Clin Endosc.
2023 Sep;56(5):537-545. 10.5946/ce.2023.001.
Role of endoscopy in patients with achalasia
- Affiliations
-
- 1Department of Internal Medicine, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2546131
- DOI: http://doi.org/10.5946/ce.2023.001
Abstract
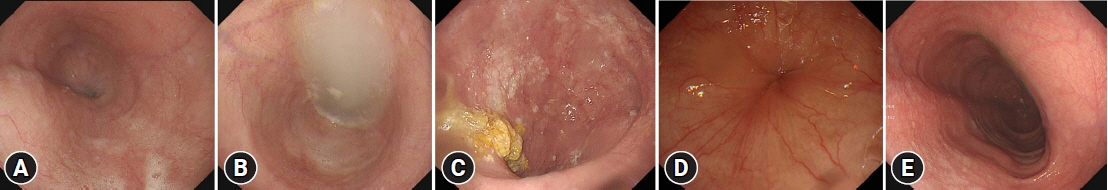
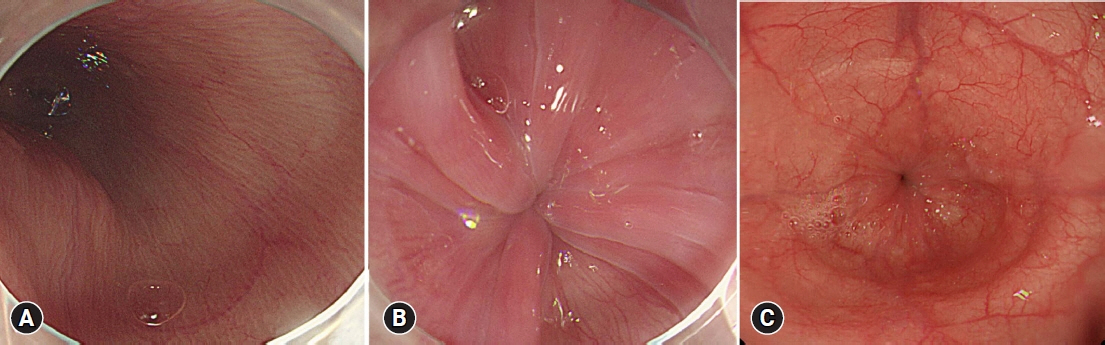
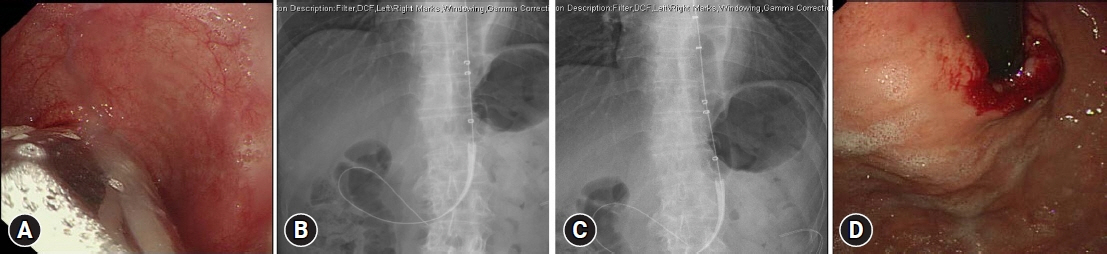
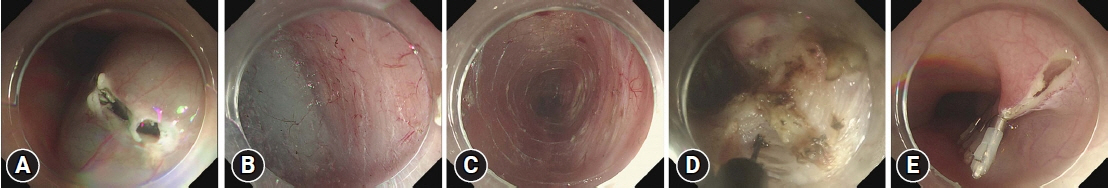
- Achalasia is an esophageal motility disorder characterized by impaired lower esophageal sphincter relaxation and peristalsis of the esophageal body. With the increasing prevalence of achalasia, interest in the role of endoscopy in its diagnosis, treatment, and monitoring is also growing. The major diagnostic modalities for achalasia include high-resolution manometry, esophagogastroduodenoscopy, and barium esophagography. Endoscopic assessment is important for early diagnosis to rule out diseases that mimic achalasia symptoms, such as pseudo-achalasia, esophageal cancer, esophageal webs, and eosinophilic esophagitis. The major endoscopic characteristics suggestive of achalasia include a widened esophageal lumen and food residue in the esophagus. Once diagnosed, achalasia can be treated either endoscopically or surgically. The preference for endoscopic treatment is increasing owing to its minimal invasiveness. Botulinum toxins, pneumatic balloon dilation, and peroral endoscopic myotomy (POEM) are important endoscopic treatments. Previous studies have demonstrated excellent treatment outcomes for POEM, with >95% improvement in dysphagia, making POEM the mainstay treatment option for achalasia. Several studies have reported an increased risk of esophageal cancer in patients with achalasia. However, routine endoscopic surveillance remains controversial owing to the lack of sufficient data. Further studies on surveillance methods and duration are warranted to establish concordant guidelines for the endoscopic surveillance of achalasia.
Keyword
Figure
Cited by 1 articles
-
식도이완불능증과 동반된 표재성 식도암의 동시 내시경 치료 증례
Myung-Hun Lee, Kyoungwon Jung, Jae Hyun Kim, Sung Eun Kim, Won Moon, Moo In Park, Seun Ja Park
Korean J Gastroenterol. 2023;82(5):248-253. doi: 10.4166/kjg.2023.099.
Reference
-
1. Pomenti S, Blackett JW, Jodorkovsky D. Achalasia: diagnosis, management and surveillance. Gastroenterol Clin North Am. 2021; 50:721–736.2. Pohl D, Tutuian R. Achalasia: an overview of diagnosis and treatment. J Gastrointestin Liver Dis. 2007; 16:297–303.3. Vaezi MF, Pandolfino JE, Yadlapati RH, et al. ACG clinical guidelines: diagnosis and management of achalasia. Am J Gastroenterol. 2020; 115:1393–1411.4. O'Neill OM, Johnston BT, Coleman HG. Achalasia: a review of clinical diagnosis, epidemiology, treatment and outcomes. World J Gastroenterol. 2013; 19:5806–5812.5. Park W, Vaezi MF. Etiology and pathogenesis of achalasia: the current understanding. Am J Gastroenterol. 2005; 100:1404–1414.6. Sadowski DC, Ackah F, Jiang B, et al. Achalasia: incidence, prevalence and survival. A population-based study. Neurogastroenterol Motil. 2010; 22:e256–e261.7. Kim E, Lee H, Jung HK, et al. Achalasia in Korea: an epidemiologic study using a national healthcare database. J Korean Med Sci. 2014; 29:576–580.8. Birgisson S, Richter JE. Achalasia in Iceland, 1952-2002: an epidemiologic study. Dig Dis Sci. 2007; 52:1855–1860.9. Samo S, Carlson DA, Gregory DL, et al. Incidence and prevalence of achalasia in central Chicago, 2004-2014, since the widespread use of high-resolution manometry. Clin Gastroenterol Hepatol. 2017; 15:366–373.10. Su B, Callahan ZM, Novak S, et al. Using impedance planimetry (EndoFLIP) to evaluate myotomy and predict outcomes after surgery for achalasia. J Gastrointest Surg. 2020; 24:964–971.11. Mari A, Abu Baker F, Pellicano R, et al. Diagnosis and management of achalasia: updates of the last two years. J Clin Med. 2021; 10:3607.12. Gockel I, Eckardt VF, Schmitt T, et al. Pseudoachalasia: a case series and analysis of the literature. Scand J Gastroenterol. 2005; 40:378–385.13. Desai TK, Stecevic V, Chang CH, et al. Association of eosinophilic inflammation with esophageal food impaction in adults. Gastrointest Endosc. 2005; 61:795–801.14. Potter JW, Saeian K, Staff D, et al. Eosinophilic esophagitis in adults: an emerging problem with unique esophageal features. Gastrointest Endosc. 2004; 59:355–361.15. Mandaliya R, DiMarino AJ, Cohen S. Association of achalasia and eosinophilic esophagitis. Indian J Gastroenterol. 2013; 32:54–57.16. Schizas D, Syllaios A, Vailas M, et al. Eosinophilic esophagitis and achalasia: two distinct nosologic entities or a possible etiopathogenic association? Dig Dis. 2021; 39:553–560.17. Japan Esophageal Society. Descriptive rules for achalasia of the esophagus, June 2012: 4th edition. Esophagus. 2017; 14:275–289.18. Howard PJ, Maher L, Pryde A, et al. Five year prospective study of the incidence, clinical features, and diagnosis of achalasia in Edinburgh. Gut. 1992; 33:1011–1015.19. Minami H, Isomoto H, Miuma S, et al. New endoscopic indicator of esophageal achalasia: "pinstripe pattern". PLoS One. 2015; 10:e0101833.20. Iwakiri K, Hoshihara Y, Kawami N, et al. The appearance of rosette-like esophageal folds ("esophageal rosette") in the lower esophagus after a deep inspiration is a characteristic endoscopic finding of primary achalasia. J Gastroenterol. 2010; 45:422–425.21. Gomi K, Inoue H, Ikeda H, et al. New endoscopic classification of the cardiac orifice in esophageal achalasia: champagne glass sign. Dig Endosc. 2016; 28:645–649.22. Payne WS. Heller's contribution to the surgical treatment of achalasia of the esophagus. 1914. Ann Thorac Surg. 1989; 48:876–881.23. Pasricha PJ, Ravich WJ, Kalloo AN, et al. Effects of intrasphincteric botulinum toxin on the lower esophageal sphincter in piglets. Gastroenterology. 1993; 105:1045–1049.24. Pasricha PJ, Ravich WJ, Hendrix TR, et al. Treatment of achalasia with intrasphincteric injection of botulinum toxin. A pilot trial. Ann Intern Med. 1994; 121:590–591.25. Pasricha PJ, Ravich WJ, Hendrix TR, et al. Intrasphincteric botulinum toxin for the treatment of achalasia. N Engl J Med. 1995; 332:774–778.26. Ramzan Z, Nassri AB. The role of botulinum toxin injection in the management of achalasia. Curr Opin Gastroenterol. 2013; 29:468–473.27. Neubrand M, Scheurlen C, Schepke M, et al. Long-term results and prognostic factors in the treatment of achalasia with botulinum toxin. Endoscopy. 2002; 34:519–523.28. Cuillière C, Ducrotté P, Zerbib F, et al. Achalasia: outcome of patients treated with intrasphincteric injection of botulinum toxin. Gut. 1997; 41:87–92.29. Kolbasnik J, Waterfall WE, Fachnie B, et al. Long-term efficacy of Botulinum toxin in classical achalasia: a prospective study. Am J Gastroenterol. 1999; 94:3434–3439.30. Richter JE, Boeckxstaens GE. Management of achalasia: surgery or pneumatic dilation. Gut. 2011; 60:869–876.31. van Hoeij FB, Prins LI, Smout AJ, et al. Efficacy and safety of pneumatic dilation in achalasia: a systematic review and meta-analysis. Neurogastroenterol Motil. 2019; 31:e13548.32. Mikaeli J, Bishehsari F, Montazeri G, et al. Pneumatic balloon dilatation in achalasia: a prospective comparison of safety and efficacy with different balloon diameters. Aliment Pharmacol Ther. 2004; 20:431–436.33. Boeckxstaens GE, Annese V, des Varannes SB, et al. Pneumatic dilation versus laparoscopic Heller's myotomy for idiopathic achalasia. N Engl J Med. 2011; 364:1807–1816.34. Hulselmans M, Vanuytsel T, Degreef T, et al. Long-term outcome of pneumatic dilation in the treatment of achalasia. Clin Gastroenterol Hepatol. 2010; 8:30–35.35. Vanuytsel T, Lerut T, Coosemans W, et al. Conservative management of esophageal perforations during pneumatic dilation for idiopathic esophageal achalasia. Clin Gastroenterol Hepatol. 2012; 10:142–149.36. Yamashita H, Ashida K, Fukuchi T, et al. Predictive factors associated with the success of pneumatic dilatation in Japanese patients with primary achalasia: a study using high-resolution manometry. Digestion. 2013; 87:23–28.37. Pratap N, Kalapala R, Darisetty S, et al. Achalasia cardia subtyping by high-resolution manometry predicts the therapeutic outcome of pneumatic balloon dilatation. J Neurogastroenterol Motil. 2011; 17:48–53.38. Eckardt VF, Aignherr C, Bernhard G. Predictors of outcome in patients with achalasia treated by pneumatic dilation. Gastroenterology. 1992; 103:1732–1738.39. Rohof WO, Salvador R, Annese V, et al. Outcomes of treatment for achalasia depend on manometric subtype. Gastroenterology. 2013; 144:718–725.40. Inoue H, Minami H, Kobayashi Y, et al. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy. 2010; 42:265–271.41. Youn YH, Minami H, Chiu PW, et al. Peroral endoscopic myotomy for treating achalasia and esophageal motility disorders. J Neurogastroenterol Motil. 2016; 22:14–24.42. Stavropoulos SN, Modayil R, Friedel D. Achalasia. Gastrointest Endosc Clin N Am. 2013; 23:53–75.43. Maselli R, Inoue H, Ikeda H, et al. Microvasculature of the esophagus and gastroesophageal junction: lesson learned from submucosal endoscopy. World J Gastrointest Endosc. 2016; 8:690–696.44. Grimes KL, Inoue H, Onimaru M, et al. Double-scope per oral endoscopic myotomy (POEM): a prospective randomized controlled trial. Surg Endosc. 2016; 30:1344–1351.45. Crespin OM, Liu LW, Parmar A, et al. Safety and efficacy of POEM for treatment of achalasia: a systematic review of the literature. Surg Endosc. 2017; 31:2187–2201.46. Lee JY, Lim CH, Kim DH, et al. Adverse events associated with peroral endoscopic myotomy affecting extended hospital stay: a multi-center retrospective study in South Korea. J Neurogastroenterol Motil. 2022; 28:247–254.47. Ren Z, Zhong Y, Zhou P, et al. Perioperative management and treatment for complications during and after peroral endoscopic myotomy (POEM) for esophageal achalasia (EA) (data from 119 cases). Surg Endosc. 2012; 26:3267–3272.48. Hungness ES, Sternbach JM, Teitelbaum EN, et al. Per-oral endoscopic myotomy (POEM) after the learning curve: durable long-term results with a low complication rate. Ann Surg. 2016; 264:508–517.49. Repici A, Fuccio L, Maselli R, et al. GERD after per-oral endoscopic myotomy as compared with Heller's myotomy with fundoplication: a systematic review with meta-analysis. Gastrointest Endosc. 2018; 87:934–943.50. Bapaye A, Dashatwar P, Dharamsi S, et al. Single-session endoscopic fundoplication after peroral endoscopic myotomy (POEM+F) for prevention of post gastroesophageal reflux: 1-year follow-up study. Endoscopy. 2021; 53:1114–1121.51. Inoue H, Ueno A, Shimamura Y, et al. Peroral endoscopic myotomy and fundoplication: a novel NOTES procedure. Endoscopy. 2019; 51:161–164.52. Li QL, Wu QN, Zhang XC, et al. Outcomes of per-oral endoscopic myotomy for treatment of esophageal achalasia with a median follow-up of 49 months. Gastrointest Endosc. 2018; 87:1405–1412.53. Brewer Gutierrez OI, Moran RA, Familiari P, et al. Long-term outcomes of per-oral endoscopic myotomy in achalasia patients with a minimum follow-up of 4 years: a multicenter study. Endosc Int Open. 2020; 8:E650–E655.54. Nabi Z, Ramchandani M, Darisetty S, et al. Impact of prior treatment on long-term outcome of peroral endoscopic myotomy in pediatric achalasia. J Pediatr Surg. 2020; 55:1552–1555.55. Xu S, Chai N, Tang X, et al. Outcomes of peroral endoscopic myotomy in challenging achalasia patients: a long-term follow-up study. Surg Endosc. 2021; 35:3732–3743.56. Podboy AJ, Hwang JH, Rivas H, et al. Long-term outcomes of per-oral endoscopic myotomy compared to laparoscopic Heller myotomy for achalasia: a single-center experience. Surg Endosc. 2021; 35:792–801.57. Shiwaku H, Inoue H, Onimaru M, et al. Multicenter collaborative retrospective evaluation of peroral endoscopic myotomy for esophageal achalasia: analysis of data from more than 1300 patients at eight facilities in Japan. Surg Endosc. 2020; 34:464–468.58. Ponds FA, Fockens P, Lei A, et al. Effect of peroral endoscopic myotomy vs pneumatic dilation on symptom severity and treatment outcomes among treatment-naïve patients with achalasia: a randomized clinical trial. JAMA. 2019; 322:134–144.59. Schlottmann F, Luckett DJ, Fine J, et al. Laparoscopic Heller myotomy versus peroral endoscopic myotomy (POEM) for achalasia: a systematic review and meta-analysis. Ann Surg. 2018; 267:451–460.60. Kumbhari V, Tieu AH, Onimaru M, et al. Peroral endoscopic myotomy (POEM) vs laparoscopic Heller myotomy (LHM) for the treatment of Type III achalasia in 75 patients: a multicenter comparative study. Endosc Int Open. 2015; 3:E195–E201.61. Eckardt AJ, Eckardt VF. Editorial: cancer surveillance in achalasia. Better late than never? Am J Gastroenterol. 2010; 105:2150–2152.62. Leeuwenburgh I, Scholten P, Alderliesten J, et al. Long-term esophageal cancer risk in patients with primary achalasia: a prospective study. Am J Gastroenterol. 2010; 105:2144–2149.63. Sandler RS, Nyrén O, Ekbom A, et al. The risk of esophageal cancer in patients with achalasia. A population-based study. JAMA. 1995; 274:1359–1362.64. Zendehdel K, Nyrén O, Edberg A, et al. Risk of esophageal adenocarcinoma in achalasia patients, a retrospective cohort study in Sweden. Am J Gastroenterol. 2011; 106:57–61.65. Leeuwenburgh I, Scholten P, Caljé TJ, et al. Barrett's esophagus and esophageal adenocarcinoma are common after treatment for achalasia. Dig Dis Sci. 2013; 58:244–252.66. Ide E, Carneiro FO, Frazão MS, et al. Endoscopic detection of early esophageal squamous cell carcinoma in patients with achalasia: narrow-band imaging versus Lugol's staining. J Oncol. 2013; 2013:736756.67. Ponds FA, Moonen A, Smout AJ, et al. Screening for dysplasia with Lugol chromoendoscopy in longstanding idiopathic achalasia. Am J Gastroenterol. 2018; 113:855–862.