J Korean Med Sci.
2023 Dec;38(47):e359. 10.3346/jkms.2023.38.e359.
The Prevalence and Risk Factors of Clostridioides difficile Infection in Inflammatory Bowel Disease: 10-Year South Korean Experience Based on the National Database
- Affiliations
-
- 1Department of Internal Medicine, Ewha Womans University College of Medicine, Seoul, Korea
- 2Department of Preventive Medicine and Public Health, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 3Department of Internal Medicine, Eunpyeong St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2548801
- DOI: http://doi.org/10.3346/jkms.2023.38.e359
Abstract
- Background
Few studies evaluate the epidemiology and risk factors of Clostridioides difficile infection (CDI) in Asian patients with inflammatory bowel disease (IBD). We investigated the year-end prevalence, cumulative incidence and risk factors of CDI in Asian patients with IBD using a large-scale population-based cohort in Korea.
Methods
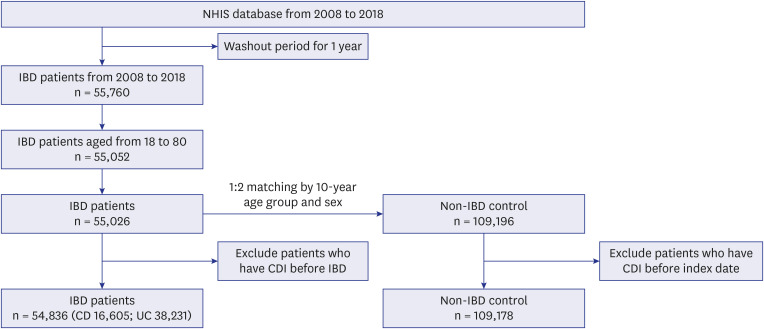
Using the National Health Insurance Service database, we identified patients with IBD and sex- and age-matched controls without IBD between 2008 and 2018. The year-end prevalence and cumulative incidence of CDI were compared among patients with Crohn’s disease (CD) and ulcerative colitis (UC) with controls. The risk factors for CDI were evaluated.
Results
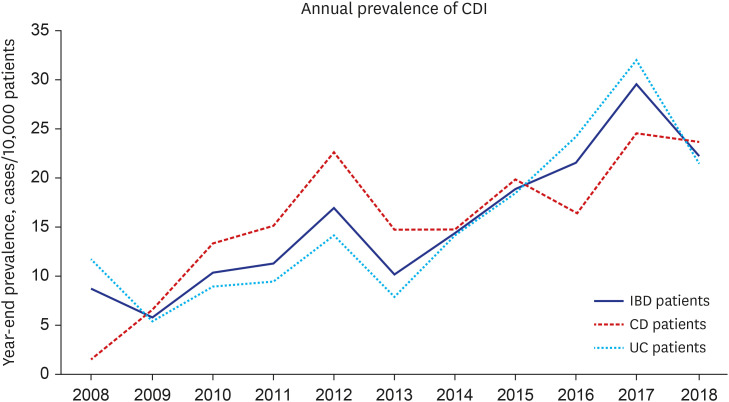
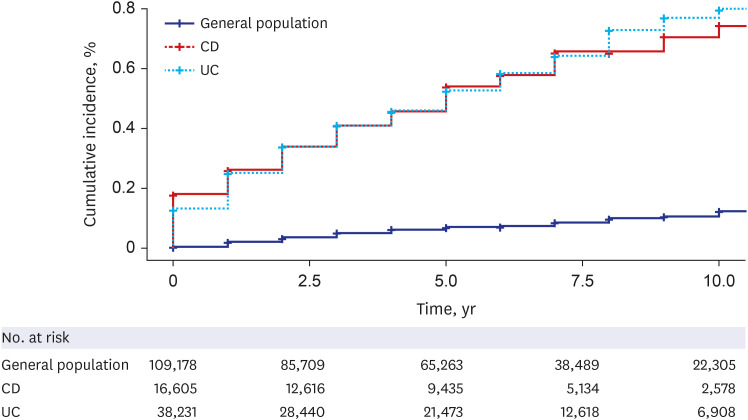
Among the 54,836 patients with IBD and 109,178 controls, CDI occurred in 293 patients with IBD and 87 controls. The annual year-end prevalence of CDI in patients with IBD increased from 8.6/10,000 persons in 2008 to 22.3/10,000 persons in 2018. The risk of CDI was higher in both patients with CD and UC than that in the matched controls (hazard ratio [HR], 7.285; 95% confidence interval [CI], 5.388–9.851; P < 0.001 and HR, 7.487; 95% CI, 5.796–9.670; P < 0.001, respectively). Among patients with IBD, the risk factors for CDI included older age, female sex, high Charlson comorbidity index score, and IBD-related medications including oral 5-aminosalicylic acid, immunomodulatory agents, biologics, and steroids used for > 90 days.
Conclusion
The risk of CDI in Korean patients with IBD was approximately seven times higher than that in controls without IBD, and the annual year-end prevalence of CDI continuously increased from 2008 to 2018.
Keyword
Figure
Reference
-
1. Bartlett JG, Chang TW, Gurwith M, Gorbach SL, Onderdonk AB. Antibiotic-associated pseudomembranous colitis due to toxin-producing clostridia. N Engl J Med. 1978; 298(10):531–534. PMID: 625309.
Article2. Balram B, Battat R, Al-Khoury A, D’Aoust J, Afif W, Bitton A, et al. Risk factors associated with Clostridium difficile Infection in inflammatory bowel disease: a systematic review and meta-analysis. J Crohn’s Colitis. 2019; 13(1):27–38. PMID: 30247650.
Article3. Kelly CR, Fischer M, Allegretti JR, LaPlante K, Stewart DB, Limketkai BN, et al. ACG clinical guidelines: prevention, diagnosis, and treatment of Clostridioides difficile infections. Am J Gastroenterol. 2021; 116(6):1124–1147. PMID: 34003176.
Article4. Shim JK, Johnson S, Samore MH, Bliss DZ, Gerding DN. Primary symptomless colonisation by Clostridium difficile and decreased risk of subsequent diarrhoea. Lancet. 1998; 351(9103):633–636. PMID: 9500319.
Article5. Burke KE, Lamont JT. Clostridium difficile infection: a worldwide disease. Gut Liver. 2014; 8(1):1–6. PMID: 24516694.
Article6. Gujja D, Friedenberg FK. Predictors of serious complications due to Clostridium difficile infection. Aliment Pharmacol Ther. 2009; 29(6):635–642. PMID: 19077106.
Article7. Kim J, Pai H, Seo MR, Kang JO. Epidemiology and clinical characteristics of Clostridium difficile infection in a Korean tertiary hospital. J Korean Med Sci. 2011; 26(10):1258–1264. PMID: 22022175.
Article8. Kelly CP, LaMont JT. Clostridium difficile--more difficult than ever. N Engl J Med. 2008; 359(18):1932–1940. PMID: 18971494.9. Guo CL, Kwong TN, Mak JW, Zhang L, Lui GC, Wong GL, et al. Trends in incidence and clinical outcomes of Clostridioides difficile infection, Hong Kong. Emerg Infect Dis. 2021; 27(12):3036–3044. PMID: 34812719.10. Choi HY, Park SY, Kim YA, Yoon TY, Choi JM, Choe BK, et al. The epidemiology and economic burden of Clostridium difficile infection in Korea. BioMed Res Int. 2015; 2015:510386. PMID: 25821807.11. Kim YS, Han DS, Kim YH, Kim WH, Kim JS, Kim HS, et al. Incidence and clinical features of Clostridium difficile infection in Korea: a nationwide study. Epidemiol Infect. 2013; 141(1):189–194. PMID: 22717061.
Article12. Bossuyt P, Verhaegen J, Van Assche G, Rutgeerts P, Vermeire S. Increasing incidence of Clostridium difficile-associated diarrhea in inflammatory bowel disease. J Crohn’s Colitis. 2009; 3(1):4–7. PMID: 21172241.
Article13. Issa M, Vijayapal A, Graham MB, Beaulieu DB, Otterson MF, Lundeen S, et al. Impact of Clostridium difficile on inflammatory bowel disease. Clin Gastroenterol Hepatol. 2007; 5(3):345–351. PMID: 17368234.14. Song EM, Yang SK. Natural history of inflammatory bowel disease: a comparison between the East and the West. Intest Res. 2022; 20(4):418–430. PMID: 34852421.
Article15. Yen HH, Weng MT, Tung CC, Wang YT, Chang YT, Chang CH, et al. Epidemiological trend in inflammatory bowel disease in Taiwan from 2001 to 2015: a nationwide population-based study. Intest Res. 2019; 17(1):54–62. PMID: 30449079.
Article16. Ye BD, Choi H, Hong M, Yun WJ, Low HQ, Haritunians T, et al. Identification of ten additional susceptibility loci for ulcerative colitis through immunochip analysis in Koreans. Inflamm Bowel Dis. 2016; 22(1):13–19. PMID: 26398853.
Article17. Nguyen GC, Kaplan GG, Harris ML, Brant SR. A national survey of the prevalence and impact of Clostridium difficile infection among hospitalized inflammatory bowel disease patients. Am J Gastroenterol. 2008; 103(6):1443–1450. PMID: 18513271.
Article18. Barber GE, Hendler S, Okafor P, Limsui D, Limketkai BN. Rising incidence of intestinal infections in inflammatory bowel disease: a nationwide analysis. Inflamm Bowel Dis. 2018; 24(8):1849–1856. PMID: 29722832.
Article19. Singh H, Nugent Z, Yu BN, Lix LM, Targownik LE, Bernstein CN. Higher incidence of Clostridium difficile infection among individuals with inflammatory bowel disease. Gastroenterology. 2017; 153(2):430–438.e2. PMID: 28479377.
Article20. Kaneko T, Matsuda R, Taguri M, Inamori M, Ogura A, Miyajima E, et al. Clostridium difficile infection in patients with ulcerative colitis: investigations of risk factors and efficacy of antibiotics for steroid refractory patients. Clin Res Hepatol Gastroenterol. 2011; 35(4):315–320. PMID: 21435967.
Article21. Nomura K, Fujimoto Y, Yamashita M, Morimoto Y, Ohshiro M, Sato K, et al. Absence of pseudomembranes in Clostridium difficile-associated diarrhea in patients using immunosuppression agents. Scand J Gastroenterol. 2009; 44(1):74–78. PMID: 18781540.
Article22. Kim DB, Lee KM, Park SH, Kim YS, Kim ES, Lee J, et al. Is Clostridium difficile infection a real threat in patients with ulcerative colitis? A prospective, multicenter study in Korea. Intest Res. 2018; 16(2):267–272. PMID: 29743839.
Article23. Li Y, Xu H, Xu T, Xiao M, Tang H, Wu D, et al. Case-control study of inflammatory bowel disease patients with and without Clostridium difficile infection and poor outcomes in patients coinfected with C. difficile and cytomegalovirus. Dig Dis Sci. 2018; 63(11):3074–3083. PMID: 30094621.
Article24. Rodemann JF, Dubberke ER, Reske KA, Seo DH, Stone CD. Incidence of Clostridium difficile infection in inflammatory bowel disease. Clin Gastroenterol Hepatol. 2007; 5(3):339–344. PMID: 17368233.
Article25. Joshi NM, Marks IH, Crowson R, Ball D, Rampton DS. Incidence and outcome of Clostridium difficile infection in hospitalized patients with inflammatory bowel disease in the UK. J Crohn’s Colitis. 2017; 11(1):70–76. PMID: 27302972.
Article26. Navaneethan U, Mukewar S, Venkatesh PG, Lopez R, Shen B. Clostridium difficile infection is associated with worse long term outcome in patients with ulcerative colitis. J Crohn’s Colitis. 2012; 6(3):330–336. PMID: 22405170.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clostridioides Infection in Patients with Inflammatory Bowel Disease
- Management of Clostridioides difficile infection in patients with inflammatory bowel disease
- Durability and outcomes of fecal microbiota transplantation for recurrent Clostridioides difficile infection in patients with moderate to severe inflammatory bowel disease
- Clinical and Microbiological Risk Factors for Community-Associated Clostridioides difficile Infections
- Clostridium difficile Infection at Diagnosis and during the Disease Course of Pediatric Inflammatory Bowel Disease