Korean J Gastroenterol.
2023 Nov;82(5):248-253. 10.4166/kjg.2023.099.
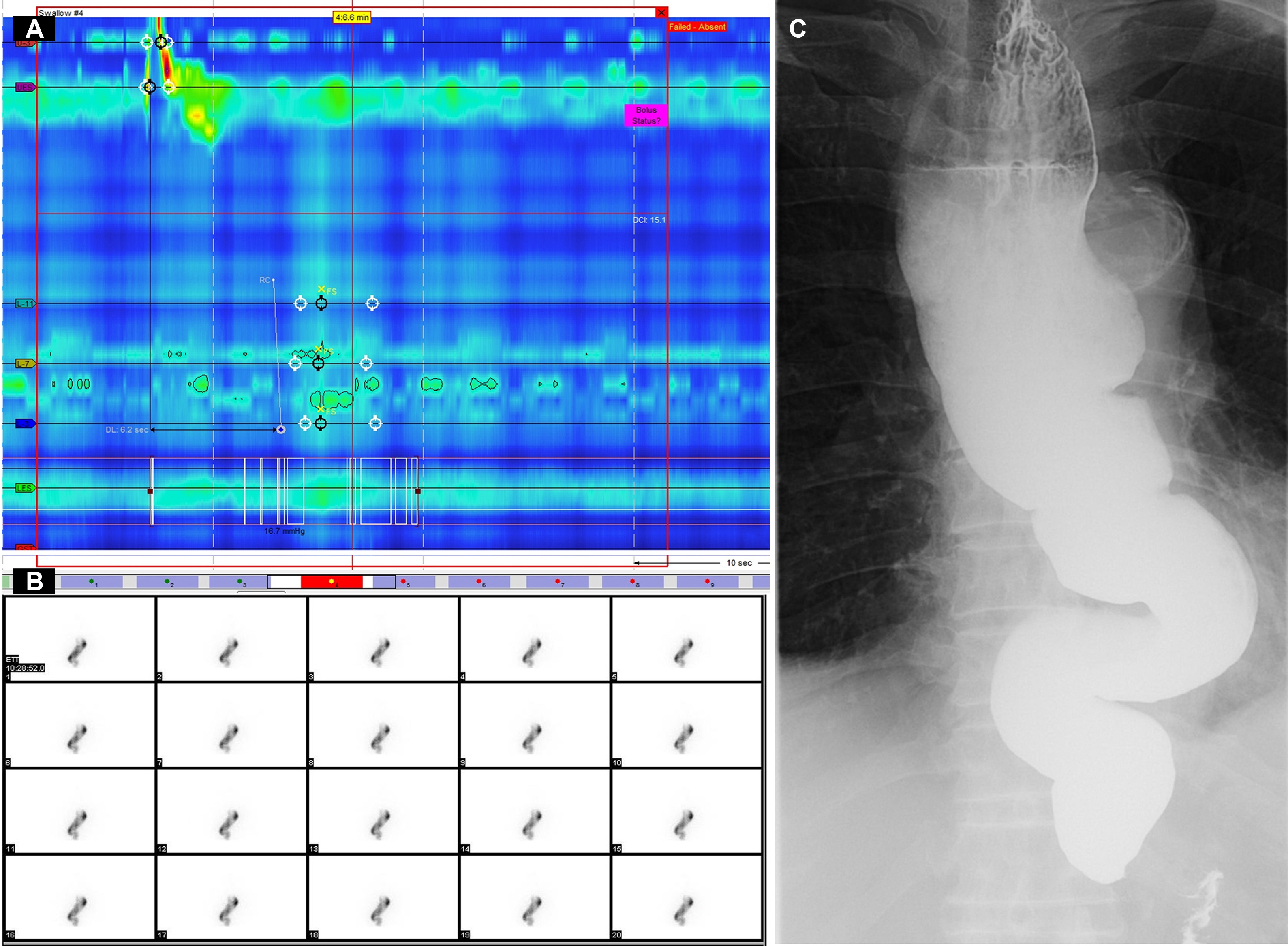
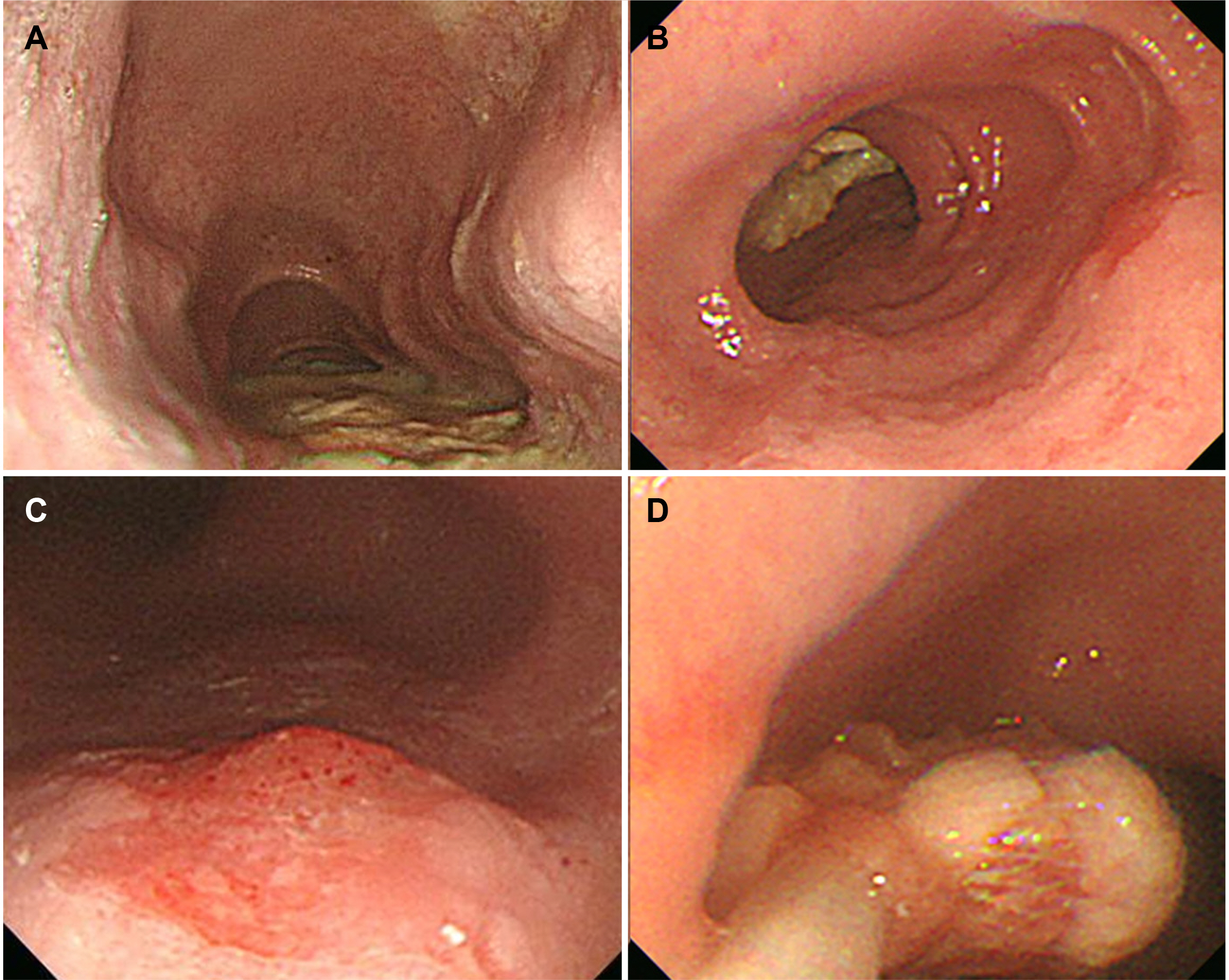
Case of Concomitant Endoscopic Treatment of Achalasia with Superficial Esophageal Cancer
- Affiliations
-
- 1Department of Internal Medicine, Kosin University College of Medicine, Busan, Korea
- KMID: 2548495
- DOI: http://doi.org/10.4166/kjg.2023.099
Abstract
- Achalasia, a rare motility disorder of the esophagus, is generally accepted as a premalignant disorder. This paper presents the case of a 72-year-old male with achalasia and synchronous superficial esophageal cancer who experienced dysphagia symptoms for five years. As achalasia is associated with an increased risk of esophageal cancer, both can be treated simultaneously if detected at the time of diagnosis. Achalasia and synchronous esophageal cancer are rarely detected and treated endoscopically. This paper reports a case of concurrent successful treatment.
Figure
Reference
-
1. Vaezi MF, Pandolfino JE, Vela MF. 2013; ACG clinical guideline: diagnosis and management of achalasia. Am J Gastroenterol. 108:1238–1249. quiz 1250DOI: 10.1038/ajg.2013.196. PMID: 23877351.
Article2. Fagge CH. 1872; A case of simple stenosis of the oesophagus, followed by epithelioma. Guy's Hosp Report (London). 17:413.3. Sato H, Terai S, Shimamura Y, et al. 2021; Achalasia and esophageal cancer: a large database analysis in Japan. J Gastroenterol. 56:360–370. DOI: 10.1007/s00535-021-01763-6. PMID: 33538893.
Article4. Leeuwenburgh I, Haringsma J, Van Dekken H, Scholten P, Siersema PD, Kuipers EJ. Long-term risk of oesophagitis, Barrett's oesophagus and oesophageal cancer in achalasia patients. Scand J Gastroenterol Suppl. 2006; (243):7–10. DOI: 10.1080/00365520600664201. PMID: 16782616.
Article5. Sato H, Nishikawa Y, Abe H, et al. 2022; Esophageal carcinoma in achalasia patients managed with endoscopic submucosal dissection and peroral endoscopic myotomy: Japan Achalasia Multicenter Study. Dig Endosc. 34:965–973. DOI: 10.1111/den.14197. PMID: 34787940.
Article6. Ghoshal UC, Daschakraborty SB, Singh R. 2012; Pathogenesis of achalasia cardia. World J Gastroenterol. 18:3050–3057. DOI: 10.3748/wjg.v18.i24.3050. PMID: 22791940. PMCID: PMC3386318.
Article7. Jung HK, Hong SJ, Lee OY, et al. 2020; 2019 Seoul consensus on esophageal achalasia guidelines. J Neurogastroenterol Motil. 26:180–203. DOI: 10.5056/jnm20014. PMID: 32235027. PMCID: PMC7176504.
Article8. Aadam AA, Abe S. 2018; Endoscopic submucosal dissection for superficial esophageal cancer. Dis Esophagus. 31:doy021. DOI: 10.1093/dote/doy021. PMID: 29982386.
Article9. Das A, Singh V, Fleischer DE, Sharma VK. 2008; A comparison of endoscopic treatment and surgery in early esophageal cancer: an analysis of surveillance epidemiology and end results data. Am J Gastroenterol. 103:1340–1345. DOI: 10.1111/j.1572-0241.2008.01889.x. PMID: 18510606.
Article10. Tang X, Ren Y, Jiang B, Gong W. 2015; Education and imaging: Gastroenterology: Endoscopic mucosal resection for esophageal dysplasia in an achalasia patient followed by peroral endoscopic myotomy. J Gastroenterol Hepatol. 30:1563. DOI: 10.1111/jgh.13034. PMID: 26177680.
Article11. Shi S, Fu K, Dong XQ, Hao YJ, Li SL. 2017; Combination of concurrent endoscopic submucosal dissection and modified peroral endoscopic myotomy for an achalasia patient with synchronous early esophageal neoplasms. World J Gastrointest Endosc. 9:99–104. DOI: 10.4253/wjge.v9.i2.99. PMID: 28250904. PMCID: PMC5311480.
Article12. Park JC, Lee YC, Kim SK, et al. 2009; Achalasia combined with esophageal cancer treated by concurrent chemoradiation therapy. Gut Liver. 3:329–333. DOI: 10.5009/gnl.2009.3.4.329. PMID: 20431771. PMCID: PMC2852741.
Article13. Goudra B, Saumoy M. 2022; Anesthesia for advanced endoscopic procedures. Clin Endosc. 55:1–7. DOI: 10.5946/ce.2021.236. PMID: 34974678. PMCID: PMC8831399.14. Leeuwenburgh I, Scholten P, Alderliesten J, et al. 2010; Long-term esophageal cancer risk in patients with primary achalasia: a prospective study. Am J Gastroenterol. 105:2144–2149. DOI: 10.1038/ajg.2010.263. PMID: 20588263.
Article15. Han SY, Youn YH. 2023; Role of endoscopy in patients with achalasia. Clin Endosc. 56:537–545. DOI: 10.5946/ce.2023.001. PMID: 37430397. PMCID: PMC10565433.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Role of endoscopy in patients with achalasia
- A Case of Esophageal Carcinoma Following Esophagomyotomy for Achalasia
- Endoscopic Treatment of Primary Esophageal Motility Disorders
- Peroral Endoscopic Myotomy for Esophageal Motility Disorders
- Non-achalasia esophageal motility disorders: Role of per-oral endoscopic myotomy