Ann Surg Treat Res.
2023 Dec;105(6):369-375. 10.4174/astr.2023.105.6.369.
Protective strategy for the caudate lobe bile duct during left hemihepatectomy based on imaging data analysis
- Affiliations
-
- 1Department of General Surgery, Second Affiliated Hospital of Nanchang University, Nanchang, China
- 2Department of Emergency, First Affiliated Hospital of Nanchang University, Nanchang, China
- KMID: 2548781
- DOI: http://doi.org/10.4174/astr.2023.105.6.369
Abstract
- Purpose
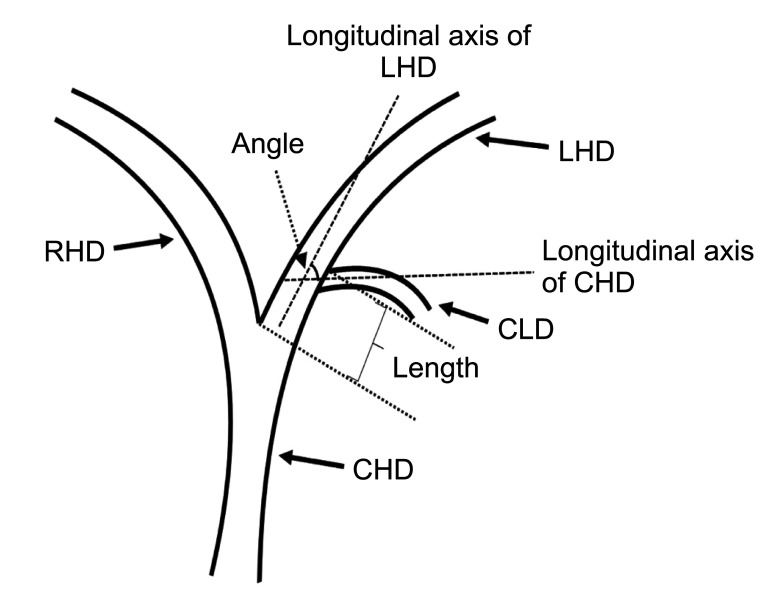
This study was performed to analyze the rule of confluence of the caudate lobe bile duct (CLD) into the left hepatic duct (LHD) and to discuss the protective strategy during left hemihepatectomy.
Methods
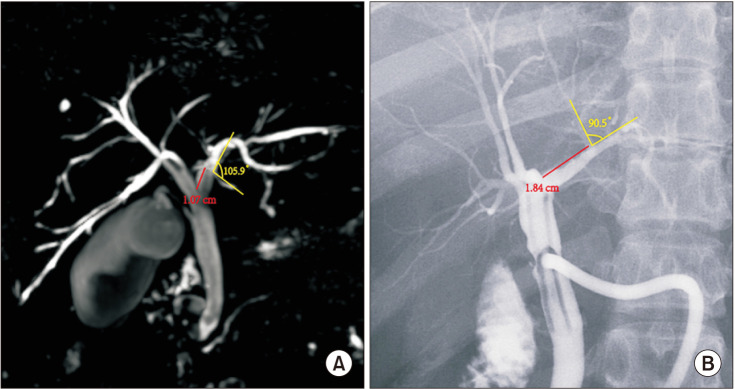
MRI of 400 patients and T-tube angiography images of 100 patients were collected, and the imaging rules of the confluence of the CLD into the LHD were summarized. The clinical data of 33 patients who underwent left hemihepatectomy using the protective strategy were analyzed.
Results
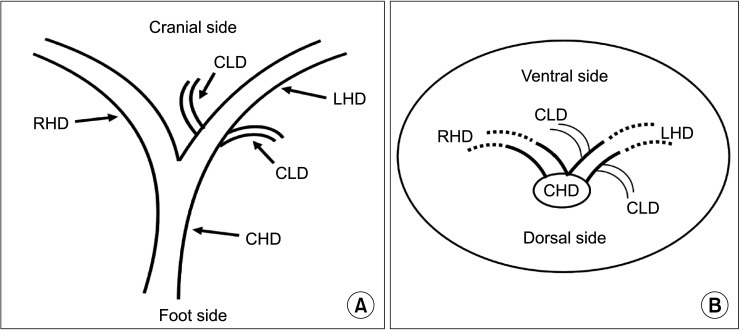
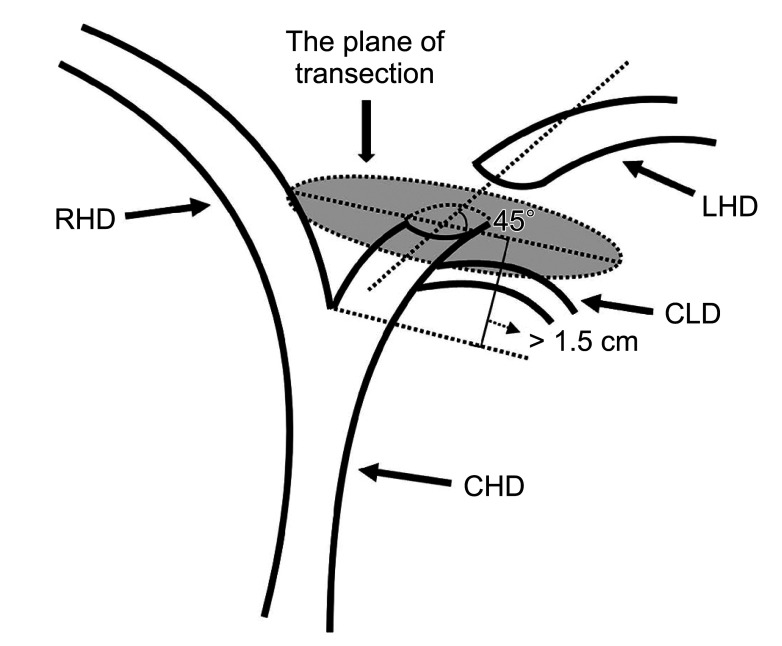
MRI and T-tube angiography images showed that the length from the confluence point of the CLD into the LHD to the confluence of the left and right hepatic ducts was 1.19 ± 0.40 cm and 1.26 ± 0.39 cm, respectively. The average angle between the longitudinal axis of the 2 bile ducts was 68.27° ± 22.59° and 66.58 ± 22.88°, respectively. Coronal and cross-sectional images showed that inflow from the foot side to the cranial side was noted in 79.8% and 82.0% of patients, respectively, and inflow from the dorsal to the ventral side was observed in 84.5% and 88.0%, respectively. Based on these imaging rules, the safe transection length and plane were summarized, and the CLD was effectively protected in 33 cases of left hemihepatectomy.
Conclusion
In left hemihepatectomy, the LHD should be transected at least 1.5 cm away from the confluence of the left and right hepatic ducts, and the plane of transection should be oblique to the dorsal side at an angle of 45° with the LHD, these parameters represent an effective strategy to protect the CLD.
Keyword
Figure
Reference
-
1. Sucandy I, Gravetz A, Ross S, Rosemurgy A. Technique of robotic left hepatectomy: how we approach it. J Robot Surg. 2019; 13:201–207. PMID: 30406886.2. Oh HC, Lee SK, Lee TY, Kwon S, Lee SS, Seo DW, et al. Analysis of percutaneous transhepatic cholangioscopy-related complications and the risk factors for those complications. Endoscopy. 2007; 39:731–736. PMID: 17661249.
Article3. Tian J, Li JW, Chen J, Fan YD, Bie P, Wang SG, et al. Laparoscopic hepatectomy with bile duct exploration for the treatment of hepatolithiasis: an experience of 116 cases. Dig Liver Dis. 2013; 45:493–498. PMID: 23395128.
Article4. Dong J, Lau WY, Lu W, Zhang W, Wang J, Ji W. Caudate lobe-sparing subtotal hepatectomy for primary hepatolithiasis. Br J Surg. 2012; 99:1423–1428. PMID: 22961524.
Article5. Aijun L, Jiamei Y, Qinhe T, Mengchao W. Caudate lobe as the sole remnant liver following extended liver resection for hepatocellular carcinoma. Int J Surg Case Rep. 2014; 5:462–464. PMID: 24973528.
Article6. Feng X, Dong J. Surgical management for bile duct injury. Biosci Trends. 2017; 11:399–405. PMID: 28824026.
Article7. Kumon M, Kumon T, Tsutsui E, Ebashi C, Namikawa T, Ito K, et al. Definition of the caudate lobe of the liver based on portal segmentation. Glob Health Med. 2020; 2:328–336. PMID: 33330828.
Article8. Edo H, Sekiguchi R, Edo N, Kajiyama A, Nagamoto M, Gomi T. Evaluation of biliary anatomy in the caudate lobe using drip infusion cholangiography-computed tomography. Abdom Radiol (NY). 2019; 44:886–893. PMID: 30448918.
Article9. Kumon M. Anatomical study of the caudate lobe with special reference to portal venous and biliary branches using corrosion liver casts and clinical application. Liver Cancer. 2017; 6:161–170. PMID: 28275582.
Article10. Martins AC, Martins C. Surgical anatomy of caudate bile ducts: silicon-injected cadaveric-livers dissected under magnification. Ann Hepatobiliary Pancreat Surg. 2020; 24:415–420. PMID: 33234743.
Article11. Kim JH, Choi JW. Intrahepatic Glissonian approach to the ventral aspect of the Arantius ligament in laparoscopic left hemihepatectomy. World J Surg. 2019; 43:1303–1307. PMID: 30652216.
Article12. Hyodo T, Kumano S, Kushihata F, Okada M, Hirata M, Tsuda T, et al. CT and MR cholangiography: advantages and pitfalls in perioperative evaluation of biliary tree. Br J Radiol. 2012; 85:887–896. PMID: 22422383.
Article13. Umut T, Remzi E. Correlation among 3-dimensional magnetic resonance cholangiography, intraoperative cholangiography, and intraoperative findings in right liver donors. Exp Clin Transplant. 2021; 02. 23. DOI: 10.6002/ect.2020.0220. [Epub].
Article14. Birgin E, Reissfelder C, Rahbari NN. Robotic left hepatectomy using the Glissonean pedicle approach for the treatment of Caroli’s syndrome. Zentralbl Chir. 2023; 148:129–132. PMID: 36104087.
Article15. Yao DB, Wu SD. Application of stapling devices in liver surgery: current status and future prospects. World J Gastroenterol. 2016; 22:7091–7098. PMID: 27610019.
Article16. Zheng SG. Characteristics and prevention strategies of bile duct injury in laparoscopic hepatectomy. Chin J Pract Surg. 2018; 38:1011–1014.17. Sugiura T, Nagino M, Kamiya J, Nishio H, Ebata T, Yokoyama Y, et al. Infraportal bile duct of the caudate lobe: a troublesome anatomic variation in right-sided hepatectomy for perihilar cholangiocarcinoma. Ann Surg. 2007; 246:794–798. PMID: 17968171.18. Shibata H, Aoki T, Koizumi T, Kusano T, Yamazaki T, Saito K, et al. The efficacy of intraoperative fluorescent imaging using indocyanine green for cholangiography during cholecystectomy and hepatectomy. Clin Exp Gastroenterol. 2021; 14:145–154. PMID: 33958888.
Article19. Seeras K, Qasawa RN, Kashyap S, Kalani AD. Bile duct repair. StatPearls [Internet]. StatPearls Publishing;2023. 01-. updated 2023 May 22. Available from: https://www.ncbi.nlm.nih.gov/books/NBK525989/.20. Lubikowski J, Piotuch B, Stadnik A, Przedniczek M, Remiszewski P, Milkiewicz P, et al. Difficult iatrogenic bile duct injuries following different types of upper abdominal surgery: report of three cases and review of literature. BMC Surg. 2019; 19:162. PMID: 31694627.
Article21. Renz BW, Bösch F, Angele MK. Bile duct injury after cholecystectomy: surgical therapy. Visc Med. 2017; 33:184–190. PMID: 28785565.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Role of Bile Duct Probe for Bile Duct Division during Donor Right Hemihepatectomy
- Isolated Caudate Lobectomy with Bile Duct Resection Performed in a Patient with Type IV Hilar Bile Duct Cancer
- An Analysis on the Usefulness of Concomitant Procurement of the Caudate Lobe in Living Donor Liver Transplantation Using a Left Lobe Graft
- S4a+S5 with Caudate Lobe (S1) Resection as a Parenchyma-preserving Liver Resection for a Patient with Type IIIb Hilar Bile Duct Cance
- Quantitative Morphology of the Frontal Lobe and the Caudate Nucleus in Boys with Attention Deficit/Hyperactivity Disorder