Ann Surg Treat Res.
2023 Dec;105(6):396-403. 10.4174/astr.2023.105.6.396.
The outcome of hiatal hernia repair and factors associated with surgical outcome in the pediatric population: a single-center experience
- Affiliations
-
- 1Department of Pediatric Surgery, Children's Hospital, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2548784
- DOI: http://doi.org/10.4174/astr.2023.105.6.396
Abstract
- Purpose
Hiatal hernia in children is a rare condition, and there is limited knowledge available about the disease itself. There is currently no agreement or consensus on the treatment of hiatal hernia in the pediatric population due to lack of evidence. In this study, we were to assess our experience with hiatal hernia, including the characteristics of our patients, surgical outcomes, and factors that influence the outcomes.
Methods
We retrospectively reviewed the medical records of 49 patients below the age of 18 years who underwent hiatal hernia repair at the Asan Medical Center between 2006 and 2021. We analyzed and compared the general characteristics and surgical outcomes based on the presence of recurrence and coexisting congenital diseases.
Results
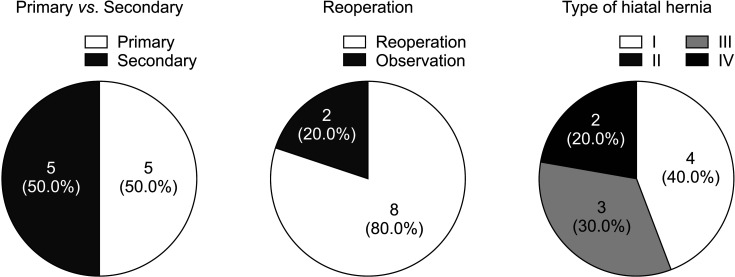
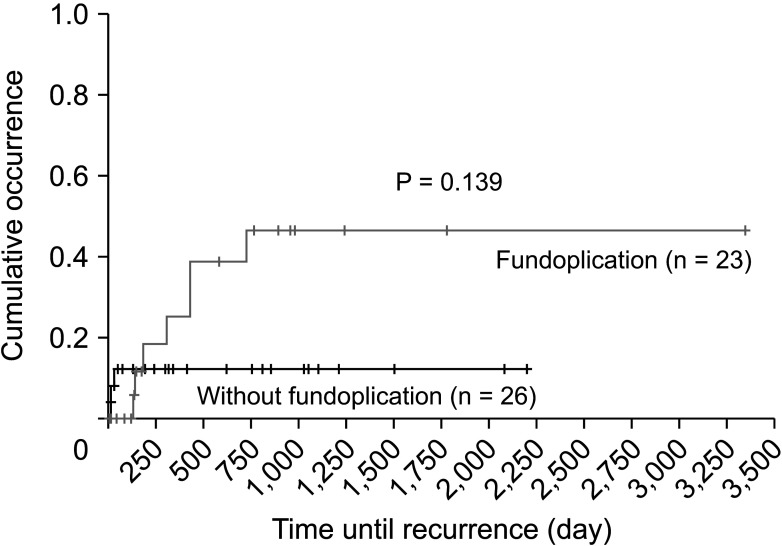
Hiatal hernia progression was found to be associated with various medical conditions; however, no significant differences in patient characteristics or surgical outcomes between those with and without comorbidities were observed. There were no significant differences in patient characteristics or outcomes between the initial and redo operations. Fundoplication was performed in 19 patients (36.7%) during the initial operation and in 7 patients (87.5%) during repeat hiatal hernia repair.
Conclusion
The presence of an underlying disease didn’t influence the treatment and progression of hiatal hernia. Furthermore, there were no significant differences in the clinical course between patients with recurrent hiatal hernia and those experiencing it for the first time. Additionally, the impact of fundoplication on the recurrence of hiatal hernia in pediatric patients was found to be minimal.
Keyword
Figure
Reference
-
1. Stylopoulos N, Rattner DW. The history of hiatal hernia surgery: from Bowditch to laparoscopy. Ann Surg. 2005; 241:185–193. PMID: 15622007.2. Kahrilas PJ, Kim HC, Pandolfino JE. Approaches to the diagnosis and grading of hiatal hernia. Best Pract Res Clin Gastroenterol. 2008; 22:601–616. PMID: 18656819.
Article3. Garvey EM, Ostlie DJ. Hiatal and paraesophageal hernia repair in pediatric patients. Semin Pediatr Surg. 2017; 26:61–66. PMID: 28550872.
Article4. Namgoong JM, Kim DY, Kim SC, Hwang JH. Hiatal hernia in pediatric patients: laparoscopic versus open approaches. Ann Surg Treat Res. 2014; 86:264–269. PMID: 24851228.
Article5. Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) Guidelines Committee. Guidelines for the management of hiatal hernia [Internet]. SAGES;c1985. cited 2023 Apr. Available from: https://www.sages.org/publications/guidelines/guidelines-forthe-management-of-hiatal-hernia/ .6. Solomon D, Bekhor E, Kashtan H. Paraesophageal hernia: to fundoplicate or not? Ann Transl Med. 2021; 9:902. PMID: 34164536.
Article7. Granderath FA, Schweiger UM, Kamolz T, Pointner R. Dysphagia after laparoscopic antireflux surgery: a problem of hiatal closure more than a problem of the wrap. Surg Endosc. 2005; 19:1439–1446. PMID: 16206005.
Article8. Linnaus ME, Garren A, Gould JC. Anatomic location and mechanism of hiatal hernia recurrence: a video-based assessment. Surg Endosc. 2022; 36:5451–5455. PMID: 34845542.
Article9. Son HY, Chang EY, Chang HK, Oh JT, Han SJ. High incidence of hiatal hernia in esophageal atresia and its etiologic factors. J Korean Assoc Pediatr Surg. 2011; 17:170–178.
Article10. Pilli S, Jiwane A, Krishnan U. Quality of life in children who have undergone fundoplication surgery for the treatment of gastroesophageal reflux disease: a review of literature. Dis Esophagus. 2017; 30:1–5.
Article11. Chang CG, Thackeray L. Laparoscopic hiatal hernia repair in 221 patients: outcomes and experience. JSLS. 2016; 20:e2015.00104.
Article12. Glen P, Chassé M, Doyle MA, Nasr A, Fergusson DA. Partial versus complete fundoplication for the correction of pediatric GERD: a systematic review and meta-analysis. PLoS One. 2014; 9:e112417. PMID: 25386679.
Article13. Serrano L, Saad AR, DuCoin C, Velanovich V. After the hiatal hernia repair: fundoplication, yes or no? Partial or complete? Ann Laparosc Endosc Surg. 2021; 6:22.
Article14. Mauritz FA, Blomberg BA, Stellato RK, van der Zee DC, Siersema PD, van Herwaarden-Lindeboom MY. Complete versus partial fundoplication in children with gastroesophageal reflux disease: results of a systematic review and meta-analysis. J Gastrointest Surg. 2013; 17:1883–1892. PMID: 23943388.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Sliding Hiatal Hernia associated with Bochdalek Hernia Repair
- Two Cases of Bochdalek Hernia and One Case of Hiatal Hernia
- Congenital Hiatal Hernia Associated with Anemia
- High Incidence of Hiatal Hernia in Esophageal Atresia and Its Etiologic Factors
- Characteristics and recent therapeutic trends of pediatric inguinal hernia