J Neurocrit Care.
2023 Dec;16(2):111-114. 10.18700/jnc.230028.
Group B Streptococcus meningitis following subarachnoid hemorrhage suspicions: a case report
- Affiliations
-
- 1Department Anesthesiology and Perioperative Medicine, Virginia Commonwealth University School of Medicine, Richmond, VA, USA
- KMID: 2549489
- DOI: http://doi.org/10.18700/jnc.230028
Abstract
- Background
Bacterial meningitis is a life-threatening disease associated with high morbidity and mortality. Subarachnoid hemorrhage (SAH) can accompany bacterial meningitis in adult patients in <1% of cases and significantly worsens the patient’s prognosis.
Case report
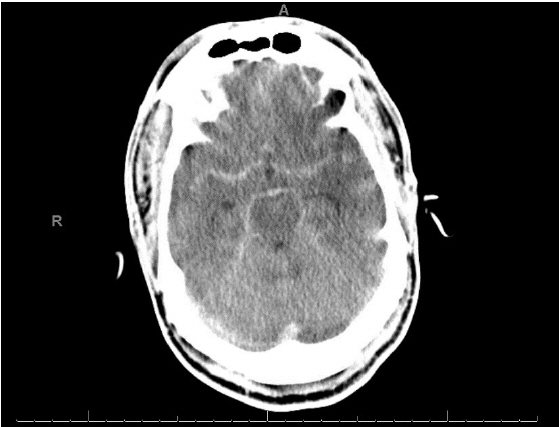
A 58-year-old man presented to the emergency department complaining of a 5-day history of progressive abdominal pain, when he suddenly developed “the worst headache of his life” and suffered a 4-minute seizure. Computed tomography head showed SAH. An emergent cerebral angiogram was negative for any bleeding source, and attention shifted to meningoencephalitis. Ultimately, the patient was found to have Group B Streptococcus (GBS) meningitis on cerebrospinal fluid polymerase chain reaction.
Conclusion
To the best of our knowledge, this patient’s presentation of GBS meningitis, masked by a classic aneurysmal SAH presentation, represents a rare and acute presentation of an underlying disease complication. Increasing awareness of this presentation can support more rapid diagnosis, earlier treatment, and improved outcomes for affected patients.
Keyword
Figure
Reference
-
1. van de Beek D, Brouwer MC, Koedel U, Wall EC. Community-acquired bacterial meningitis. Lancet. 2021; 398:1171–83.2. Al-Bayati A, Douedi S, Alsaoudi G, Mosseri M, Albustani S, Upadhyaya V, et al. Meningitis from invasive Streptococcus agalactiae in a healthy young adult. IDCases. 2020; 21:e00907.3. Deliran SS, Brouwer MC, van de Beek D. Subarachnoid hemorrhage in bacterial meningitis patients. Cerebrovasc Dis. 2022; 51:118–24.4. Kannoth S, Iyer R, Thomas SV, Furtado SV, Rajesh BJ, Kesavadas C, et al. Intracranial infectious aneurysm: presentation, management and outcome. J Neurol Sci. 2007; 256:3–9.5. Mook-Kanamori BB, Fritz D, Brouwer MC, van der Ende A, van de Beek D. Intracerebral hemorrhages in adults with community associated bacterial meningitis in adults: should we reconsider anticoagulant therapy? PLoS One. 2012; 7:e45271.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Intracerebral Thrombosis and Cortical Hemorrhage Complicated by Streptococcus pneumoniae Meningitis
- Streptococcus viridans Meningitis After Epidural Nerve Block
- Two Cases of Cerebral Infarctions Complicated by Streptococcus pneumoniae Meningitis
- A Case of Bilateral Endogenous Endophthalmitis in a Streptococcus pneumoniae Meningitis Patient
- Spontaneous Spinal Subarachnoid Hemorrhage Report of a Case