Ann Pediatr Endocrinol Metab.
2023 Dec;28(4):275-282. 10.6065/apem.2244214.107.
Glycemic control and complications of type 2 diabetes mellitus in children and adolescents during the COVID-19 outbreak
- Affiliations
-
- 1Department of Pediatrics, Woori Children’s Hospital, Seoul, Korea
- 2Department of Pediatrics, Korea University Ansan Hospital, Korea University College of Medicine, Ansan, Korea
- 3Department of Pediatrics, Korea University Anam Hospital, Korea University College of Medicine, Seoul, Korea
- 4Department of Pediatrics, Korea University Kuro Hospital, Korea University College of Medicine, Seoul, Korea
- KMID: 2549320
- DOI: http://doi.org/10.6065/apem.2244214.107
Abstract
- Purpose
This study aimed to investigate the impact of coronavirus disease 2019 (COVID-19) on type 2 diabetes mellitus (T2DM) in children and adolescents.
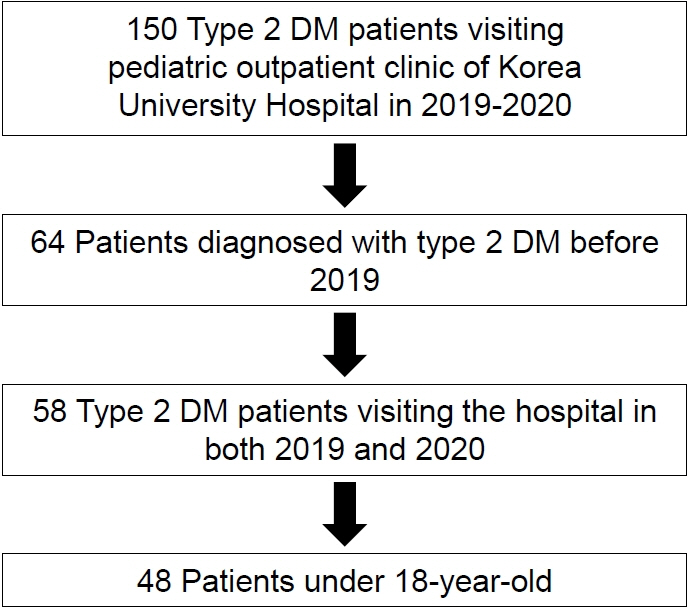
Methods
Children and adolescents diagnosed with T2DM who visited the Korea University Hospital in 2019 and 2020 were retrospectively analyzed, including changes in body mass index (BMI)-standard deviation score (SDS), glycated hemoglobin (HbA1c), diabetes complications, and diabetes management from 2019 to 2020.
Results
Patient mean age and disease duration were 15.48±2.15 and 2.56±1.51 years, respectively. Obese patients accounted for 70.6% of the study population. From 2019 to 2020, mean BMI-SDS (2.21±1.25 vs. 2.35±1.43, P=0.044), HbA1c level (6.5%±2.72% vs. 7.3%±3.70%, P<0.001), blood pressure (BP), total cholesterol, and non–high-density lipoprotein cholesterol level in all patients increased significantly. Obesity was an independent predictor of increased HbA1c (95% confidence interval, 1.071–50.384; P=0.042). HbA1c levels did not increase significantly in nonobese patients, whereas HbA1c (6.45%±2.30% vs. 7.20%±3.05%, P<0.001), BMI-SDS (2.88±0.75 vs. 3.08±0.98, P=0.045), diastolic BP (P=0.037), and total cholesterol values (P=0.019) increased in obese patients in 2020 compared to 2019.
Conclusion
During the COVID-19 outbreak, glycemic control and diabetic complications worsened in children and adolescents with T2DM, particularly in obese patients. Close monitoring for glycemic control and diabetic complications is necessary in children and adolescents with T2DM, especially those with obesity.
Keyword
Figure
Reference
-
References
1. Du Q, Zhang D, Hu W, Li X, Xia Q, Wen T, et al. Nosocomial infection of COVID19: a new challenge for healthcare professionals (Review). Int J Mol Med. 2021; 47:31.2. Panovska-Griffiths J, Kerr CC, Stuart RM, Mistry D, Klein DJ, Viner RM, et al. Determining the optimal strategy for reopening schools, the impact of test and trace interventions, and the risk of occurrence of a second COVID-19 epidemic wave in the UK: a modelling study. Lancet Child Adolesc Health. 2020; 4:817–27.3. Xiang M, Zhang Z, Kuwahara K. Impact of COVID-19 pandemic on children and adolescents' lifestyle behavior larger than expected. Prog Cardiovasc Dis. 2020; 63:531–2.4. Gwag SH, Oh YR, Ha JW, Kang E, Nam HK, Lee Y, et al. Weight changes of children in 1 year during COVID-19 pandemic. J Pediatr Endocrinol Metab. 2022; 35:297–302.5. Weihrauch-Bluher S, Schwarz P, Klusmann JH. Childhood obesity: increased risk for cardiometabolic disease and cancer in adulthood. Metabolism. 2019; 92:147–52.6. Song K, Jeon S, Lee HS, Choi HS, Suh J, Kwon A, et al. Trends of dyslipidemia in Korean youth according to sex and body mass index: based on the Korea National Health and Nutrition Examination Survey (2007-2018). J Pediatr. 2021; 237:71–8.e5.7. Song K, Park G, Lee HS, Lee M, Lee HI, Ahn J, et al. Trends in prediabetes and non-alcoholic fatty liver disease associated with abdominal obesity among Korean children and adolescents: based on the Korea National Health and Nutrition Examination Survey between 2009 and 2018. Biomedicines. 2022; 10:584.8. Jenssen BP, Kelly MK, Powell M, Bouchelle Z, Mayne SL, Fiks AG. COVID-19 and changes in child obesity. Pediatrics. 2021; 147:e2021050123.9. Yang S, Guo B, Ao L, Yang C, Zhang L, Zhou J, et al. Obesity and activity patterns before and during COVID-19 lockdown among youths in China. Clinc Obes. 2020; 10:e12416.10. Benmerzoug M, Djoudi B, Debbache A, Harbouche A, Dehmani ID, Djekkoun N, et al. Impact of COVID-19 lockdown on children's health in North Africa. Matern Child Health J. 2022; 26:1701–8.11. Roh SM, Eun BW, Seo JY. Does coronavirus disease 2019 affect body mass index of children and adolescents who visited a growth clinic in South Korea?: a single-center study. Ann Pediatr Endocrinol Metab. 2022; 27:52–9.12. Kang HM, Jeong DC, Suh BK, Ahn MB. The impact of the coronavirus disease-2019 pandemic on childhood obesity and vitamin D status. J Korean Med Sci. 2021; 36:e21.13. Leitner DR, Fruhbeck G, Yumuk V, Schindler K, Micic D, Woodward E, et al. Obesity and type 2 diabetes: two diseases with a need for combined treatment strategies -EASO can lead the way. Obes Facts. 2017; 10:483–92.14. Xu H, Verre MC. Type 2 diabetes mellitus in children. Am Fam Physician. 2018; 98:590–4.15. Weihrauch-Bluher S, Wiegand S. Risk factors and implications of childhood obesity. Curr Obes R ep. 2018; 7:254–9.16. Serbis A, Giapros V, Kotanidou EP, Galli-Tsinopoulou A, Siomou E. Diagnosis, treatment and prevention of type 2 diabetes mellitus in children and adolescents. World J Diabetes. 2021; 12:344–65.17. Drake AJ, Smith A, Betts PR, Crowne EC, Shield JP. Type 2 diabetes in obese white children. Arch Dis Child. 2002; 86:207–8.18. Schober E, Holl RW, Grabert M, Thon A, Rami B, Kapellen T, et al. Diabetes mellitus type 2 in childhood and adolescence in Germany and parts of Austria. Eur J Pediatr. 2005; 164:705–7.19. Ha J, Oh YR, Kang E, Nam HK, Rhie YJ, Lee KH. Single Point Insulin Sensitivity Estimator for predicting type 2 diabetes mellitus in obese adolescents. Ann Pediatr Endocrinol Metab. 2022; 27:201–6.20. Hong YH, Chung IH, Han K, Chung S. Prevalence of type 2 diabetes mellitus among Korean children, adolescents, and adults younger than 30 years: changes from 2002 to 2016. Diabetes Metab J. 2022; 46:297–306.21. Reinehr T. Type 2 diabetes mellitus in children and adolescents. World J Diabetes. 2013; 4:270–81.22. La Sala L, Pontiroli AE. New fast acting glucagon for recovery from hypoglycemia, a life-threatening situation: nasal powder and injected stable solutions. Int J Mol Sci. 2021; 22:10643.23. Marks BE, Khilnani A, Meyers A, Flokas ME, Gai J, Monaghan M, et al. Increase in the diagnosis and severity of presentation of pediatric type 1 and type 2 diabetes during the COVID-19 pandemic. Horm Res Paediatr. 2021; 94:275–84.24. Lee MS, Lee R, Ko CW, Moon JE. Increase in blood glucose level and incidence of diabetic ketoacidosis in children with type 1 diabetes mellitus in the Daegu-Gyeongbuk area during the coronavirus disease 2019 (COVID-19) pandemic: a retrospective cross-sectional study. J Yeungnam Med Sci. 2022; 39:46–52.25. Magge SN, Wolf RM, Pyle L, Brown EA, Benavides VC, Bianco ME, et al. The coronavirus disease 2019 pandemic is associated with a substantial rise in frequency and severity of presentation of youth-onset type 2 diabetes. J Pediatr. 2022; 251:51–9.e2.26. Shin CH. Impact of COVID-19 pandemic on pediatric diabetes mellitus. J Korean Med Sci. 2022; 37:e186.27. Kim JH, Yun S, Hwang SS, Shim JO, Chae HW, Lee YJ, et al. The 2017 Korean National Growth Charts for children and adolescents: development, improvement, and prospects. Korean J Pediatr. 2018; 61:135–49.28. Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, Daniels SR, et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics. 2017; 140:e20171904.29. Roberts WC. The Friedewald-Levy-Fredrickson formula for calculating low-density lipoprotein cholesterol, the basis for lipid-lowering therapy. Am J Cardiol. 1988; 62:345–6.30. Lim JS, Kim EY, Kim JH, Yoo JH, Yi KH, Chae HW, et al. 2017 Clinical practice guidelines for dyslipidemia of Korean children and adolescents. Ann Pediatr Endocrinol Metab. 2020; 25:199–207.31. Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents; National Heart, Lung, and Blood Institute. Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. Pediatrics. 2011; 128 Suppl 5(Suppl 5):S213–56.32. Vajro P, Lenta S, Socha P, Dhawan A, McKiernan P, Baumann U, et al. Diagnosis of nonalcoholic fatty liver disease in children and adolescents: position paper of the ESPGHAN Hepatology Committee. J Pediatr Gastroenterol Nutr. 2012; 54:700–13.33. Eslam M, Alkhouri N, Vajro P, Baumann U, Weiss R, Socha P, et al. Defining paediatric metabolic (dysfunction)-associated fatty liver disease: an international expert consensus statement. Lancet Gastroenterol Hepatol. 2021; 6:864–73.34. Nur S. Diabetic nephropathy: challenges in pathogenesis, diagnosis, and treatment. Biomed Res Int. 2021; 2021:1497449.35. Gavin B, Lyne J, McNicholas F. The global impact on mental health almost 2 years into the COVID-19 pandemic. Ir J Psychol Med. 2021; 38:243–6.36. Pulgaron ER, Delamater AM. Obesity and type 2 diabetes in children: epidemiology and treatment. Curr Diab Rep. 2014; 14:508.37. Biamonte E, Pegoraro F, Carrone F, Facchi I, Favacchio G, Lania AG, et al. Weight change and glycemic control in type 2 diabetes patients during COVID-19 pandemic: the lockdown effect. Endocrine. 2021; 72:604–10.38. Onmez A, Gamsizkan Z, Ozdemir S, Kesikbas E, Gokosmanoglu F, Torun S, et al. The effect of COVID-19 lockdown on glycemic control in patients with type 2 diabetes mellitus in Turkey. Diabetes Metab Syndr. 2020; 14:1963–6.39. Brooks CG, Spencer JR, Sprafka JM, Roehl KA, Ma J, Londhe AA, et al. Pediatric BMI changes during COVID-19 pandemic: an electronic health record-based retrospective cohort study. EClinicalMedicine. 2021; 38:101026.40. Ge W, Hu J, Xiao Y, Liang F, Yi L, Zhu R, et al. COVID-19‒related childhood BMI increases in China: a health surveillance‒based ambispective cohort analysis. Am J Prev Med. 2022; 63:647–55.41. Pietrobelli A, Pecoraro L, Ferruzzi A, Heo M, Faith M, Zoller T, et al. Effects of COVID-19 lockdown on lifestyle behaviors in children with obesity living in Verona, Italy: a longitudinal study. Obesity (Silver Spring). 2020; 28:1382–5.42. Wang G, Zhang Y, Zhao J, Zhang J, Jiang F. Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet. 2020; 395:945–7.43. Selek A, Gezer E, Altun E, Sözen M, Topaloğlu Ö, Köksalan D, et al. The impact of COVID-19 pandemic on glycemic control in patients with diabetes mellitus in Turkey: a multi-center study from Kocaeli. J Diabetes Metab Disord. 2021; 20:1461–7.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Commentary on "Glycemic control and complications of type 2 diabetes mellitus in children and adolescents during the COVID-19 outbreak"
- Changes in metrics of continuous glucose monitoring during COVID-19 in Korean children and adolescents with type 1 diabetes mellitus
- COVID-19 and diabetes in children
- Year-Long Trend in Glycated Hemoglobin Levels in Patients with Type 2 Diabetes during the COVID-19 Pandemic
- Impact of COVID-19 lockdown on blood glucose levels in pediatric patients with type 1 diabetes mellitus