artery system Moyamoya disease: new classification of Moyamoya disease from the perspective of embryology. World Neurosurg. 2016; 96:222–9.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Isolated Axial Lateropulsion in Lateral Medullary Infarction
- Systemic vasculopathy associated with an RNF213 p.Arg4810Lys variant in moyamoya disease: A review
- Genetics and Biomarkers of Moyamoya Disease: Significance of RNF213 as a Susceptibility Gene
- A Case of Lateral Medullary Syndrome with Ipsilesional Nystagmus due to Intramedullary Hemorrhage
- Opalski Syndrome Presenting as Sensorimotor Deficits Ipsilateral to Cerebral Infarction