Endocrinol Metab.
2023 Dec;38(6):669-678. 10.3803/EnM.2023.1734.
Age-Dependent Association of Height Loss with Incident Fracture Risk in Postmenopausal Korean Women
- Affiliations
-
- 1Yonsei University College of Medicine, Seoul, Korea
- 2Department of Internal Medicine, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- 3Department of Internal Medicine, Severance Hospital, Endocrine Research Institute, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2549260
- DOI: http://doi.org/10.3803/EnM.2023.1734
Abstract
- Background
Height loss is a simple clinical measure associated with increased fracture risk. However, limited data exists on the association between height loss and fracture risk in postmenopausal Korean women. It is unknown whether this association varies with age.
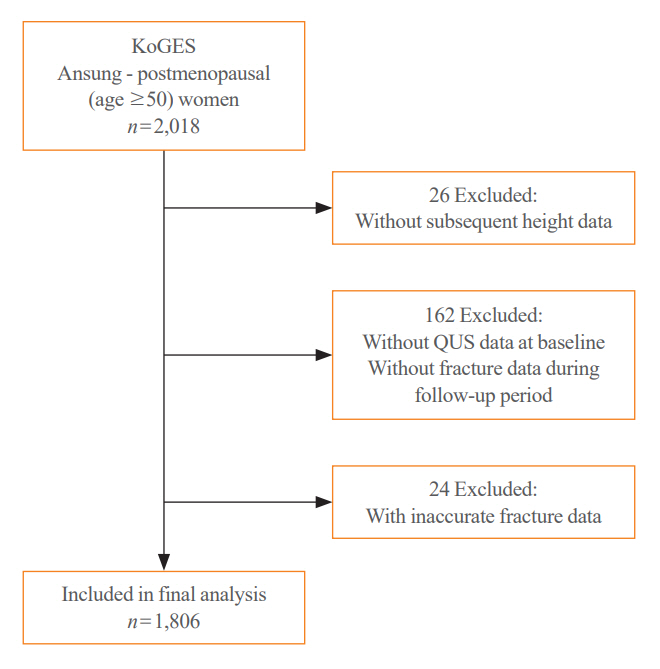
Methods
Data on height loss over a 6-year period were collected from a community-based longitudinal follow-up cohort (Ansung cohort of the Korean Genome and Epidemiology Study). Incident fractures were defined based on self-reported fractures after excluding those due to severe trauma or toes/fingers. The association between incident fractures and height loss was investigated using a Cox proportional hazards model.
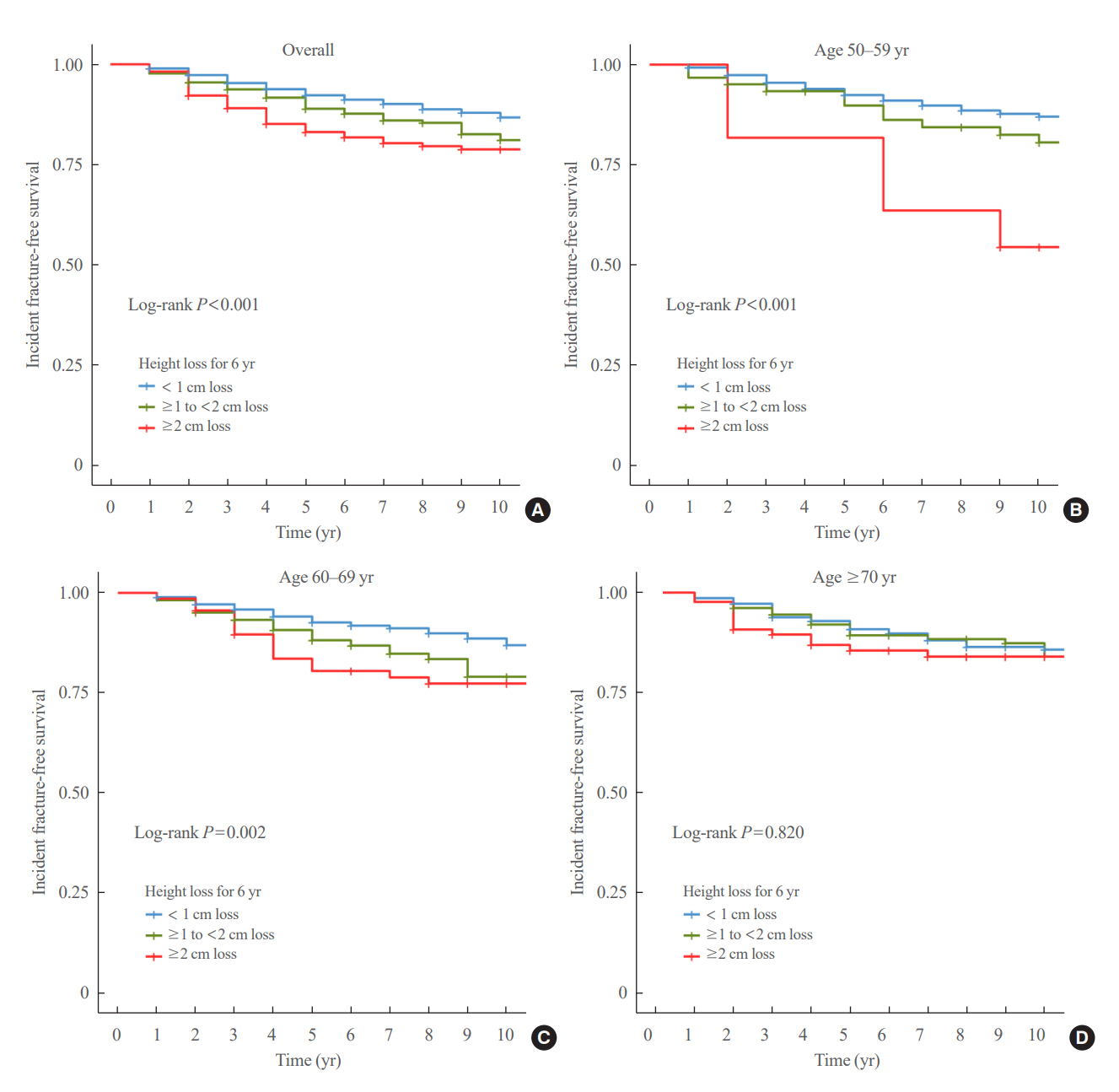
Results
During a median follow-up of 10 years after the second visit, 259/1,806 participants (median age, 64 years) experienced incident fractures. Overall, a 1 standard deviation (SD) decrease in height (1.6 cm/median 5.8 years) was associated with 9% increased risk of fracture (hazard ratio [HR], 1.09; P=0.037), which lost statistical significance after adjustment for covariates. When stratified into age groups (50–59, 60–69, 70 years or older), a 1 SD decrease in height remained a robust predictor of fracture in the 50 to 59 years age group after adjusting for covariates (adjusted hazard ratio [aHR], 1.52; P=0.003), whereas height loss was not an independent predictor of fracture in the 60 to 69 (aHR, 1.06; P=0.333) or the 70 years or older age groups (aHR, 1.05; P=0.700; P for interaction <0.05, for all).
Conclusion
Height loss during the previous 6 years was associated with an increased 10-year fracture risk in postmenopausal women in their 50s.
Keyword
Figure
Reference
-
1. Baek YH, Cho SW, Jeong HE, Kim JH, Hwang Y, Lange JL, et al. 10-Year fracture risk in postmenopausal women with osteopenia and osteoporosis in South Korea. Endocrinol Metab (Seoul). 2021; 36:1178–88.
Article2. Civinini R, Paoli T, Cianferotti L, Cartei A, Boccaccini A, Peris A, et al. Functional outcomes and mortality in geriatric and fragility hip fractures-results of an integrated, multidisciplinary model experienced by the “Florence hip fracture unit”. Int Orthop. 2019; 43:187–92.
Article3. Mariconda M, Costa GG, Cerbasi S, Recano P, Aitanti E, Gambacorta M, et al. The determinants of mortality and morbidity during the year following fracture of the hip: a prospective study. Bone Joint J. 2015; 97-B:383–90.4. Lee TC, Ho PS, Lin HT, Ho ML, Huang HT, Chang JK. One-year readmission risk and mortality after hip fracture surgery: a national population-based study in Taiwan. Aging Dis. 2017; 8:402–9.
Article5. Dubljanin-Raspopovic E, Markovic-Denic L, Marinkovic J, Nedeljkovic U, Bumbasirevic M. Does early functional outcome predict 1-year mortality in elderly patients with hip fracture? Clin Orthop Relat Res. 2013; 471:2703–10.
Article6. Yoshimura N, Kinoshita H, Takijiri T, Oka H, Muraki S, Mabuchi A, et al. Association between height loss and bone loss, cumulative incidence of vertebral fractures and future quality of life: the Miyama study. Osteoporos Int. 2008; 19:21–8.
Article7. Yeoum SG, Lee JH. Usefulness of estimated height loss for detection of osteoporosis in women. J Korean Acad Nurs. 2011; 41:758–67.
Article8. Asahi R, Yuguchi S, Kamo T, Azami M, Ogihara H, Asano S. Association of height loss with falls and sarcopenia in community-dwelling older women. Osteoporos Sarcopenia. 2020; 6:59–64.
Article9. Leslie WD, Schousboe JT, Morin SN, Martineau P, Lix LM, Johansson H, et al. Measured height loss predicts incident clinical fractures independently from FRAX: a registry-based cohort study. Osteoporos Int. 2020; 31:1079–87.
Article10. Schuit SC, van der Klift M, Weel AE, de Laet CE, Burger H, Seeman E, et al. Fracture incidence and association with bone mineral density in elderly men and women: the Rotterdam Study. Bone. 2004; 34:195–202.
Article11. Kim Y, Han BG; KoGES group. Cohort profile: the Korean Genome and Epidemiology Study (KoGES) Consortium. Int J Epidemiol. 2017; 46:1350.
Article12. Sorkin JD, Muller DC, Andres R. Longitudinal change in height of men and women: implications for interpretation of the body mass index: the Baltimore Longitudinal Study of Aging. Am J Epidemiol. 1999; 150:969–77.
Article13. Son IH, Han YH, Hyun T. Changes in weight, waist circumference, prevalence of obesity, and dietary factors associated with weight gain over 8 years in Korean adults: longitudinal data from the Korean Genome and Epidemiology Study. J Nutr Health. 2017; 50:336–49.
Article14. Kanis JA, Harvey NC, Johansson H, Oden A, McCloskey EV, Leslie WD. Overview of fracture prediction tools. J Clin Densitom. 2017; 20:444–50.
Article15. Blake GM, Fogelman I. The clinical role of dual energy X-ray absorptiometry. Eur J Radiol. 2009; 71:406–14.
Article16. Marshall D, Johnell O, Wedel H. Meta-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fractures. BMJ. 1996; 312:1254–9.
Article17. Kanis JA, Johansson H, Harvey NC, McCloskey EV. A brief history of FRAX. Arch Osteoporos. 2018; 13:118.
Article18. Siminoski K, Jiang G, Adachi JD, Hanley DA, Cline G, Ioannidis G, et al. Accuracy of height loss during prospective monitoring for detection of incident vertebral fractures. Osteoporos Int. 2005; 16:403–10.
Article19. Xu W, Perera S, Medich D, Fiorito G, Wagner J, Berger LK, et al. Height loss, vertebral fractures, and the misclassification of osteoporosis. Bone. 2011; 48:307–11.
Article20. Mikula AL, Hetzel SJ, Binkley N, Anderson PA. Validity of height loss as a predictor for prevalent vertebral fractures, low bone mineral density, and vitamin D deficiency. Osteoporos Int. 2017; 28:1659–65.
Article21. Hillier TA, Lui LY, Kado DM, LeBlanc ES, Vesco KK, Bauer DC, et al. Height loss in older women: risk of hip fracture and mortality independent of vertebral fractures. J Bone Miner Res. 2012; 27:153–9.
Article22. Moayyeri A, Luben RN, Bingham SA, Welch AA, Wareham NJ, Khaw KT. Measured height loss predicts fractures in middle-aged and older men and women: the EPIC-Norfolk prospective population study. J Bone Miner Res. 2008; 23:425–32.
Article23. Pluskiewicz W, Adamczyk P, Drozdzowska B. Height loss in postmenopausal women-do we need more for fracture risk assessment?: results from the GO Study. Osteoporos Int. 2021; 32:2043–9.
Article24. Center JR, Nguyen TV, Pocock NA, Noakes KA, Kelly PJ, Eisman JA, et al. Femoral neck axis length, height loss and risk of hip fracture in males and females. Osteoporos Int. 1998; 8:75–81.
Article25. Ahn KS, Kang CH, Cho SB, Cho KH, Han KD, Park YG, et al. Height loss was associated with osteoporosis in Korean elderly men, not in women: the Korea National Health and Nutrition Examination Survey 2008-2010. J Clin Densitom. 2019; 22:59–66.
Article26. Ji S, Lee E, Kim BJ, Baek JY, Yi Y, Jang IY, et al. Height loss as an indicator of ageing through its association with frailty and sarcopenia: an observational cohort study. Arch Gerontol Geriatr. 2023; 110:104916.
Article27. Peter RS, Fromm E, Klenk J, Concin H, Nagel G. Change in height, weight, and body mass index: longitudinal data from Austria. Am J Hum Biol. 2014; 26:690–6.28. Galbusera F, van Rijsbergen M, Ito K, Huyghe JM, Brayda-Bruno M, Wilke HJ. Ageing and degenerative changes of the intervertebral disc and their impact on spinal flexibility. Eur Spine J. 2014; 23 Suppl 3:S324–32.
Article29. Kinoshita H, Tamaki T, Hashimoto T, Kasagi F. Factors influencing lumbar spine bone mineral density assessment by dual-energy X-ray absorptiometry: comparison with lumbar spinal radiogram. J Orthop Sci. 1998; 3:3–9.
Article30. Kim HS, Yang SO. Quality control of DXA system and precision test of radio-technologists. J Bone Metab. 2014; 21:2–7.
Article31. Link TM, Lang TF. Axial QCT: clinical applications and new developments. J Clin Densitom. 2014; 17:438–48.
Article32. Ensrud KE, Schousboe JT, Kats AM, Vo TN, Taylor BC, Cawthon PM, et al. Height loss in old age and fracture risk among men in late life: a prospective cohort study. J Bone Miner Res. 2021; 36:1069–76.
Article33. Gadam RK, Schlauch K, Izuora KE. Frax prediction without BMD for assessment of osteoporotic fracture risk. Endocr Pract. 2013; 19:780–4.
Article34. Kanis JA, McCloskey E, Johansson H, Oden A, Leslie WD. FRAX(®) with and without bone mineral density. Calcif Tissue Int. 2012; 90:1–13.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intervention thresholds to identify postmenopausal women with high fracture risk: A single center study based on the Philippines FRAX model
- Association of height loss with falls and sarcopenia in communitydwelling older women
- Validation of age- and sex-dependent association of uric acid and incident hypertension in rural areas
- The bone mineral densities in Korean postmenopausal women: a comparison between natural and surgically induced menopause
- Incidence of Osteoporosis and Falls and Predictors of Fracture Risk in Postmenopausal Women